Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (1): 57-65. doi: 10.19723/j.issn.1671-167X.2024.01.010
Previous Articles Next Articles
Mandibular condyle localization in orthognathic surgery based on mandibular movement trajectory and its preliminary accuracy verification
Xinyu XU,Ling WU,Fengqi SONG,Zili LI,Yi ZHANG,Xiaojing LIU*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.2
| 1 |
Apostolakis D , Michelinakis G , Kamposiora P , et al. The current state of computer assisted orthognathic surgery: A narrative review[J]. J Dent, 2022, 119, 104052.
doi: 10.1016/j.jdent.2022.104052 |
| 2 |
Ho CT , Lin HH , Liou EJ , et al. Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: A qualitative and quantitative study[J]. Sci Rep, 2017, 7, 40423.
doi: 10.1038/srep40423 |
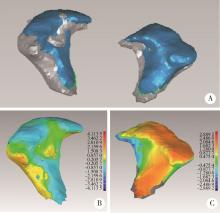
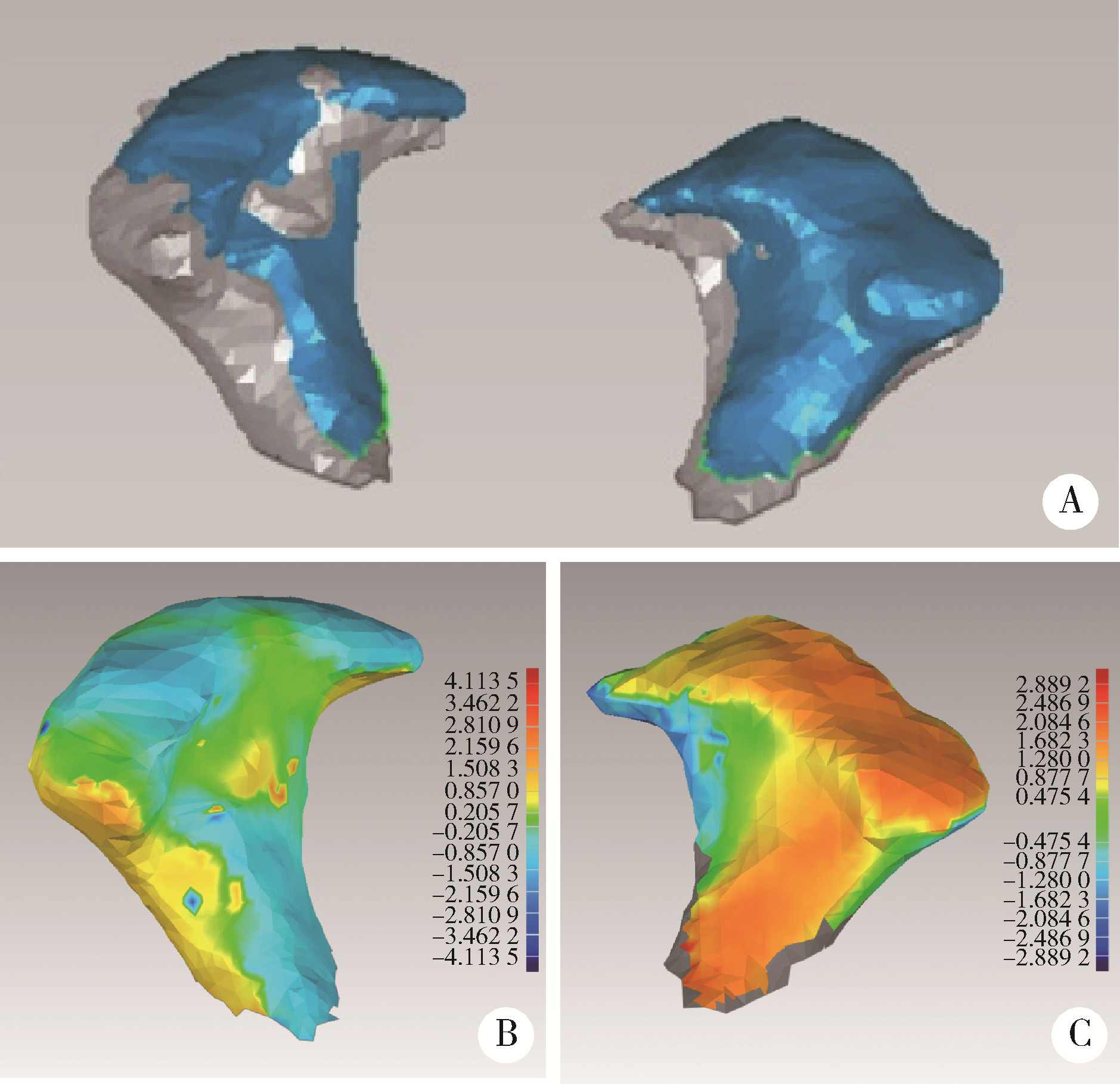
| 3 | 黄俊强, 黄臻, 伍军, 等. 骨性Ⅲ类错牙合伴下颌偏斜患者下颌支矢状劈开截骨术前后髁突位置的锥形束CT分析[J]. 中华口腔医学杂志, 2019, 54 (10): 649- 655. |
| 4 |
Nunes de Lima V , Faverani LP , Santiago JF Jr , et al. Evaluation of condylar resorption rates after orthognathic surgery in class Ⅱ and Ⅲ dentofacial deformities: A systematic review[J]. J Craniomaxillofac Surg, 2018, 46 (4): 668- 673.
doi: 10.1016/j.jcms.2018.02.002 |
| 5 |
Pachnicz D , Ramos A . Mandibular condyle displacements after orthognathic surgery: An overview of quantitative studies[J]. Quant Imag Med Surg, 2021, 11 (4): 1628- 1650.
doi: 10.21037/qims-20-677 |
| 6 |
Mozzo P , Procacci C , Tacconi A , et al. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results[J]. Eur Radiol, 1998, 8 (9): 1558- 1564.
doi: 10.1007/s003300050586 |
| 7 |
Wu TY , Lin HH , Lo LJ , et al. Postoperative outcomes of two- and three-dimensional planning in orthognathic surgery: A compa-rative study[J]. J Plast Reconstr Aesthet Surg, 2017, 70 (8): 1101- 1111.
doi: 10.1016/j.bjps.2017.04.012 |
| 8 |
Adolphs N , Haberl EJ , Liu W , et al. Virtual planning for craniomaxillofacial surgery: 7 years of experience[J]. J Craniomaxillofac Surg, 2014, 42 (5): e289- e295.
doi: 10.1016/j.jcms.2013.10.008 |
| 9 |
Kim DS , Choi SC , Lee SS , et al. Principal direction of inertia for 3D trajectories from patient-specific TMJ movement[J]. Comput Biol Med, 2013, 43 (3): 169- 175.
doi: 10.1016/j.compbiomed.2012.12.007 |
| 10 |
Zhang L , Shen L , Zhang L , et al. Dynamic 3D images fusion of the temporomandibular joints: A novel technique[J]. J Dent, 2022, 126, 104286.
doi: 10.1016/j.jdent.2022.104286 |
| 11 |
李源, 刘木清, 刘博, 等. 基于锥形束CT影像的颞下颌关节髁突骨改建三维定量评价研究[J]. 中华口腔医学杂志, 2020, 55 (9): 617- 623.
doi: 10.3760/cma.j.cn112144-20200507-00249 |
| 12 |
Tecco S , Saccucci M , Nucera R , et al. Condylar volume and surface in Caucasian young adult subjects[J]. BMC Med Imaging, 2010, 10, 28.
doi: 10.1186/1471-2342-10-28 |
| 13 | 侯磊, 叶国华, 刘筱菁, 等. 下颌后缩伴颞下颌关节重度骨关节病患者正颌术后颌骨稳定性及髁突体积变化的评价[J]. 北京大学学报(医学版), 2020, 52 (1): 113- 118. |
| 14 | Marlière DAA , Demétrio MS , Schmitt ARM , et al. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm and color maps: A retrospective cohort study[J]. Med Oral Patol Oral, 2019, 24 (2): E243- E253. |
| 15 | 陈硕, 刘筱菁, 李自力, 等. 下颌后缩畸形患者正颌外科术后髁突改建的三维影像评价[J]. 北京大学学报(医学版), 2015, 47 (4): 703- 707. |
| 16 |
Epker BN , Wylie GA . Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible[J]. Oral Surg Oral Med Oral Pathol, 1986, 62 (6): 613- 617.
doi: 10.1016/0030-4220(86)90251-3 |
| 17 | Barretto MDA , Melhem-Elias F , Deboni MCZ . Methods of mandibular condyle position and rotation center used for orthognathic surgery planning: A systematic review[J]. J Stomatol Oral Maxi, 2022, 123 (3): 345- 352. |
| 18 |
Costa F , Robiony M , Toro C , et al. Condylar positioning devices for orthognathic surgery: A literature review[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008, 106 (2): 179- 190.
doi: 10.1016/j.tripleo.2007.11.027 |
| 19 |
Jung GS , Kim TK , Lee JW , et al. The effect of a condylar repositioning plate on condylar position and relapse in two-jaw surgery[J]. Arch Plast Surg, 2017, 44 (1): 19- 25.
doi: 10.5999/aps.2017.44.1.19 |
| 20 |
Bethge LS , Ballon A , Mack M , et al. Intraoperative condyle positioning by sonographic monitoring in orthognathic surgery verified by MRI[J]. J Cranio Maxill Surg, 2015, 43 (1): 71- 80.
doi: 10.1016/j.jcms.2014.10.012 |
| 21 |
Marmulla R , Muhling J . Computer-assisted condyle positioning in orthognathic surgery[J]. J Oral Maxil Surg, 2007, 65 (10): 1963- 1968.
doi: 10.1016/j.joms.2006.11.024 |
| 22 |
Quast A , Santander P , Trautmann J , et al. A new approach in three dimensions to define pre- and intraoperative condyle-fossa relationships in orthognathic surgery: Is there an effect of general anaesthesia on condylar position?[J]. Int J Oral Max Surg, 2020, 49 (10): 1303- 1310.
doi: 10.1016/j.ijom.2020.02.011 |
| 23 |
Oh HJ , Moon JH , Ha H , et al. Virtually-planned orthognathic surgery achieves an accurate condylar position[J]. J Oral Maxillofac Surg, 2021, 79 (5): 1146.e1- 1146.e25.
doi: 10.1016/j.joms.2020.12.048 |
| 24 |
Schouman T , Rouch P , Imholz B , et al. Accuracy evaluation of CAD/CAM generated splints in orthognathic surgery: A cadaveric study[J]. Head Face Med, 2015, 11, 24.
doi: 10.1186/s13005-015-0082-9 |
| 25 |
Ritto FG , Schmitt ARM , Pimentel T , et al. Comparison of the accuracy of maxillary position between conventional model surgery and virtual surgical planning[J]. Int J Oral Maxillofac Surg, 2018, 47 (2): 160- 166.
doi: 10.1016/j.ijom.2017.08.012 |
| 26 |
Kaur A , Rattan V , Rai S , et al. Changes in condylar position after orthognathic surgery and its correlation with temporomandibular symptoms (TMD): A prospective study[J]. J Cranio Maxill Surg, 2022, 50 (12): 915- 922.
doi: 10.1016/j.jcms.2022.12.003 |
| 27 |
Lee SJ , Yang HJ , Choi MH , et al. Real-time augmented model guidance for mandibular proximal segment repositioning in orthognathic surgery, using electromagnetic tracking[J]. J Craniomaxillofac Surg, 2019, 47 (1): 127- 137.
doi: 10.1016/j.jcms.2018.10.016 |
| [1] | Andong CAI,Xiaoxia WANG,Wenjuan ZHOU,Zhonghao LIU. Comparison of the virtual surgical planning position of maxilla and condyle with the postoperative real position in patients with mandibular protrusion [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 74-80. |
| [2] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [3] | Wen ZHANG,Xiao-jing LIU,Zi-li LI,Yi ZHANG. Effect of alar base cinch suture based on anatomic landmarks on the morphology of nasolabial region in patients after orthognathic surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 736-742. |
| [4] | FENG Sha-wei,GUO Hui,WANG Yong,ZHAO Yi-jiao,LIU He. Initial establishment of digital reference standardized crown models of the primary teeth [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 327-334. |
| [5] | LI Yi,WONG Lai U,LIU Xiao-qiang,ZHOU Ti,LYU Ji-zhe,TAN Jian-guo. Marginal features of CAD/CAM laminate veneers with different materials and thicknesses [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 140-145. |
| [6] | QIU Shu-ting,ZHU Yu-jia,WANG Shi-min,WANG Fei-long,YE Hong-qiang,ZHAO Yi-jiao,LIU Yun-song,WANG Yong,ZHOU Yong-sheng. Preliminary clinical application verification of complete digital workflow of design lips symmetry reference plane based on posed smile [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 193-199. |
| [7] | XU Xiao-xiang,CAO Ye,ZHAO Yi-jiao,JIA Lu,XIE Qiu-fei. In vitro evaluation of the application of digital individual tooth tray in the impression making of mandibular full-arch crown abutments [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 54-61. |
| [8] | YUE Zhao-guo,ZHANG Hai-dong,YANG Jing-wen,HOU Jian-xia. Comparison of residual cement between CAD/CAM customized abutments and stock abutments via digital measurement in vitro [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 69-75. |
| [9] | LI Zheng,LIU Yu-shu,WANG Shi-min,ZHANG Rui,JIA Lu,YE Hong-qiang,HU Wen-jie,ZHAO Wen-yan,LIU Yun-song,ZHOU Yong-sheng. Application of biocopy function of temporary crown occlusal morphology in patients with severe attrition [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 62-68. |
| [10] | FANG Shuo-bo,YANG Guang-ju,KANG Yan-feng,SUN Yu-chun,XIE Qiu-fei. Method and accuracy of determining the jaw position of repositioning splint with the aid of digital technique [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 76-82. |
| [11] | Lang YOU,Ke-hui DENG,Wei-wei LI,Yi-jiao ZHAO,Yu-chun SUN,Yong-sheng ZHOU. Visual sensitivity threshold of lateral view of nasolabial Angle changes in edentulous jaw patients [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 107-112. |
| [12] | Shuo CHEN,Yang HE,Jin-gang AN,Yi ZHANG. Application of computer-aided virtual mandibular position in the simultaneous treatment of children with temporomandibular joint ankylosis and jaw deformity [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 954-958. |
| [13] | Jing WANG,Jun-peng CHEN,Yang WANG,Xiang-liang XU,Chuan-bin GUO. Application of digital mandibular movement record and masticatory muscle electromyography in the evaluation of stomatognathic function in patients with mandibular tumor [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 571-578. |
| [14] | Xin-xin LI,Yu-shu LIU,Yu-chun SUN,Hu CHEN,Hong-qiang YE,Yong-sheng ZHOU. Evaluation of one-piece polyetheretherketone removable partial denture fabricated by computer-aided design and computer-aided manufacturing [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 335-339. |
| [15] | Kuan-paul WANG,Hong-qiang YE,Hu CHEN,Yong WANG,Yu-chun SUN,Yong-sheng ZHOU. Establishment and preliminary clinical evaluation of edentulous custom trays designed and fabricated by chair-side CAD and 3D printing systems [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 349-355. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 537
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 405
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||