Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 798-802. doi: 10.19723/j.issn.1671-167X.2021.04.030
Previous Articles Next Articles
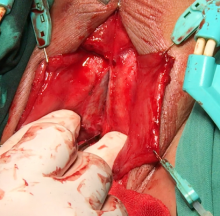
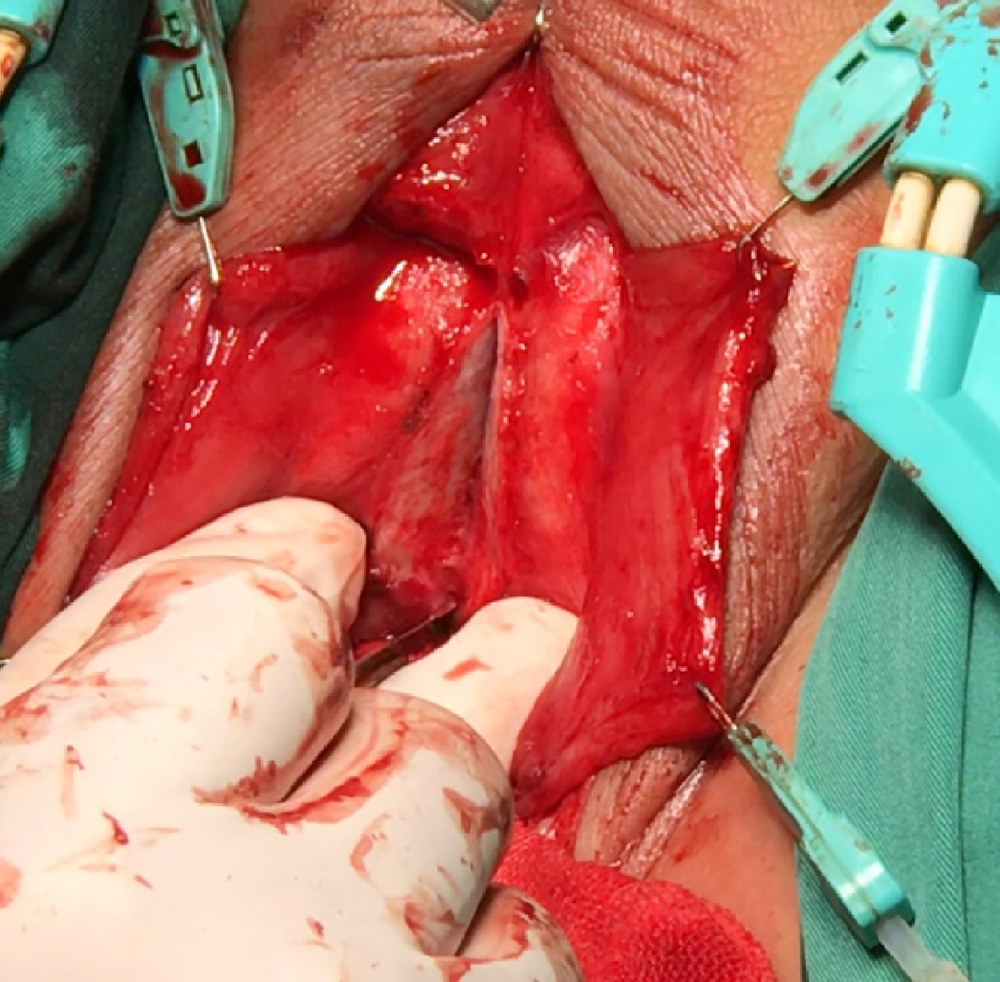
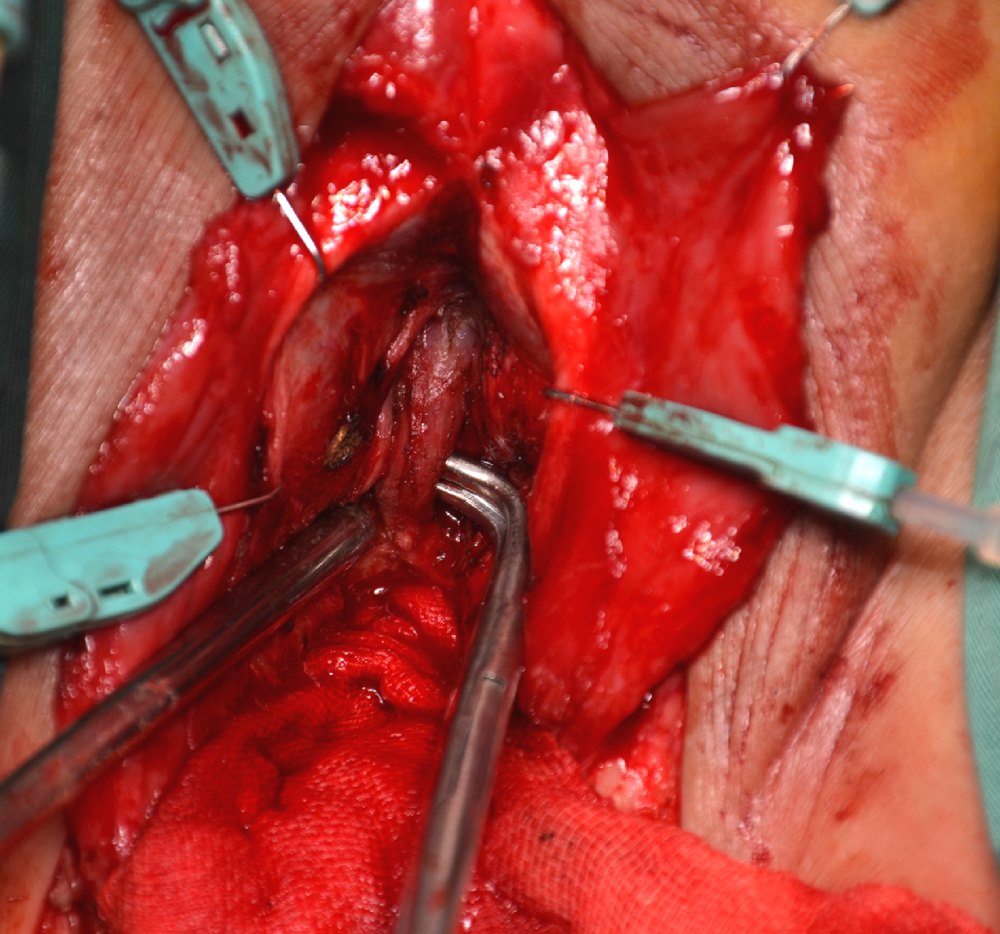
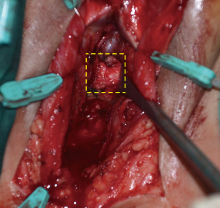
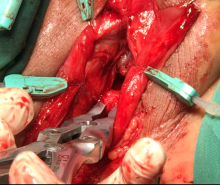
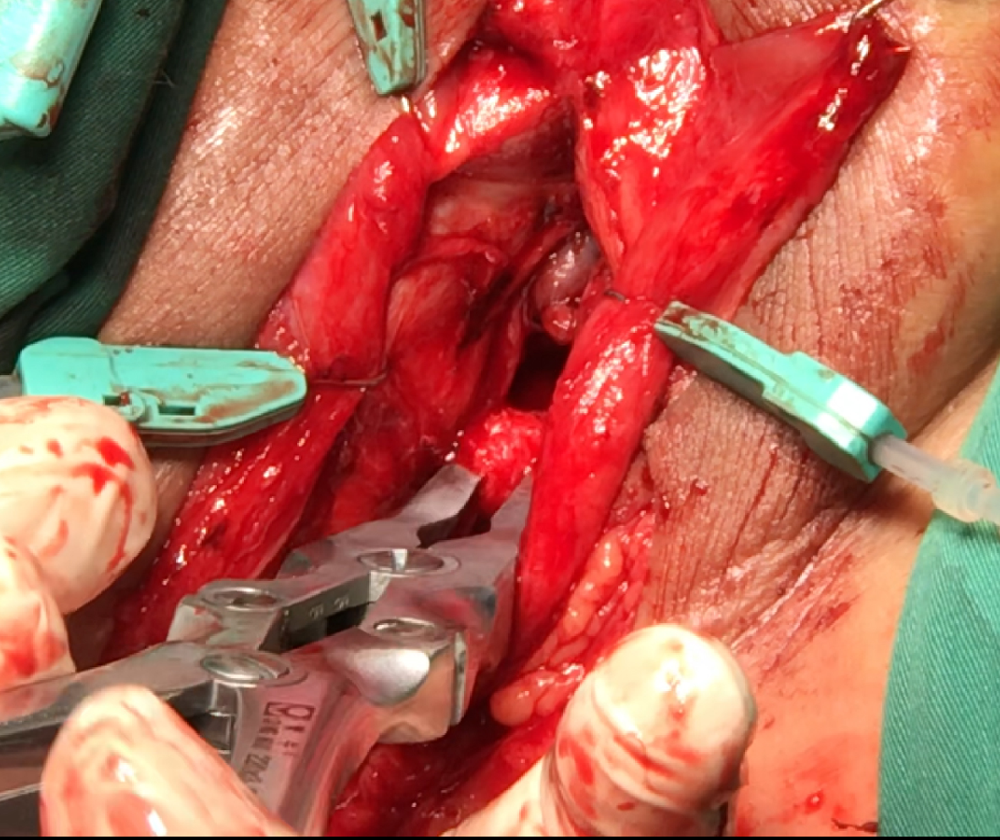
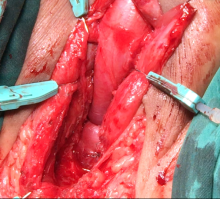
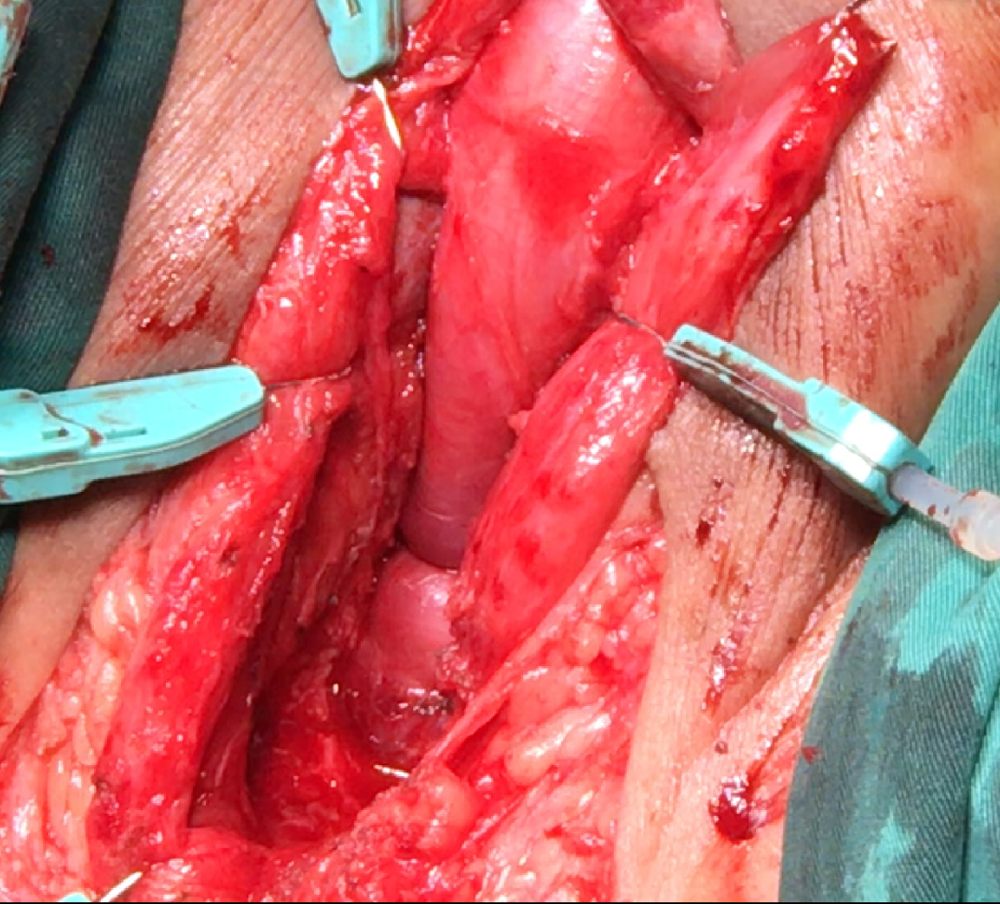
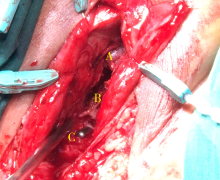
Outcomes of partial pubectomy assisted anastomotic urethroplasty for male patients with pelvic fracture urethral distraction defect
WANG Jian-wei,XU Xiao,BAO Zheng-qing,LIU Zhen-hua,HE Feng,HUANG Guang-lin,MAN Li-bo( )
)
- Department of Urology, Beijing Jishuitan Hospital, the Fourth Medical College of Peking University, Beijing 100096, China
CLC Number:
- R699.6
| [1] |
Xu YM, Song LJ, Wang KI, et al. Changing trends in the causes and management of male urethral stricture disease in China: An observational descriptive study from 13 centers [J]. BJU Int, 2015, 116(6):938-944.
doi: 10.1111/bju.12945 |
| [2] | 满立波, 王建伟. 图解尿道成形术[M]. 北京: 人民卫生出版社, 2018: 43-49. |
| [3] | Joshi PM, Batra V, Kulkarni SB. Controversies in the management of pelvic fracture urethral distraction defects [J]. Turk J Urol, 2019, 45(1):1-6. |
| [4] |
Horiguchi A. Management of male pelvic fracture urethral injuries: review and current topics [J]. Int J Urol, 2019, 26(6):596-607.
doi: 10.1111/iju.13947 pmid: 30895658 |
| [5] |
Wessells H, Angermeier KW, Elliott S, et al. Male urethral stricture: American Urological Association guideline [J]. J Urol, 2017, 197(1):182-190.
doi: S0022-5347(16)30961-2 pmid: 27497791 |
| [6] |
Horiguchi A, Shinchi M, Masunaga A, et al. Do transurethral treatment increase the complexity of urethral stricture? [J]. J Urol, 2018, 199(2):508-514.
doi: S0022-5347(17)77417-4 pmid: 28866464 |
| [7] |
Koraitim MM. Optimising the outcome after anastomotic posterior urethroplasty [J]. Arab J Urol, 2015, 13(1):27-31.
doi: 10.1016/j.aju.2014.12.006 |
| [8] |
Andrich DE, Malley KJO, Summerton DJ, et al. The type of urethroplasty for pelvic fracture urethral distraction defect cannot be predicted preoperatively [J]. J Urol, 2003, 170(2 Pt 1):464-467.
doi: 10.1097/01.ju.0000076752.32199.40 |
| [9] |
Horiguchi A, Edo H, Soga S, et al. Pubourethral stump angle measured on preoperative magnetic resonance imaging predeicts urethroplasty type for pelvic fracture injury repair [J]. Urology, 2018, 112:198-204.
doi: S0090-4295(17)31199-8 pmid: 29158171 |
| [10] | Joshi PM, Desai DJ, Shah D, et al. Magnetic resonance imaging procedure for pelvic fracture urethral injuries and recto urethral fistulas: A simple protocaol [J]. Turk J Urol, 2021, 47(1):35-42. |
| [11] |
Yin L, Li Z, Kong C, et al. Urethral pull-through operation for the management of pelvic fracture urethral distraction defects [J]. Urology, 2011, 78(4):946-950.
doi: 10.1016/j.urology.2011.05.027 |
| [12] |
Kulkarni SB, Joshi PM, Hunter C, et al. Complex posterior urethral injury [J]. Arab J Urol, 2015, 13(1):43-52.
doi: 10.1016/j.aju.2014.11.008 |
| [13] | 王建伟, 满立波, 徐啸, 等. 耻骨会阴联合切口后尿道吻合术治疗复杂男性骨盆骨折后尿道离断 [J]. 北京大学学报(医学版), 2020, 52(4):646-650. |
| [14] | 王建伟, 满立波, 黄广林, 等. 经会阴三步法手术策略治疗单纯性男性骨盆骨折后尿道离断 [J]. 北京大学学报(医学版), 2018, 50(4):617-620. |
| [15] |
Saini DK, Sinha RJ, Solhal AK, et al. Analysis of anastomotic urethroplasty for pelvic fracture urethral distraction defect: Decadal experience from a high-volume tertiary care center [J]. Urol Ann, 2019, 11(1):77-82.
doi: 10.4103/UA.UA_48_17 |
| [16] |
Webster GD, Peterson AC. Simple perineal and elaborated peri-neal posterior urethroplasty [J]. Arab J Urol, 2015, 13(1):17-23.
doi: 10.1016/j.aju.2015.01.002 |
| [17] |
Johnsen NV, Moses RA, Elliott SP, et al. Multicenter analysis of posterior urethroplasty complexity and outcomes following pelvic fracture urethral injury [J]. World J Urol, 2020, 38(4):1073-1079.
doi: 10.1007/s00345-019-02824-5 pmid: 31144093 |
| [18] | Ríosa E, Martínez-Piñeirob L. Treatment of posterior urethral distractions defects following pelvic fracture [J]. Asian J Urol, 2018, 5(3):164-171. |
| [1] | Jian-wei WANG,Li-bo MAN,Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI. Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 646-650. |
| [2] | Jian-wei WANG,Li-bo MAN,Guang-lin HUANG,Feng HE,Hai WANG,Hai-dong WANG,Xiao XU,Wei LI,Jian-po ZHAI,Zhen-hua LIU. Single-stage repair of penile urethral stricture using combined dorsal onlay oral mucosa grafting with ventral onlay penile skin flap [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 641-645. |
| [3] | WANG Jian-wei, MAN Li-bo, HUANG Guang-lin, WANG Hai, Xu Xiao, ZHU Xiao-fei, LI Wei, LIU Zhen-hua. “3-step” strategy of transperineal anastomotic urethroplasty for the simple pelvic fracture urethral distraction defect in male patients [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 617-620. |
| [4] | XIE Tian-Peng, HUANG Xiao-Bo, XU Qing-Quan, YE Hai-Yun, YANG Qing-Ya, WANG Xiao-Feng. Balloon dilation by B ultrasound monitoring for treatment of urethral stricture: 5 case reports [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 657-658. |
| [5] | HUANG Guang-Lin, MAN Li-Bo, WANG Hai, WANG Jian-Wei, DI Jian-Po, ZHU Xiao-Fei, ZHOU Ning, XU Xiao. Management of female urethral obliteration with the rotary excision appliance [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 574-577. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 476
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 859
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||