Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (2): 260-264. doi: 10.19723/j.issn.1671-167X.2019.02.011
Previous Articles Next Articles
Cerebral blood flow measurements in patients with comorbid hypertension and depression using 3D arterial spin labeling
Ying LIU1,Xiang-zhu ZENG1,Zheng WANG1,Han ZHANG2,Xi-lin WANG2,Hui-shu YUAN1,∆( )
)
- 1. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
2. Department of Consultation Liaison, Peking University Sixth Hospital, Beijing 100191, China
CLC Number:
- R814.46
| [1] |
Nezamzadeh M, Matson GB, Young K , et al. Improved pseudo-continuous arterial spin labeling for mapping brain perfusion[J]. J Magn Reson Imaging, 2010,31(6):1419-1427.
doi: 10.1002/jmri.22199 |
| [2] |
Shin DD, Liu TT, Wong EC , et al. Pseudocontinuous arterial spin labeling with optimized tagging efficiency[J]. Magn Reson Med, 2012,68(4):1135-1144.
doi: 10.1002/mrm.v68.4 |
| [3] |
Chen Y, Wang DJ, Detre JA . Test-retest reliability of arterial spin labeling with common labeling strategies[J]. J Magn Reson Imaging, 2011,33(4):940-949.
doi: 10.1002/jmri.v33.4 |
| [4] |
Gevers S, van Osch MJ, Bokkers RP , et al. Intra- and multicenter reproducibility of pulsed, continuous and pseudo-continuous arterial spin labeling methods for measuring cerebral perfusion[J]. J Cereb Blood Flow Metab, 2011,31(8):1706-1715.
doi: 10.1038/jcbfm.2011.10 |
| [5] |
Arnone D, Mclntosh AM, Ebmeier KP , et al. Magnetic resonance imaging studies in unipolar depression: systematic review and meta-regression analyses[J]. Eur Neuropsychopharmacol, 2012,22(1):1-16.
doi: 10.1016/j.euroneuro.2011.05.003 |
| [6] |
Bora E, Harrison BJ, Davey CG , et al. Meta-analysis of volumetric abnormalities in cortico-striatal-pallidal-thalamic circuits in major depressive disorder[J]. Psychol Med, 2012,42(4):671-681.
doi: 10.1017/S0033291711001668 |
| [7] |
Colloby SJ, Firbank MJ, He J , et al. Regional cerebral blood flow in late-life depression: Arterial spin labelling magnetic resonance study[J]. Br J Psychiatry, 2012,200(2):150-155.
doi: 10.1192/bjp.bp.111.092387 |
| [8] |
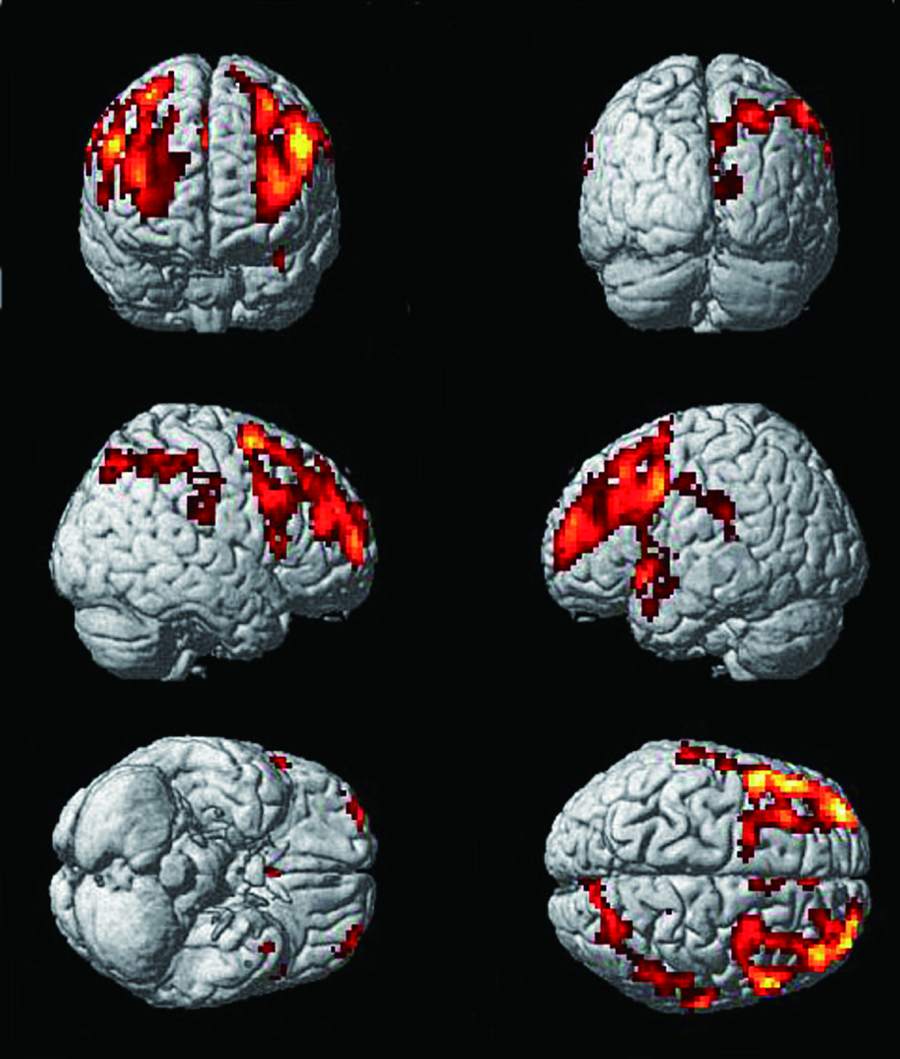
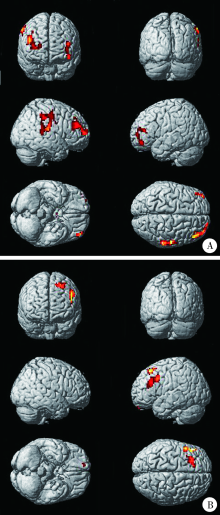
Ota M, Noda T, Sato N , et al. Characteristic distributions of regional cerebral blood flow changes in major depressive disorder patients: A pseudo-continuous arterial spin labeling (pCASL) study[J]. J Affect Disord, 2014,165:59-63.
doi: 10.1016/j.jad.2014.04.032 |
| [9] |
Naismith SL, Norrie LM, Mowszowski L , et al. The neurobiology of depression in later-life: Clinical, neuropsychological, neuro-imaging and pathophysiological features[J]. Prog Neurobiol, 2012,98(1):99-143.
doi: 10.1016/j.pneurobio.2012.05.009 |
| [10] |
Detre JA, Wang J, Wang Z , et al. Arterial spin-labeled perfusion MRI in basic and clinical neuroscience[J]. Curr Opin Neurol, 2009,22(4):348-355.
doi: 10.1097/WCO.0b013e32832d9505 |
| [11] |
Järnum H, Eskildsen SF, Steffensen EG , et al. Longitudinal MRI study of cortical thickness, perfusion, and metabolite levels in major depressive disorder[J]. Acta Psychiatr Scand, 2011,124(6):435-446.
doi: 10.1111/acps.2011.124.issue-6 |
| [12] |
Ho TC, Wu J, Shin DD , et al. Altered cerebral perfusion in exe-cutive, affective, and motor networks during adolescent depression[J]. J Am Acad Child Adolesc Psychiatry, 2013,52(10):1076-1091.
doi: 10.1016/j.jaac.2013.07.008 |
| [13] |
Lui S, Parkes LM, Huang X , et al. Depressive disorders: focally altered cerebral perfusion measured with arterial spin-labeling MR imaging[J]. Radiology, 2009,251(2):476-484.
doi: 10.1148/radiol.2512081548 |
| [14] |
Duhameau B, Ferré JC, Jannin P , et al. Chronic and treatment-resistant depression: a study using arterial spin labeling perfusion MRI at 3 Tesla[J]. Psychiatry Res, 2010,182(2):111-116.
doi: 10.1016/j.pscychresns.2010.01.009 |
| [15] |
Walther S, Höfle O, Federspiel A , et al. Neural correlates of disbalanced motor control in major depression[J]. J Affect Disord, 2012,136(1/2):124-133.
doi: 10.1016/j.jad.2011.08.020 |
| [16] | 吕粟, 黄晓琦, 孙学礼 , 等. 抑郁症患者脑MR血流灌注的图像特征[J]. 中华放射学杂志, 2009,43(3):244-248. |
| [17] |
Alosco ML, Gunstad J, Xu X , et al. The impact of hypertension on cerebral perfusion and cortical thickness in older adults[J]. J Am Soc Hypertens, 2014,8(8):561-570.
doi: 10.1016/j.jash.2014.04.002 |
| [1] | Chu-yun CHEN,Peng-fei SUN,Jing ZHAO,Jia JIA,Fang-fang FAN,Chun-yan WANG,Jian-ping LI,Yi-meng JIANG,Yong HUO,Yan ZHANG. Related factors of endogenous erythropoietin and its association with 10-year risks of cardiovascular disease in a community-based Chinese study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1068-1073. |
| [2] | Ying LIU,Ran HUO,Hui-min XU,Zheng WANG,Tao WANG,Hui-shu YUAN. Correlations between plaque characteristics and cerebral blood flow in patients with moderate to severe carotid stenosis using magnetic resonance vessel wall imaging [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 646-651. |
| [3] | Zhe LIANG,Fang-fang FAN,Yan ZHANG,Xian-hui QIN,Jian-ping LI,Yong HUO. Rate and characteristics of H-type hypertension in Chinese hypertensive population and comparison with American population [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1028-1037. |
| [4] | Yu-chao HUANG-FU,Yi-qing DU,Lu-ping YU,Tao XU. Risk factors of persistent hypertension in primary aldosteronism patients after surgery [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 686-691. |
| [5] | Zhi-sheng LI,Hao-nan QIAN,Tian-yuan FAN. Preparation and in vitro evaluation of fused deposition modeling 3D printed compound tablets of captopril and hydrochlorothiazide [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 572-577. |
| [6] | XIAO Yun-shu,ZHU Feng-yun-zhi,LUO Lan,XING Xiao-yan,LI Yu-hui,ZHANG Xue-wu,SHEN Dan-hua. Clinical and immunological characteristics of 88 cases of overlap myositis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1088-1093. |
| [7] | Hang YANG,Lin-cheng YANG,Rui-tao ZHANG,Yun-peng LING,Qing-gang GE. Risks factors for death among COVID-19 patients combined with hypertension, coronary heart disease or diabetes [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 420-424. |
| [8] | Hong-chen ZHENG,En-ci XUE,Xue-heng WANG,Xi CHEN,Si-yue WANG,Hui HUANG,Jin JIANG,Ying YE,Chun-lan HUANG,Yun ZHOU,Wen-jing GAO,Can-qing YU,Jun LV,Xiao-ling WU,Xiao-ming HUANG,Wei-hua CAO,Yan-sheng YAN,Tao WU,Li-ming LI. Bivariate heritability estimation of resting heart rate and common chronic disease based on extended pedigrees [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 432-437. |
| [9] | Wen-ying MENG,Wan-tong HUANG,Jie ZHANG,Ming-yuan JIAO,Lei JIN,Lei JIN. Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 470-478. |
| [10] | GUO Xiao-yue, SHAO Hui, ZHAO Yang-yu. A case of systemic lupus erythematosus in pregnancy complicated by pulmonary hypertension [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 928-931. |
| [11] | DONG Yan-hui, SONG Yi, DONG Bin, ZOU Zhi-yong, WANG Zheng-he, YANG Zhao-geng, WANG Xi-jie, LI Yan-hui, MA Jun. Association between the blood pressure status and nutritional status among Chinese students aged 7-18 years in 2014: based on the national blood pressure reference for Chinese children and adolescents [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 422-428. |
| [12] | ZHAO Yun, SU Bai-ge, XIAO Hui-jie, ZHANG Hong-wen, LIU Xiao-yu, WANG Fang, DING Jie. Clinical characteristics of glucocorticoid-induced eye adverse reactions in children with primary nephrotic syndrome [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 794-797. |
| [13] | LIU Xue-qin, YAN Hui, QIU Jian-xing, ZHANG Chun-yu, QI Jian-guang, ZHANG Xin, XIAO Hui-jie, YANG Yan-ling, CHEN Yong-hong, DU Jun-bao. Pulmonary arterial hypertension as leading manifestation of methylmalonic aciduria: clinical characteristics and gene testing in 15 cases [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 768-777. |
| [14] | ZHANG Hu-yang, JIAN Wei-yan, FANG Hai. Analysis of substitutional effect of outpatient expenditure on inpatient expenditure in hypertensive patients with rural new cooperative medical scheme [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 472-477. |
| [15] | YU Can-qing, CHEN Yi-ping, LV Jun, GUO Yu, Paul SHERLIKER, BIAN Zheng, ZHOU Hui-yan, TAN Yun-long, CHEN Jun-shi, CHEN Zheng-ming, LI Li-ming1. Major depressive disorder in relation with coronary heart disease and stroke in Chinese adults aged 30-79 years [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 465-471. |
|
||