Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 946-951. doi: 10.19723/j.issn.1671-167X.2021.05.023
Previous Articles Next Articles
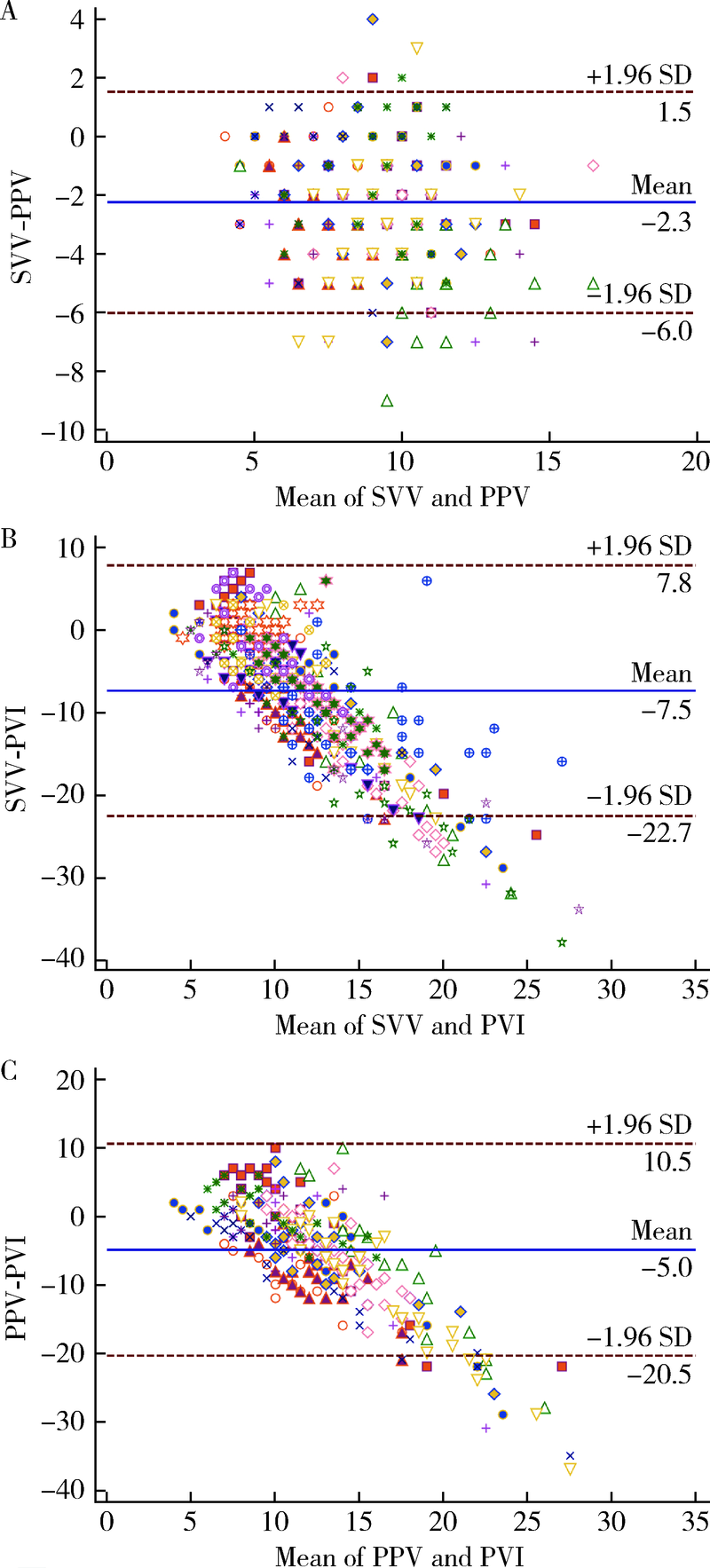
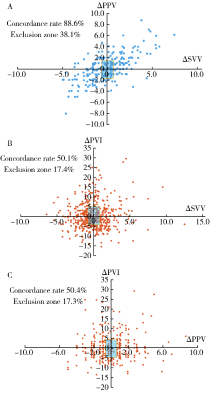
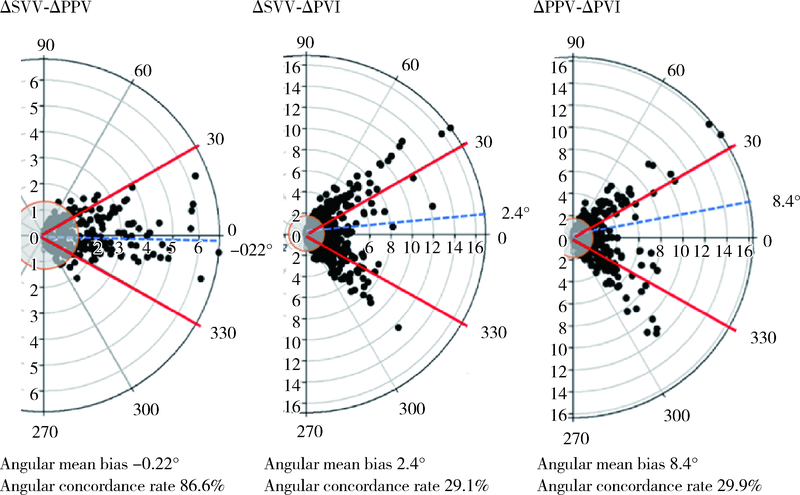
Comparison of pulse pressure variation, stroke volume variation, and plethysmographic variability index in pediatric patients undergoing craniotomy
LIU Ya-fei1,SONG Lin-lin1,△( ),XING Mao-wei1,CAI Li-xin2,WANG Dong-xin1
),XING Mao-wei1,CAI Li-xin2,WANG Dong-xin1
- 1. Department of Anesthesiology, Beijing 100034, China
2. Pediatric Epilepsy Center, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R726.1
| [1] |
Chen PH, Chan KC, Liao MH, et al. Accuracy of dynamic preload variables for predicting fluid responsiveness in patients with pediatric liver cirrhosis: a prospective study [J]. Paediatr Anaesth, 2020, 30(4):455-461.
doi: 10.1111/pan.v30.4 |
| [2] |
Cheng YW, Xu F, Li J. Identification of volume parameters monitored with a noninvasive ultrasonic cardiac output monitor for predicting fluid responsiveness in children after congenital heart disease surgery [J]. Medicine (Baltimore), 2018, 97(39):e12289.
doi: 10.1097/MD.0000000000012289 |
| [3] |
Liu T, Xu C, Wang M, et al. Reliability of pleth variability index in predicting preload responsiveness of mechanically ventilated patients under various conditions: a systematic review and meta-analysis [J]. BMC Anesthesiol, 2019, 19(1):67.
doi: 10.1186/s12871-019-0744-4 |
| [4] |
Kim DH, Shin S, Kim JY, et al. Pulse pressure variation and pleth variability index as predictors of fluid responsiveness in patients undergoing spinal surgery in the prone position [J]. Ther Clin Risk Manag, 2018, 14:1175-1183.
doi: 10.2147/TCRM |
| [5] |
Saugel B, Heeschen J, Hapfelmeier A, et al. Cardiac output estimation using multi-beat analysis of the radial arterial blood pressure waveform: a method comparison study in patients having off-pump coronary artery bypass surgery using intermittent pulmonary artery thermodilution as the reference method [J]. J Clin Monit Comput, 2020, 34(4):649-654.
doi: 10.1007/s10877-019-00375-z pmid: 31456072 |
| [6] | Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update [J]. Ann Intensive Care, 2016, 2016(6):111. |
| [7] |
Joosten A, Jacobs A, Desebbe O, et al. Monitoring of pulse pressure variation using a new smartphone application (Capstesia) versus stroke volume variation using an uncalibrated pulse wave analysis monitor: a clinical decision making study during major abdominal surgery [J]. J Clin Monit Comput, 2019, 33(5):787-793.
doi: 10.1007/s10877-018-00241-4 |
| [8] |
Ji SH, Song IK, Jang YE, et al. Comparison of pulse pressure variation and pleth variability index in the prone position in pediatric patients under 2 years old [J]. Korean J Anesthesiol, 2019, 72(5):466-471.
doi: 10.4097/kja.19128 |
| [9] |
Desgranges FP, Evain JN, Pereira de Souza NE, et al. Does the plethysmographic variability index predict fluid responsiveness in mechanically ventilated children? A meta-analysis [J]. Br J Anaesth, 2016, 117(3):409-410.
doi: 10.1093/bja/aew245 pmid: 27543550 |
| [10] |
Lee JH, Kim EH, Jang YE, et al. Fluid responsiveness in the pediatric population [J]. Korean J Anesthesiol, 2019, 72(5):429-440.
doi: 10.4097/kja.19305 |
| [1] | Shuangyun ZHAO, Siyu ZOU, Xueying LI, Lijuan SHEN, Hong ZHOU. Evaluation of reliability and validity of Chinese version of a short-form of Health Literacy Dental scale (HeLD-14) in the application among parents of preschool children [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 828-832. |
| [2] | Xinxin CHEN, Zhe TANG, Yanchun QIAO, Wensheng RONG. Caries experience and its correlation with caries activity of 4-year-old children in Miyun District of Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 833-838. |
| [3] | Zhihan YUE,Na HAN,Zheng BAO,Jinlang LYU,Tianyi ZHOU,Yuelong JI,Hui WANG,Jue LIU,Haijun WANG. A prospective cohort study of association between early childhood body mass index trajectories and the risk of overweight [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 390-396. |
| [4] | Xiuwen FEI,Si LIU,Bo WANG,Aimei DONG. Clinical characteristics and treatment in adults and children with histiocytic necroti-zing lymphadenitis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 533-540. |
| [5] | Xiao-jin YAN,Yun-fei LIU,Ning MA,Jia-jia DANG,Jing-shu ZHANG,Pan-liang ZHONG,Pei-jin HU,Yi SONG,Jun MA. Assessment of prevalence of malnutrition among Chinese primary and secondary school students and analysis of policy effect during the period of the Program for the Development of Chinese Children 2011-2020 [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 593-599. |
| [6] | Xiao-yi MI,Shan-shan HOU,Zi-yuan FU,Mo ZHOU,Xin-xuan LI,Zhao-xue MENG,Hua-fang JIANG,Hong Zhou. Reliability and validity of the Chinese version of adverse childhood experiences international questionnaire in parents of preschool children [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 408-414. |
| [7] | Meng-jie CUI,Qi MA,Man-man CHEN,Tao MA,Xin-xin WANG,Jie-yu LIU,Yi ZHANG,Li CHEN,Jia-nuo JIANG,Wen YUAN,Tong-jun GUO,Yan-hui DONG,Jun MA,Yi XING. Association between different growth patterns and metabolic syndrome in children and adolescents aged 7 to 17 years [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 415-420. |
| [8] | Jia-jia DANG,Shan CAI,Pan-liang ZHONG,Ya-qi WANG,Yun-fei LIU,Di SHI,Zi-yue CHEN,Yi-hang ZHANG,Pei-jin HU,Jing LI,Jun MA,Yi SONG. Association of outdoor artificial light at night exposure with overweight and obesity among children and adolescents aged 9 to 18 years in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 421-428. |
| [9] | Hui LI,Yang-xu GAO,Shu-lei WANG,Hong-xin YAO. Surgical complications of totally implantable venous access port in children with malignant tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1167-1171. |
| [10] | Jing LIU,Ai-dong LU,Ying-xi ZUO,Jun WU,Zhi-zhuo HUANG,Yue-ping JIA,Ming-ming DING,Le-ping ZHANG,Jiong QIN. Clinical characteristics and prognosis of seizures in 75 children with acute lymphoblastic leukemia [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 948-953. |
| [11] | Ya-xi CUI,Jun-bao DU,Qing-you ZHANG,Ying LIAO,Ping LIU,Yu-li WANG,Jian-guang QI,Hui YAN,Wen-rui XU,Xue-qin LIU,Yan SUN,Chu-fan SUN,Chun-yu ZHANG,Yong-hong CHEN,Hong-fang JIN. A 10-year retrospective analysis of spectrums and treatment options of orthostatic intolerance and sitting intolerance in children [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 954-960. |
| [12] | Tao MA,Yan-hui LI,Man-man CHEN,Ying MA,Di GAO,Li CHEN,Qi MA,Yi ZHANG,Jie-yu LIU,Xin-xin WANG,Yan-hui DONG,Jun MA. Associations between early onset of puberty and obesity types in children: Based on both the cross-sectional study and cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 961-970. |
| [13] | Yan-yan DU,Jian WANG,Lan HE,Li-na JI,Xi-wei XU. Kawasaki disease complicated with mild encephalitis/encephalopathy with a reversible splenial lesion: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 756-761. |
| [14] | Yun-fei LIU,Jia-jia DANG,Pan-liang ZHONG,Ning MA,Di SHI,Yi SONG. Injury mortality among Chinese aged 5 to 24 years from 1990 to 2019 [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 498-504. |
| [15] | Jing QIAN,You-jia WEI,Yi-jing CHENG,Yi ZHANG,Bo PENG,Chun-mei ZHU. Analysis of clinical features and risk factors of necrotizing pneumonia in children [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 541-547. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 177
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 824
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||