Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (1): 69-75. doi: 10.19723/j.issn.1671-167X.2021.01.011
Previous Articles Next Articles
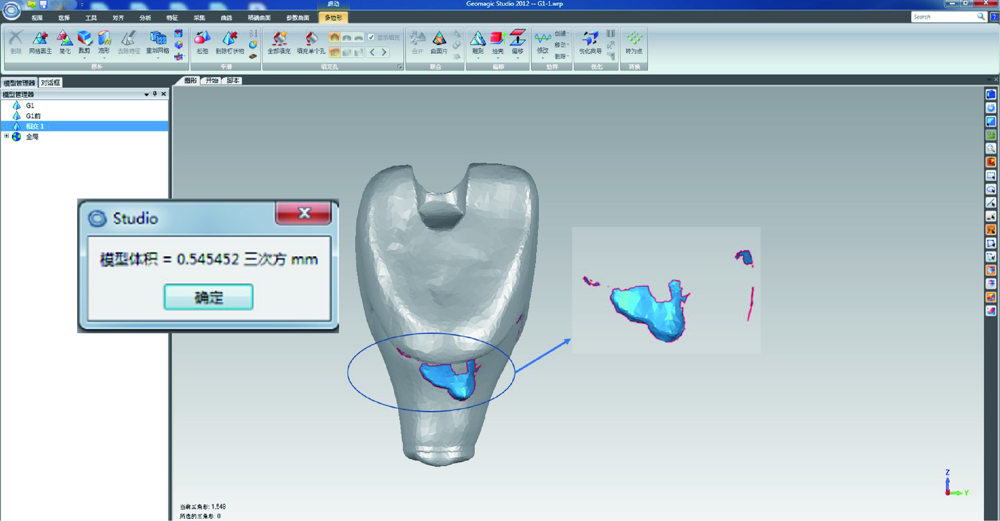
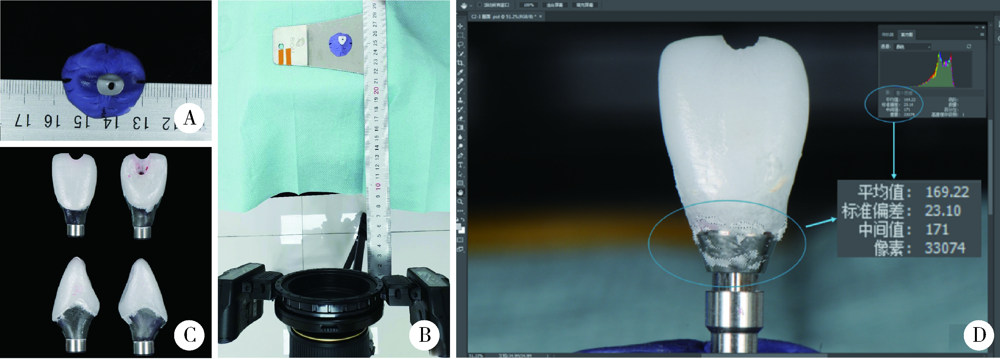
Comparison of residual cement between CAD/CAM customized abutments and stock abutments via digital measurement in vitro
YUE Zhao-guo1,ZHANG Hai-dong1,YANG Jing-wen2,HOU Jian-xia1,Δ( )
)
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Prosthetics, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R783
| [1] |
Jung RE, Pjetursson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns[J]. Clin Oral Implants Res, 2008,19(2):119-130.
doi: 10.1111/j.1600-0501.2007.01453.x pmid: 18067597 |
| [2] |
Chee W, Felton DA, Johnson PF, et al. Cemented versus screw-retained implant prostheses: Which is better?[J]. Int J Oral Maxillofac Implants, 1999,14(1):137-141.
pmid: 10074764 |
| [3] |
Linkevicius T, Vindasiute E, Puisys A, et al. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations[J]. Clin Oral Implants Res, 2011,22(12):1379-1384.
doi: 10.1111/j.1600-0501.2010.02119.x pmid: 21382089 |
| [4] |
Staubli N, Walter C, Schmidt JC, et al. Excess cement and the risk of peri-implant disease: A systematic review[J]. Clin Oral Implants Res, 2017,28(10):1278-1290.
doi: 10.1111/clr.12954 pmid: 27647536 |
| [5] |
Korsch M, Obst U, Walther W. Cement-associated peri-implantitis: A retrospective clinical observational study of fixed implant-supported restorations using a methacrylate cement[J]. Clin Oral Implants Res, 2014,25(7):797-802.
doi: 10.1111/clr.12173 pmid: 23600620 |
| [6] |
Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: A prospective clinical endoscopic study[J]. J Periodontol, 2009,80(9):1388-1392.
doi: 10.1902/jop.2009.090115 pmid: 19722787 |
| [7] |
Linkevicius T, Puisys A, Vindasiute E, et al. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis[J]. Clin Oral Implants Res, 2013,24(11):1179-1184.
doi: 10.1111/j.1600-0501.2012.02570.x pmid: 22882700 |
| [8] |
Ichikawa T, Ishida O, Watanabe M, et al. A new retrieval system for cement-retained implant superstructures: A technical report[J]. J Prosthodont, 2008,17(6):487-489.
doi: 10.1111/j.1532-849X.2008.00329.x pmid: 18544129 |
| [9] |
Galván G, Kois JC, Chaiyabutr Y, et al. Cemented implant restoration: A technique for minimizing adverse biologic consequences[J]. J Prosthet Dent, 2015,114(4):482-485.
doi: 10.1016/j.prosdent.2014.10.017 pmid: 26119018 |
| [10] |
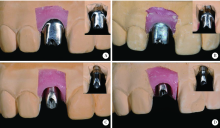
Seo CW, Seo JM. A technique for minimizing subgingival residual cement by using rubber dam for cement-retained implant crowns[J]. J Prosthet Dent, 2017,117(2):327-328.
doi: 10.1016/j.prosdent.2016.08.024 pmid: 27771147 |
| [11] | Linkevicius T. Zero bone loss concepts [M]. Illinois: Quintessence Publishing Co, 2019. |
| [12] |
Lewis S, Beumer J 3rd, Hornburg W, et al. The “UCLA” abutment[J]. Int J Oral Maxillofac Implants, 1988,3(3):183-189.
pmid: 3074050 |
| [13] | 戴文雍, 汤春波. 种植体修复个性化基台研究现状及展望[J]. 口腔医学, 2012,32(11):685-687. |
| [14] | 宿玉成. 口腔种植学[M]. 2版. 北京: 人民卫生出版社, 2014: 403-404. |
| [15] |
Shapoff CA, Lahey BJ. Crestal bone loss and the consequences of retained excess cement around dental implants[J]. Compend Contin Educ Dent, 2012,33(2):94-101.
pmid: 22545427 |
| [16] |
Schwarz F, Derks J, Monje A, et al. Peri-implantitis[J]. J Clin Periodontol, 2018,45(Suppl 20):S246-S266.
doi: 10.1111/jcpe.2018.45.issue-S20 |
| [17] |
Andersson B, Odman P, Lindvall AM, et al. Cemented single crowns on osseointegrated implants after 5 years: Results from a prospective study on CeraOne[J]. Int J Prosthodont, 1998,11(3):212-218.
pmid: 9728114 |
| [18] |
Linkevicius T, Vindasiute E, Puisys A, et al. The influence of the cementation margin position on the amount of undetected cement. A prospective clinical study[J]. Clin Oral Implants Res, 2013,24(1):71-76.
doi: 10.1111/j.1600-0501.2012.02453.x pmid: 22487018 |
| [19] |
Kappel S, Eiffler C, Lorenzo-Bermejo J, et al. Undetected resi-dual cement on standard or individualized all-ceramic abutments with cemented zirconia single crowns: A prospective randomized pilot trial[J]. Clin Oral Implants Res, 2016,27(9):1065-1071.
doi: 10.1111/clr.12691 pmid: 26381392 |
| [20] |
Kotsakis GA, Zhang L, Gaillard P, et al. Investigation of the association between cement retention and prevalent peri-implant diseases: A cross-sectional study[J]. J Periodontol, 2016,87(3):212-220.
doi: 10.1902/jop.2015.150450 pmid: 26537368 |
| [21] |
Daubert DM, Weinstein BF, Bordin S, et al. Prevalence and predictive factors for peri-implant disease and implant failure: A cross-sectional analysis[J]. J Periodontol, 2015,86(3):337-347.
doi: 10.1902/jop.2014.140438 pmid: 25415249 |
| [22] | Fuchigami K, Munakata M, Kitazume T, et al. A diversity of peri-implant mucosal thickness by site[J]. Clin Oral Impl Res, 2017,28(2):171-176. |
| [23] | 张众, 孟焕新, 韩劼, 等. 软组织垂直厚度对牙周炎患者种植修复临床效果的影响[J]. 北京大学学报(医学版), 2020,52(2):332-338. |
| [24] |
Dumbrigue HB, Abanomi AA, Cheng LL. Techniques to minimize excess luting agent in cement-retained implant restorations[J]. J Prosthet Dent, 2002,87(1):112-114.
doi: 10.1067/mpr.2002.119418 pmid: 11807495 |
| [25] |
Vindasiute E, Puisys A, Maslova N, et al. Clinical factors influencing removal of the cement excess in implant-supported restorations[J]. Clin Implant Dent Relat Res, 2015,17(4):771-778.
doi: 10.1111/cid.12170 pmid: 24224895 |
| [26] |
Andersson B, Odman P, Lindvall AM, et al. Single-tooth restorations supported by osseointegrated implants: results and experiences from a prospective study after 2 to 3 years[J]. Int J Oral Maxillofac Implants, 1995,10(6):702-711.
pmid: 8530173 |
| [27] | Higginbottom F, Belser U, Jones JD, et al. Prosthetic management of implants in the esthetic zone[J]. Int J Oral Maxillofac Implants, 2004,19(Suppl.):62-72. |
| [28] |
Berglundh T, Lindhe J, Marinello C, et al. Soft tissue reaction to de novo plaque formation on implants and teeth. An experimental study in the dog[J]. Clin Oral Implants Res, 1992,3(1):1-8.
doi: 10.1034/j.1600-0501.1992.030101.x pmid: 1420721 |
| [29] | 高鹏程, 谢理哲, 严斌. 牙颌模型三维数字化技术及其在口腔正畸学中的应用进展[J]. 口腔生物医学, 2014,5(3):152-157. |
| [1] | Yuxuan TIAN,Mingjian RUAN,Yi LIU,Derun LI,Jingyun WU,Qi SHEN,Yu FAN,Jie JIN. Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 567-574. |
| [2] | Liang LYU,Mingjin ZHANG,Aonan WEN,Yijiao ZHAO,Yong WANG,Jing LI,Gengchen YANG,Dawei LIU. Preliminary evaluation of chin symmetry with three dimentional soft tissue spatial angle wireframe template [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 106-110. |
| [3] | Bochun MAO,Yajing TIAN,Xuedong WANG,Jing LI,Yanheng ZHOU. Soft and hard tissue changes of hyperdivergent class Ⅱ patients before and after orthodontic extraction treatment [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 111-119. |
| [4] | Xiaotong LING,Liuyang QU,Danni ZHENG,Jing YANG,Xuebing YAN,Denggao LIU,Yan GAO. Three-dimensional radiographic features of calcifying odontogenic cyst and calcifying epithelial odontogenic tumor [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 131-137. |
| [5] | Xinyu XU,Ling WU,Fengqi SONG,Zili LI,Yi ZHANG,Xiaojing LIU. Mandibular condyle localization in orthognathic surgery based on mandibular movement trajectory and its preliminary accuracy verification [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 57-65. |
| [6] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [7] | Yi LIU,Chang-wei YUAN,Jing-yun WU,Qi SHEN,Jiang-xi XIAO,Zheng ZHAO,Xiao-ying WANG,Xue-song LI,Zhi-song HE,Li-qun ZHOU. Diagnostic efficacy of prostate cancer using targeted biopsy with 6-core systematic biopsy for patients with PI-RADS 5 [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 812-817. |
| [8] | Chang-wei YUAN,De-run LI,Zhi-hua LI,Yi LIU,Gang-zhi SHAN,Xue-song LI,Li-qun ZHOU. Application of dynamic contrast enhanced status in multiparametric magnetic resonance imaging for prostatic cancer with PI-RADS 4 lesion [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 838-842. |
| [9] | Zhan-yi ZHANG,Fan ZHANG,Ye YAN,Cai-guang CAO,Chang-jian LI,Shao-hui DENG,Yue-hao SUN,Tian-liang HUANG,Yun-he GUAN,Nan LI,Min LU,Zhen-hua HU,Shu-dong ZHANG. Near-infrared targeted probe designed for intraoperative imaging of prostatic neurovascular bundles [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 843-850. |
| [10] | Zhuo-hua LIN,Ru-yi CAI,Yang SUN,Rong MU,Li-gang CUI. Methodology and clinical use of superb microvascular imaging in assessing micro-circulation changes of fingertips in systemic sclerosis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 636-640. |
| [11] | Ying LIU,Ran HUO,Hui-min XU,Zheng WANG,Tao WANG,Hui-shu YUAN. Correlations between plaque characteristics and cerebral blood flow in patients with moderate to severe carotid stenosis using magnetic resonance vessel wall imaging [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 646-651. |
| [12] | Qiang FU,Guan-ying GAO,Yan XU,Zhuo-hua LIN,You-jing SUN,Li-gang CUI. Comparative study of ultrasound and magnetic resonance imaging in the diagnosis of asymptomatic anterosuperior acetabular labrum tears [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 665-669. |
| [13] | Xiang LIU,Hui-hui XIE,Yu-feng XU,Xiao-dong ZHANG,Xiao-feng TAO,Lin LIU,Xiao-ying WANG. Value of artificial intelligence in the improvement of diagnostic consistency of radiology residents [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 670-675. |
| [14] | Wen ZHANG,Xiao-jing LIU,Zi-li LI,Yi ZHANG. Effect of alar base cinch suture based on anatomic landmarks on the morphology of nasolabial region in patients after orthognathic surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 736-742. |
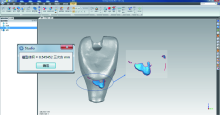
| [15] | Meng-en OU,Yun DING,Wei-feng TANG,Yong-sheng ZHOU. Three-dimensional finite element analysis of cement flow in abutment margin-crown platform switching [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 548-552. |
|
||