Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (4): 646-650. doi: 10.19723/j.issn.1671-167X.2020.04.009
Previous Articles Next Articles
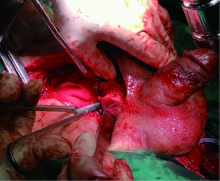
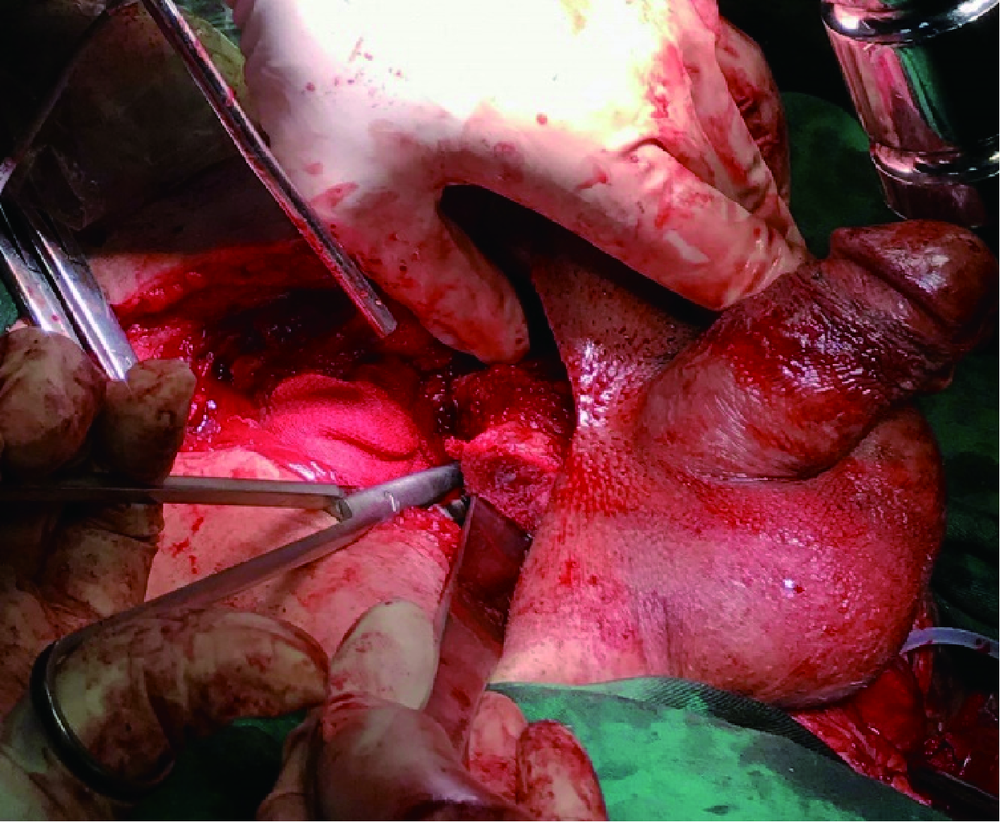
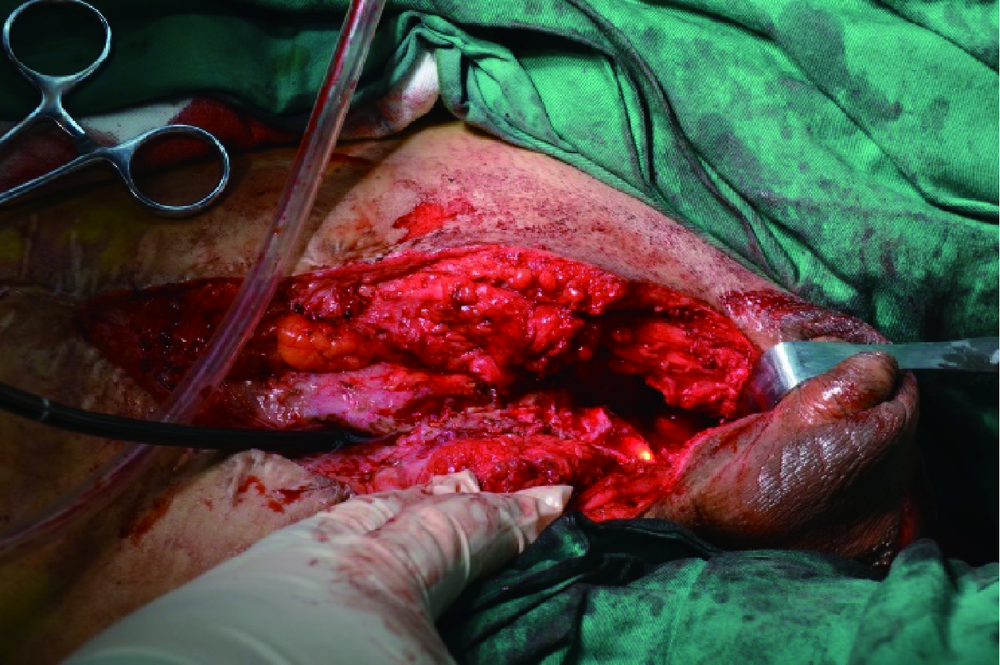
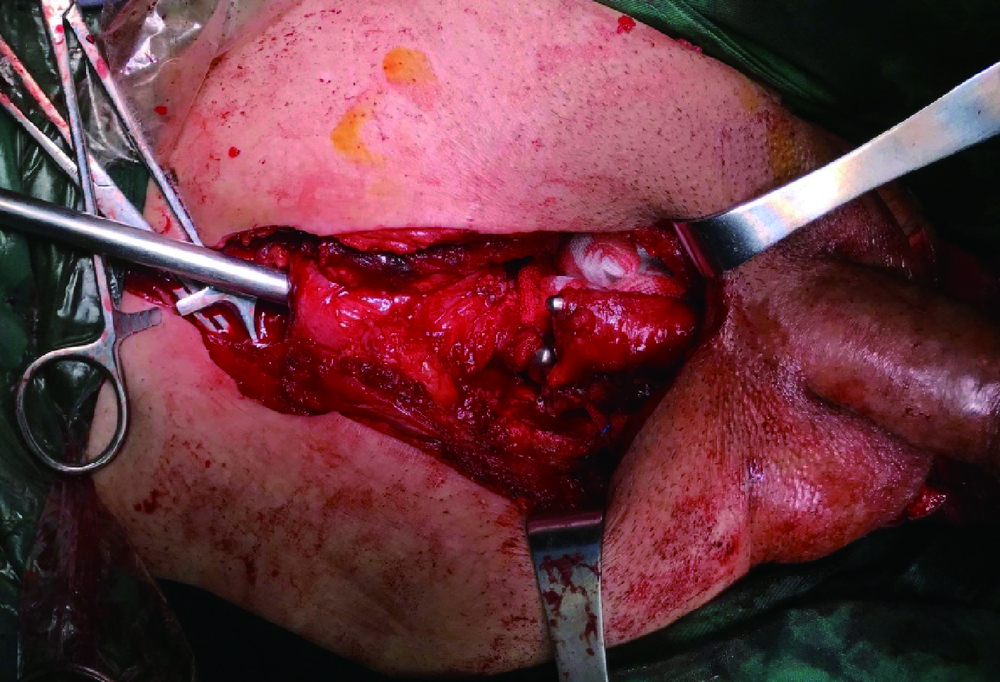
Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect
Jian-wei WANG,Li-bo MAN( ),Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI
),Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI
- Department of Urology, Beijing Jishuitan Hospital, the Fourth Medical College of Peking University, Beijing 100096, China
CLC Number:
- R699.6
| [1] | 满立波, 王建伟. 图解尿道成形术 [M]. 北京: 人民卫生出版社, 2018: 43-51. |
| [2] | 王建伟, 满立波, 黄广林, 等. 经会阴三步法手术策略治疗单纯性男性骨盆骨折后尿道离断[J]. 北京大学学报(医学版), 2018,50(4):617-620. |
| [3] |
Gelman J. Tips for successful open surgical reconstruction of posterior urethral disruption injuries[J]. Urol Clin North Am, 2013,40(3):381-392.
doi: 10.1016/j.ucl.2013.04.007 pmid: 23905936 |
| [4] |
Barratt RC, Bernard J, Mundy AR, et al. Pelvic fracture urethral injury in males—mechanisms of injury, management options and outcomes[J]. Transl Androl Urol, 2018,7(Suppl 1):S29-S62.
pmid: 29644168 |
| [5] |
Koraitim MM. Predictors of surgical approach to repair pelvic fracture urethral distraction defects[J]. J Urol, 2009,182(4):1435-1439.
pmid: 19683294 |
| [6] | Horiguchi A. Management of male pelvic fracture urethral injuries: review and current topics[J]. Int J Urol, 2019,26(6):596-607. |
| [7] |
Pierce JM Jr. Exposure of the membranous and posterior urethra by total pubectomy[J]. J Urol, 1962,88:256-258.
pmid: 14486460 |
| [8] |
Koraitim MM. The combined perineo-abdominal transpubic urehtroplasty[J]. Arab J Urol, 2015,13(1):24-26.
pmid: 26019974 |
| [9] | Koraitim MM. Optimising the outcome after anastomotic posterior urethroplasty[J]. Arab J Urol, 2015,13(1):27-31. |
| [10] | Horiguchi A, Edo H, Soga S, et al. Pubourethral stump angle measured on preoperative magnetic resonance imaging predicts urethroplasty type for pelvic fracture urethral injury repair[J]. Urology, 2018,112:198-204. |
| [11] | Barbagli G. History and evolution of transpubic urethroplasty: a lesson for young urologists in training[J]. Eur Urol, 2009,52(5):1290-1292. |
| [12] | Johnsen NV, Moses RA, Ellliott SP, et al. Multicenter analysis of posterior urethroplasty complexity and outcomes following pelvic fracture urethral injury[J]. World J Urol, 2019,38(4):1073-1079. |
| [13] |
Angulo JC, Gómez RG, Nikolavsky D. Reconstruction of membranous urethral strictures[J]. Curr Urol Rep, 2018,19(6):37.
pmid: 29644478 |
| [14] | Mathur RK, Tiwari NS, Odiya SA. Transpubic urethroplasty: a single center experience[J]. Adv Urol, 2014,2014:826710. doi: 10.1155/2014/826710. |
| [15] | Koraitim MM. Complex pelvic fracture urethral distraction defects revisited[J]. Scand J Urol, 2014,48(1):84-89. |
| [16] | Podesta M, Podesta M Jr. Delayed surgical repair of posttraumatic posterior urethral distraction defects in children and adolesents: long-term results [J]. J Pediatr Urol, 2015, 11(2): 67.e1-6. |
| [17] |
Joshi PM, Batra V, Kulkarni SB. Controversies in the management of pelvic fracture urethral distraction defects[J]. Turk J Urol, 2019,45(1):1-6.
pmid: 30668305 |
| [18] |
Kulkarni SB, Surana S, Desai DJ, et al. Management of complex and redo cases of pelvic fracture urethral injuries[J]. Asian J Urol, 2018,5(2):107-117.
pmid: 29736373 |
| [19] |
Gomez RG, Mundy T, Dubey D, et al. SIU/ICUD consultation on urethral strictures: pelvic fracture urethral injuries[J]. Urology, 2014,83(3 Suppl):S48-S58.
doi: 10.1016/j.urology.2013.09.023 pmid: 24210734 |
| [20] |
Pratap A, Agrawal CS, Pandit RK, et al. Factors contributing to a successful outcome of combined abdominal transpubic perineal urethroplasty for complex posterior urethral disruptions[J]. J Urol, 2006,176(6 Pt 1):2514-2517.
pmid: 17085145 |
| [1] | WANG Jian-wei,XU Xiao,BAO Zheng-qing,LIU Zhen-hua,HE Feng,HUANG Guang-lin,MAN Li-bo. Outcomes of partial pubectomy assisted anastomotic urethroplasty for male patients with pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 798-802. |
| [2] | WANG Jian-wei, MAN Li-bo, HUANG Guang-lin, WANG Hai, Xu Xiao, ZHU Xiao-fei, LI Wei, LIU Zhen-hua. “3-step” strategy of transperineal anastomotic urethroplasty for the simple pelvic fracture urethral distraction defect in male patients [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 617-620. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 266
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 1295
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||