Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (1): 74-80. doi: 10.19723/j.issn.1671-167X.2024.01.012
Previous Articles Next Articles
Comparison of the virtual surgical planning position of maxilla and condyle with the postoperative real position in patients with mandibular protrusion
Andong CAI1,2,Xiaoxia WANG1,*( ),Wenjuan ZHOU3,Zhonghao LIU2,3,*(
),Wenjuan ZHOU3,Zhonghao LIU2,3,*( )
)
- 1. Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Characteristic Laboratories of Colleges and Universities in Shandong Province for Digital Stomatology, School of Stomatology, Binzhou Medical University, Yantai 264003, Shandong, China
3. Yantai Engineering Research Center for Digital Technology of Stomatology, The affiliated Yantai Stomatological Hospital, Binzhou Medical University, Yantai 264000, Shandong, China
CLC Number:
- R782.2
| 1 | 何东明, 毛丽霞, 刘凯, 等. 精准牙-骨移动的手术先行正颌正畸联合治疗——数字医学时代的理念与尝试[J]. 口腔医学, 2022, 42 (1): 20- 28. |
| 2 |
Ying X , Tian K , Zhang K , et al. Accuracy of virtual surgical planning in segmental osteotomy in combination with bimaxillary orthognathic surgery with surgery first approach[J]. BMC Oral Health, 2021, 21 (1): 529.
doi: 10.1186/s12903-021-01892-7 |
| 3 |
Lee SJ , Yoo JY , Woo SY , et al. A complete digital workflow for planning, simulation, and evaluation in orthognathic surgery[J]. J Clin Med, 2021, 10 (17): 4000.
doi: 10.3390/jcm10174000 |
| 4 |
Stamm T , Kanemeier M , Dirksen D , et al. The position of the virtual hinge axis in relation to the maxilla in digital orthognathic surgery planning: A k-means cluster analysis[J]. J Clin Med, 2023, 12 (10): 3582.
doi: 10.3390/jcm12103582 |
| 5 |
Dvoranova B , Vavro M , Czako L , et al. Does orthognathic surgery affect mandibular condyle position? A retrospective study[J]. Oral Maxillofac Surg, 2023,
doi: 10.1007/s10006-023-01181-3 |
| 6 |
Alkaabl S , Maningky M , Helder MN , et al. Virtual and tradi-tional surgical planning in orthognathic surgery: Systematic review and meta-analysis[J]. Br J Oral Maxillofac Surg, 2022, 60 (9): 1184- 1191.
doi: 10.1016/j.bjoms.2022.07.007 |
| 7 |
Quast A , Santander P , Kahlmeier T , et al. Predictability of maxillary positioning: A 3D comparison of virtual and conventional orthognathic surgery planning[J]. Head Face Med, 2021, 17 (1): 27.
doi: 10.1186/s13005-021-00279-x |
| 8 | 周颖欣, 何泽, 刘瑶, 等. 正颌术中髁突定位技术的研究进展[J]. 口腔疾病防治, 2022, 30 (4): 283- 288. |
| 9 | Lee K , Tan S , Tan D , et al. Accuracy of a digital workflow for bimaxillary orthognathic surgery: Comparison of planned and actual outcomes[J]. Int J Comput Dent, 2022, 25 (4): 397- 405. |
| 10 |
Almadi D , Benington P , Ju X , et al. Reproducibility and reliabi-lity of digital occlusal planning for orthognathic surgery[J]. Int J Oral Maxillofac Surg, 2023, 52 (10): 1074- 1080.
doi: 10.1016/j.ijom.2023.03.001 |
| 11 |
Apostolakis D , Michelinakis G , Kamposlora P , et al. The current state of computer assisted orthognathic surgery: A narrative review[J]. J Dent, 2022, 119, 104052.
doi: 10.1016/j.jdent.2022.104052 |
| 12 |
Han JJ , Woo SY , Yi WJ , et al. Robot-assisted maxillary positioning in orthognathic surgery: A feasibility and accuracy evaluation[J]. J Clin Med, 2021, 10 (12): 2596.
doi: 10.3390/jcm10122596 |
| 13 |
Neeraj , Reddy SG , Dixit A , et al. Relapse and temporomandibular joint dysfunction (TMD) as postoperative complication in skeletal class Ⅲ patients undergoing bimaxillary orthognathic surgery: A systematic review[J]. J Oral Biol Craniofac Res, 2021, 11 (4): 467- 475.
doi: 10.1016/j.jobcr.2021.06.003 |
| 14 |
Kaur A , Rattan V , Rai S , et al. Changes in condylar position after orthognathic surgery and its correlation with temporomandibular symptoms (TMD): A prospective study[J]. J Craniomaxillofac Surg, 2022, 50 (12): 915- 922.
doi: 10.1016/j.jcms.2022.12.003 |
| 15 | Ma RH , LI G , Yin S , et al. Quantitative assessment of condyle positional changes before and after orthognathic surgery based on fused 3D images from cone beam computed tomography[J]. Clin Oral Investig, 2019, 24 (8): 2663- 2672. |
| 16 |
郑博文, 刘奕. 颞下颌关节紊乱病与错 畸形特征的关系[J]. 中国实用口腔科杂志, 2023, 16 (2): 139- 142. 畸形特征的关系[J]. 中国实用口腔科杂志, 2023, 16 (2): 139- 142.
|
| 17 |
Ma W , Niu S , Wang L , et al. Clinical Application of individua-lized 3D-printed templates in the treatment of condylar osteochondroma[J]. Healthcare, 2022, 10 (11): 2163.
doi: 10.3390/healthcare10112163 |
| 18 |
Shrestha A , Song SH , Aung HN , et al. Three-dimensional cephalometric analysis: The changes in condylar position pre- and post-orthognathic surgery with skeletal class Ⅲ malocclusion[J]. J Craniofac Surg, 2021, 32 (2): 546- 551.
doi: 10.1097/SCS.0000000000006873 |
| 19 | 史舒菡, 马国武. 早期去除内固定解决正颌术后中度髁突移位1例[J]. 口腔医学研究, 2022, 38 (2): 197- 198. |
| 20 | Berköz Ö , Karaali S , Kozanoğlu E , et al. The relationship between fixation method and early central condylar sagging after bilateral sagittal split ramus osteotomy in orthognathic surgery[J]. J Craniomaxillofac Surg, 2020, 48 (10): 928- 932. |
| 21 | Zachariah T , Bharathi R , Ramanatan M , et al. The anatomical basis for plate fixation in BSSO to minimize condylar torquing: A comparative CT study of mandibular advancement and setback[J]. J Maxillofac Oral Surg, 2021, 20 (3): 432- 438. |
| 22 | Chow W , He Z , Liu Y , et al. Intraoperative condylar positioning techniques on mandible in orthognathic surgery[J]. Orthod Craniofac Res, 2022, 25 (4): 449- 458. |
| 23 | Barretto MDA , Melhem-Elias F , Deboni MCZ . Methods of mandibular condyle position and rotation center used for orthognathic surgery planning: A systematic review[J]. J Stomatol Oral Maxillofac Surg, 2022, 123 (3): 345- 352. |
| 24 | Quast A , Santander P , Trautmann J , et al. A new approach in three dimensions to define pre- and intraoperative condyle-fossa relationships in orthognathic surgery: Is there an effect of general anaesthesia on condylar position?[J]. Int J Oral Maxillofac Surg, 2020, 49 (10): 1303- 1310. |
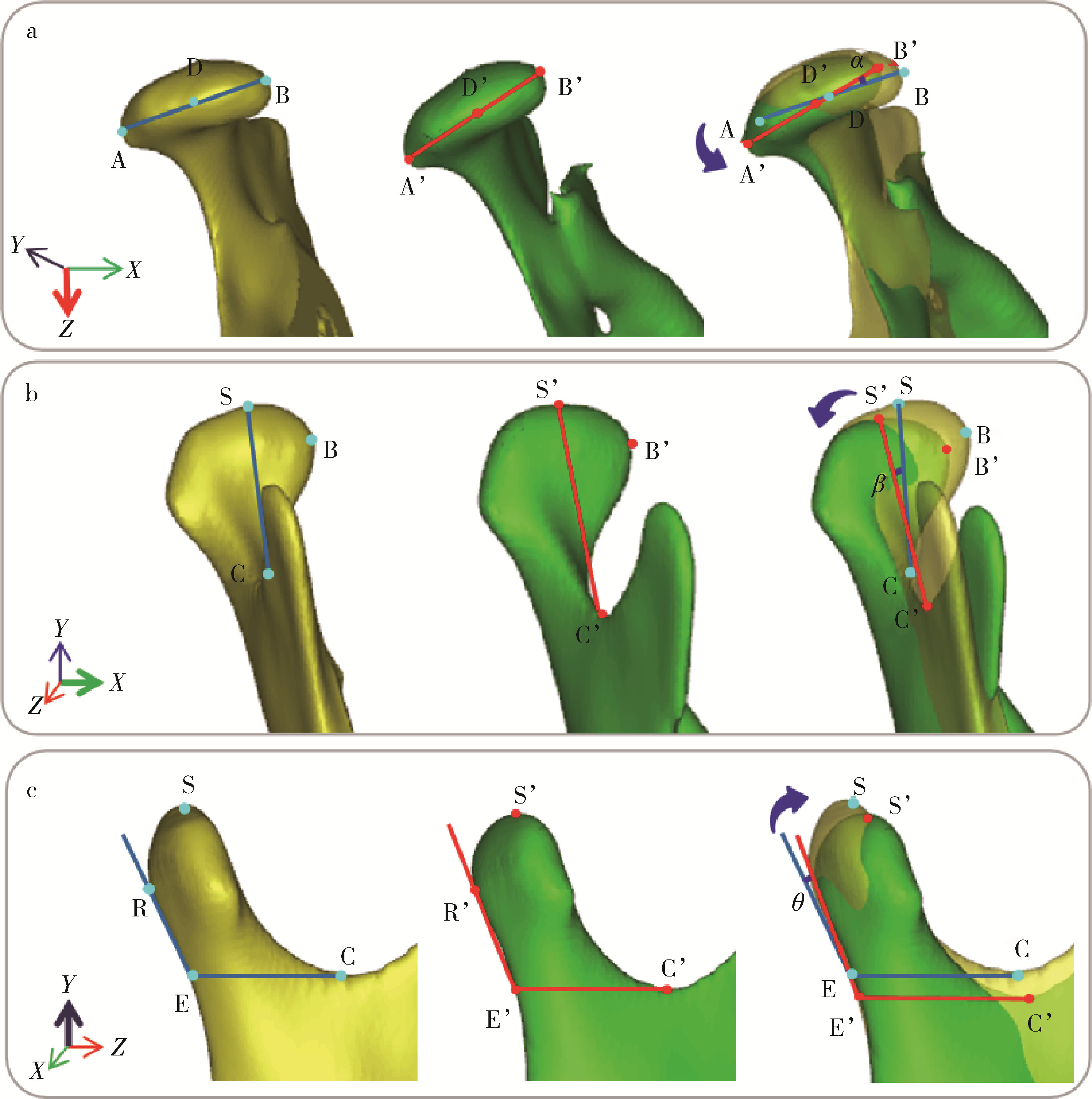
| [1] | Xinyu XU,Ling WU,Fengqi SONG,Zili LI,Yi ZHANG,Xiaojing LIU. Mandibular condyle localization in orthognathic surgery based on mandibular movement trajectory and its preliminary accuracy verification [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 57-65. |
| [2] | Wen ZHANG,Xiao-jing LIU,Zi-li LI,Yi ZHANG. Effect of alar base cinch suture based on anatomic landmarks on the morphology of nasolabial region in patients after orthognathic surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 736-742. |
| [3] | LI Zheng,LIU Yu-shu,WANG Shi-min,ZHANG Rui,JIA Lu,YE Hong-qiang,HU Wen-jie,ZHAO Wen-yan,LIU Yun-song,ZHOU Yong-sheng. Application of biocopy function of temporary crown occlusal morphology in patients with severe attrition [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 62-68. |
|
||
 ," />
," />