Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (3): 447-452. doi: 10.19723/j.issn.1671-167X.2021.03.002
Previous Articles Next Articles
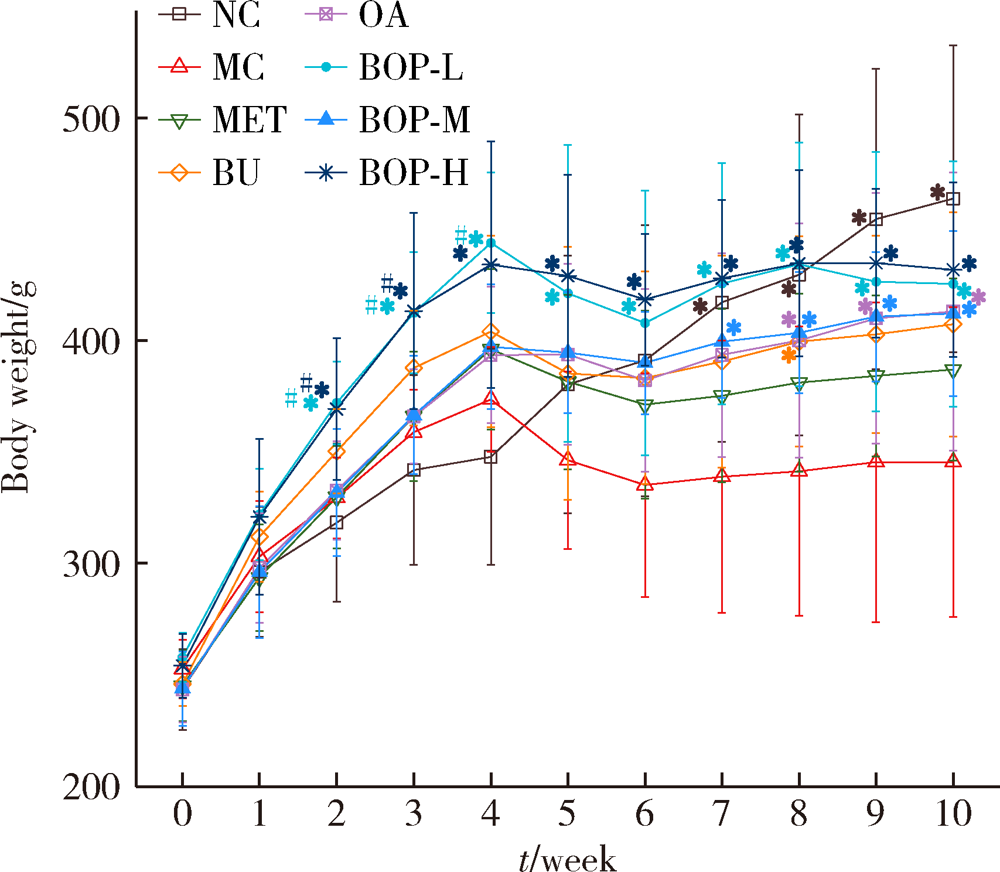
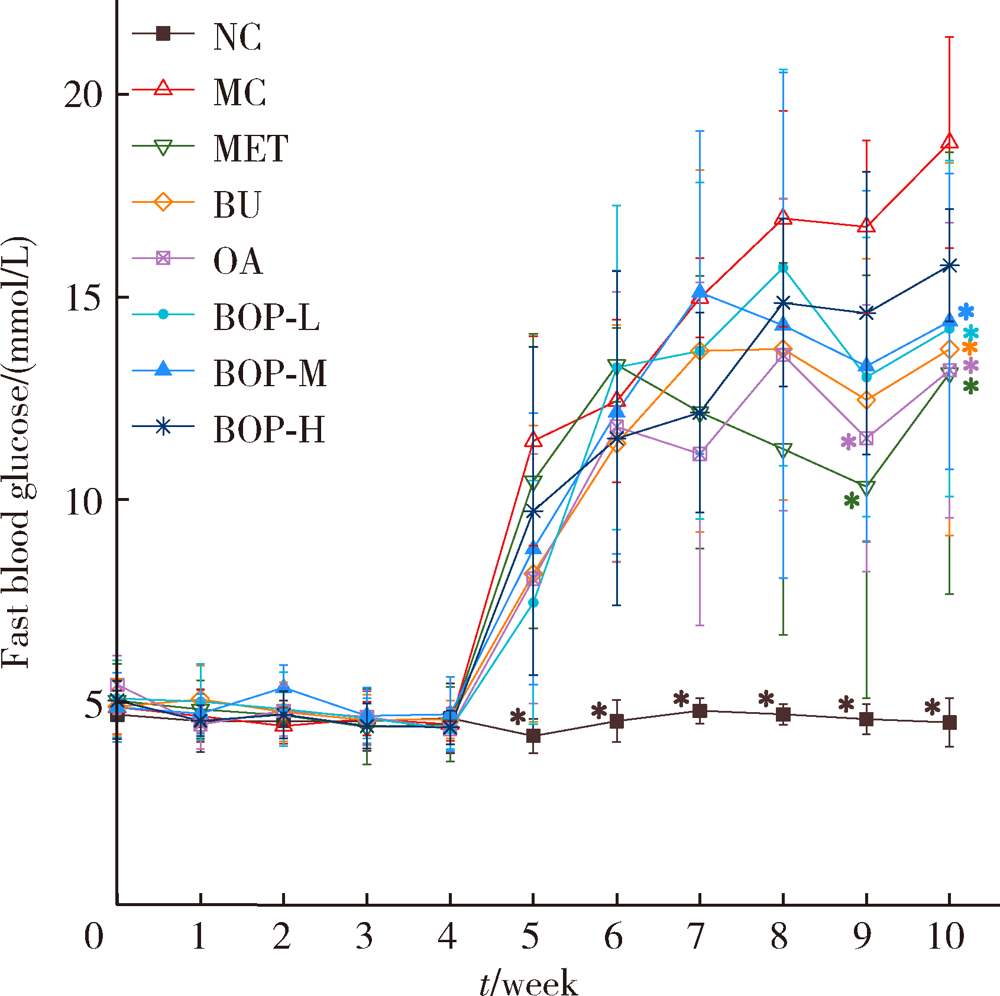
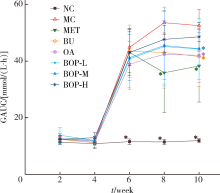
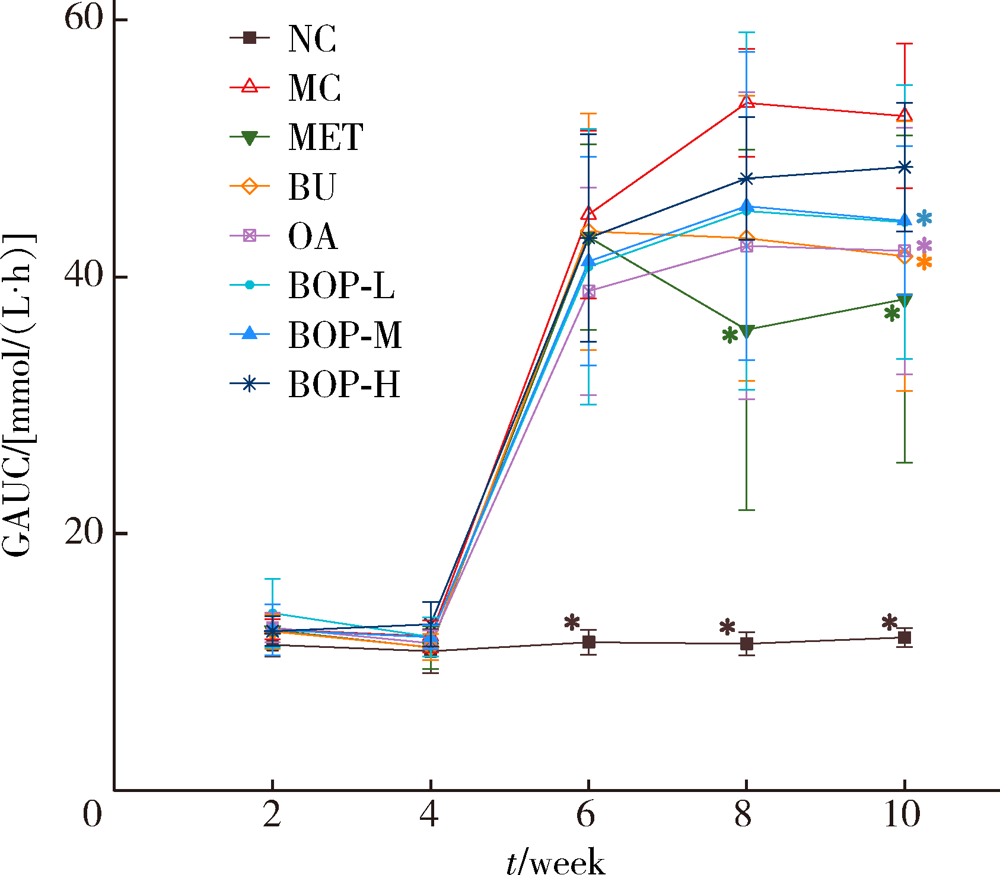
Effects of the composite of buckwheat-oat-pea on blood glucose in diabetic rats
YIN Xue-qian,ZHANG Xiao-xuan,WEN Jing,LIU Si-qi,LIU Xin-ran,ZHOU Ruo-yu,WANG Jun-boΔ( )
)
- Department of Nutrition and Food Hygiene, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- R587.1
| [1] | International Diabetes Federation. IDF Diabetes Atlas[EB/OL]. (2019-11-14) [2020-08-24]. https://www.diabetesatlas.org. |
| [2] |
Li L, Lietz G, Seal C. Buckwheat and CVD risk markers: A systematic review and meta-analysis[J]. Nutrients, 2018,10(5):619.
doi: 10.3390/nu10050619 |
| [3] |
He LX, Zhao J, Huang YS, et al. The difference between oats and beta-glucan extract intake in the management of HbA1c, fasting glucose and insulin sensitivity: a meta-analysis of rando-mized controlled trials[J]. Food Funct, 2016,7(3):1413-1428.
doi: 10.1039/C5FO01364J |
| [4] | Al-Malki AL. Oat Attenuation of hyperglycemia-induced retinal oxidative stress and NF-kappaB activation in streptozotocin-induced diabetic rats[J]. Evid Based Complement Alternat Med, 2013,2013:983923. |
| [5] |
Hashemi Z, Fouhse J, Im HS, et al. Dietary pea fiber supplementation improves glycemia and induces changes in the composition of gut microbiota, serum short chain fatty acid profile and expression of mucins in glucose intolerant rats[J]. Nutrients, 2017,9(11):1236.
doi: 10.3390/nu9111236 |
| [6] | 何宇纳, 赵丽云, 于冬梅, 等. 中国成年居民粗杂粮摄入状况[J]. 营养学报, 2016,38(2):115-118. |
| [7] |
Ruggiero E, Bonaccio M, Di Castelnuovo A, et al. Consumption of whole grain food and its determinants in a general Italian population: Results from the INHES study[J]. Nutr Metab Cardiovasc Dis, 2019,29(6):611-620.
doi: S0939-4753(19)30066-3 pmid: 30956028 |
| [8] | 韩珍华, 王瑞, 吕万勇. 糖尿病患者营养教育中粗杂粮摄入情况分析[J]. 海南医学, 2013,24(12):1842-1844. |
| [9] |
Qiu J, Liu Y, Yue Y, et al. Dietary tartary buckwheat intake attenuates insulin resistance and improves lipidprofiles in patients with type 2 diabetes: a randomized controlled trial[J]. Nutr Res, 2016,36(12):1392-1401.
doi: S0271-5317(16)30673-X pmid: 27919453 |
| [10] | 杨兰兰, 徐曼, 董方虹, 等. 燕麦饮食干预在社区2型糖尿病饮食治疗中的应用研究[J]. 中国现代医学杂志, 2018,28(19):75-79. |
| [11] |
Li X, Cai X, Ma X, et al. Short- and long-term effects of wholegrain oat intake on weight management and glucolipid metabolism in overweight type-2 diabetics: a randomized control trial[J]. Nutrients, 2016,8(9):549.
doi: 10.3390/nu8090549 |
| [12] | 梁云. 荞麦早餐饮食对糖尿病患者餐后血糖的影响[J]. 临床合理用药杂志, 2018,11(17):116-117. |
| [13] | 方海滨, 亢春雨, 郭梦冉, 等. 薏米燕麦膨化食品对高血糖血脂大鼠模型的降糖降脂作用研究[J]. 河北农业大学学报, 2018,41(6):87-91. |
| [14] | 中国食品药品监督管理局. 辅助降血糖功能评价方法[EB/OL]. (2012-04-23) [2020-08-27]. http://www.cfda.com.cn/NewsDetail.aspx?id=53366. |
| [15] |
Perez-Ramirez IF, Becerril-Ocampo LJ, Reynoso-Camacho R, et al. Cookies elaborated with oat and common bean flours improved serum markers in diabetic rats[J]. J Sci Food Agric, 2018,98(3):998-1007.
doi: 10.1002/jsfa.2018.98.issue-3 |
| [16] | 杨月欣, 王光亚, 潘兴昌. 中国食物成分表[M]. 2版. 北京: 北京大学医学出版社, 2009. |
| [17] | Beitane I, Krumina-Zemture G, Sabovics M. Technological properties of pea and buckwheat flours and their blends[M]// Treija S, Skujeniece S. Research for rural development. Jelgava: Latvia Univ Life Sciences & Technologies, 2016: 137-142. |
| [18] |
Angioloni A, Collar C. Nutritional and functional added value of oat, Kamut, spelt, rye and buckwheat versus common wheat in breadmaking[J]. J Sci Food Agric, 2011,91(7):1283-1292.
doi: 10.1002/jsfa.4314 |
| [19] | 齐婧, 吕莹果. 多谷物面条的配方优化[J]. 河南工业大学学报(自然科学版), 2018,39(3):58-64. |
| [20] | 刘淑梅, 韩淑英, 张宝忠, 等. 荞麦种子总黄酮对糖尿病高脂血症大鼠血脂、血糖及脂质过氧化的影响[J]. 中成药, 2003,25(8):60-61. |
| [21] |
Peng L, Zhang Q, Zhang Y, et al. Effect of tartary buckwheat, rutin, and quercetin on lipid metabolism in rats during high dietary fat intake[J]. Food Sci Nutr, 2020,8(1):199-213.
doi: 10.1002/fsn3.v8.1 |
| [22] |
Liu M, Zhang Y, Zhang H, et al. The anti-diabetic activity of oat β-d-glucan in streptozotocin-nicotinamide induced diabetic mice[J]. Int J Biol Macromol, 2016,91:1170-1176.
doi: 10.1016/j.ijbiomac.2016.06.083 |
| [23] |
Shen RL, Cai FL, Dong JL, et al. Hypoglycemic effects and biochemical mechanisms of oat products on streptozotocin-induced diabetic mice[J]. J Agric Food Chem, 2011,59(16):8895-8900.
doi: 10.1021/jf200678q |
| [24] | 张慧娟, 黄莲燕, 尹梦, 等. 燕麦多肽降血糖功能的研究[J]. 食品工业科技, 2017,38(10):360-363, 384. |
| [25] | 柳春, 王艳杰, 刘洋, 等. 苦荞麦提取物对糖尿病模型大鼠肾脏的保护作用及机制[J]. 中国老年学杂志, 2016,36(3):557-559. |
| [26] |
Hu Y, Hou Z, Yi R, et al. Tartary buckwheat flavonoids ameliorate high fructose-induced insulin resistance and oxidative stress associated with the insulin signaling and Nrf2/HO-1 pathwaysin mice[J]. Food Funct, 2017,8(8):2803-2816.
doi: 10.1039/C7FO00359E |
| [27] |
Hashemi Z, Yang K, Yang H, et al. Cooking enhances beneficial effects of pea seed coat consumption on glucosetolerance, incretin, and pancreatic hormones in high-fat-diet-fed rats[J]. Appl Physiol Nutr Metab, 2015,40(4):323-333.
doi: 10.1139/apnm-2014-0380 pmid: 25794240 |
| [1] | ZHU Zhen-jie, XU Qing-quan, HUANG Xiao-bo, HONG Yang, YANG Qing-ya, WANG Shu, AN Li-zhe, XU Tao. Risk factor analysis of systemic inflammatory response syndrome in type 2 diabetics after percutaneous nephrolithotomy [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 643-649. |
| [2] | SUN Ke-Xin, LIU Zhi, CAO Ya-Ying, JUAN Juan, XIANG Xiao, YANG Cheng, HUANG Shao-Ping, LIU Xiao-Fen, LI Na, TANG Xun, LI Jin, WU Tao, CHEN Da-Fang, HU Yong-Hua- . Relationship between brachial-ankle pulse wave velocity and glycemic control of type 2 diabetes mellitus patients in Beijing community population [J]. Journal of Peking University(Health Sciences), 2015, 47(3): 431-436. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 403
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 969
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||