Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (6): 1085-1090. doi: 10.19723/j.issn.1671-167X.2019.06.019
Previous Articles Next Articles
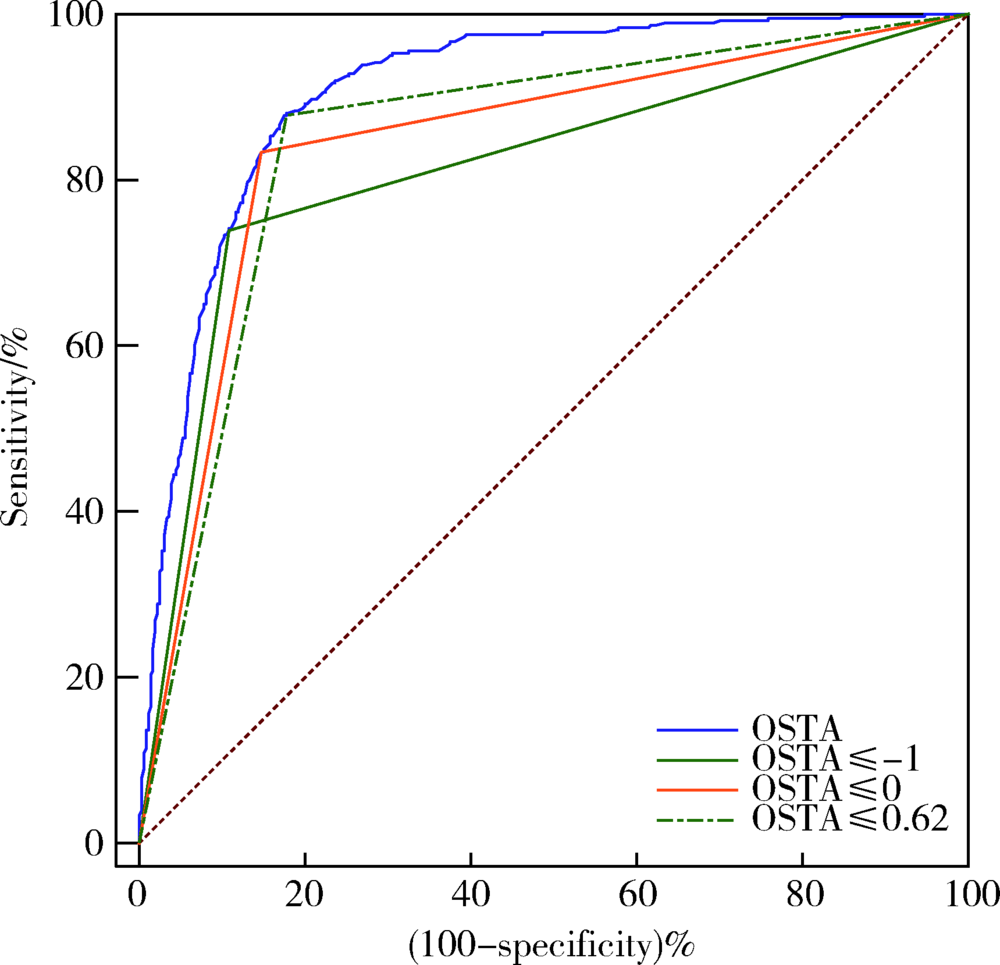
Evaluation of screening accuracy on osteoporosis self-assessment tool for Asians and its cut-off value in healthy physical examination population
Peng WANG1,Hua WU1,Ying CHE1,Dong-wei FAN2,Jue LIU3,Li-yuan TAO4,△( )
)
- 1. Medical Examination Centre, Peking University Third Hospital, Beijing 100191, China
2. Department of Orthopedics, Peking University Third Hospital, Beijing 100191, China
3. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
4. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R681
| [1] | Kanis JA, McCloskey E, Branco J, et al. Goal-directed treatment of osteoporosis in Europe[J]. Osteoporos Int, 2014,25(11):2533-2543. |
| [2] | Lorenc R, Gluszko P, Franek E , et al. Guidelines for the diagnosis and management of osteoporosis in Poland: Update 2017[J]. Endokrynol Pol, 2017,68(5):604-609. |
| [3] | Si L, Winzenberg TM, Jiang Q , et al. Projection of osteoporosis-related fractures and costs in China: 2010—2050[J]. Osteoporos Int, 2015,26(7):1929-1937. |
| [4] | Koh LK, Sedrine WB, Torralba TP , et al. A simple tool to identify Asian women at increased risk of osteoporosis[J]. Osteoporos Int, 2001,12(8):699-705. |
| [5] | Lydick E, Cook K, Turpin J , et al. Development and validation of a simple questionnaire to facilitate identification of women likely to have low bone density[J]. Am J Manag Care, 1998,4(1):37-48. |
| [6] | Cadarette SM, Jaglal SB, Kreiger N , et al. Development and validation of the osteoporosis risk assessment instrument to facilitate selection of women for bone densitometry[J]. CMAJ, 2000,162(9):1289-1294. |
| [7] | Sedrine WB, Chevallier T, Zegels B , et al. Development and assessment of the osteoporosis index of risk (OSIRIS) to facilitate selection of women for bone densitometry[J]. Gynecol Endocrinol, 2002,16(3):245-250. |
| [8] | Salaffi F, Silveri F, Stancati A , et al. Development and validation of the osteoporosis prescreening risk assessment (OPERA) tool to facilitate identification of women likely to have low bone density[J]. Clin Rheumatol, 2005,24(3):203-211. |
| [9] | Crandall CJ . Risk assessment tools for osteoporosis screening in postmenopausal women: a systematic review[J]. Curr Osteoporos Rep, 2015,13(5):287-301. |
| [10] | 中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2017)[J]. 中华骨质疏松和骨矿盐疾病杂志, 2017,10(5):413-443. |
| [11] | 《中国老年骨质疏松症诊疗指南(2018)》工作组, 中国老年学和老年医学学会骨质疏松分会, 马远征 , 等. 中国老年骨质疏松症诊疗指南(2018)[J]. 中国骨质疏松杂志, 2018,24(12):1541-1567. |
| [12] | Chang SF, Yang RS . Determining the cut-off point of osteoporosis based on the osteoporosis self-assessment tool, body mass index and weight in Taiwanese young adult women[J]. J Clin Nurs, 2014,23(17-18):2628-2636. |
| [13] | Chang AJ, Ying Q, Chen XN , et al. Evaluation of three risk assessment tools in discriminating fracture status among Chinese patients undergoing hemodialysis[J]. Osteoporosis Int, 2016,27(12):3599-3606. |
| [14] | Oh SM, Nam B, Rhee Y , et al. Development and validation of osteoporosis risk-assessment model for Korean postmenopausal women[J]. J Bone Miner Metab, 2013,31(4):423-432. |
| [15] | Pencina MJ, D’Agostino RS, D’Agostino RJ, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond[J]. Stat Med, 2008, 27(2): 157-172, 207-212. |
| [16] | Si L, Winzenberg TM, Chen M , et al. Screening for osteoporosis in Chinese post-menopausal women: a health economic modelling study[J]. Osteoporos Int, 2016,27(7):2259-2269. |
| [17] | Yang Y, Wang B, Fei Q , et al. Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporo-tic vertebral fractures in postmenopausal Chinese women in Beijing[J]. BMC Musculoskelet Disord, 2013,14:271. |
| [18] | Huang JY, Song WZ, Zeng HR , et al. Performance of the osteoporosis self-assessment tool for asians (OSTA) in screening osteoporosis among middle-aged and old women in the Chengdu region of China[J]. J Clin Densitom, 2015,18(4):539-545. |
| [19] | Li-Yu JT, Llamado LJ, Torralba TP . Validation of OSTA among Filipinos[J]. Osteoporos Int, 2005,16(12):1789-1793. |
| [20] | Muslim D, Mohd E, Sallehudin A , et al. Performance of osteoporosis self-assessment tool for asian (OSTA) for primary osteoporosis in post-menopausal Malay women[J]. Malays Orthop J, 2012,6(1):35-39. |
| [21] | Kung AW, Ho AY, Ross PD , et al. Development of a clinical assessment tool in identifying Asian men with low bone mineral density and comparison of its usefulness to quantitative bone ultrasound[J]. Osteoporos Int, 2005,16(7):849-855. |
| [22] | Oh SM, Song BM, Nam BH , et al. Development and validation of osteoporosis risk-assessment model for Korean men[J]. Yonsei Med J, 2016,57(1):187-196. |
| [23] | Liu M, Zhang Y, Cheng X , et al. The effect of age on the changes in bone mineral density and osteoporosis detection rates in Han Chinese men over the age of 50[J]. Aging Male, 2014,17(3):166-173. |
| [24] | Huang JY, Song WZ, Huang M . Effectiveness of osteoporosis self-assessment tool for Asians in screening for osteoporosis in healthy males over 40 years old in China[J]. J Clin Densitom, 2017,20(2):153-159. |
| [25] | Geater S, Leelawattana R, Geater A . Validation of the OSTA index for discriminating between high and low probability of femoral neck and lumbar spine osteoporosis among Thai postmenopausal women[J]. J Med Assoc Thai, 2004,87(11):1286-1292. |
| [26] | Chan SP, Teo CC, Ng SA , et al. Validation of various osteoporosis risk indices in elderly Chinese females in Singapore[J]. Osteoporos Int, 2006,17(8):1182-1188. |
| [27] | Moon JH, Kim LO, Kim HJ , et al. Evaluation of the predictive index for osteoporosis as a clinical tool to identify the risk of osteoporosis in Korean men by using the Korea National Health and Nutrition Examination Survey Data[J]. Korean J Fam Med, 2016,37(6):346-350. |
| [28] | Zha XY, Hu Y, Pang XN , et al. Diagnostic value of osteoporosis self-assessment tool for Asians (OSTA) and quantitative bone ultrasound (QUS) in detecting high-risk populations for osteoporosis among elderly Chinese men[J]. J Bone Miner Metab, 2015,33(2):230-238. |
| [1] | Rui-jie CAO,Zhong-qiang YAO,Peng-qing JIAO,Li-gang CUI. Comparison of diagnostic efficacy of different classification criteria for Takayasu arteritis in Chinese patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1128-1133. |
| [2] | Hai-hong YAO,Su-mei TANG,Zhi-min WANG,Xia ZHANG,Xu-yong CHEN,Li GAO,Jing LIU,Yi-jun DAI,Zhao-heng HU,Xue-wu ZHANG,Zhan-guo LI. Study of bone mineral density and serum bone turnover markers in newly diagnosed systemic lupus erythematosus patients [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 998-1003. |
| [3] | CAO Jie, MENG Huan-xin. Evaluation of using cone beam computed tomography as a regular test before and after periodontal regenerative surgery#br# [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 110-116. |
| [4] | XU Xiao, XU Li, JIANG Jiu-hui, WU Jia-qi, LI Xiao-tong, JING Wu-di. Accuracy analysis of alveolar dehiscence and fenestration of maxillary anterior teeth of Angle class Ⅲ by cone-beam CT [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 104-109. |
| [5] | WANG Yu, HAO Yan-jie, DENG Xue-rong, LI Guang-tao, GENG Yan, ZHAO Juan, ZHOU Wei, ZHANG Zhuo-li. Risk factors for bone mineral density changes in patients with rheumatoid arthritis and fracture risk assessment [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 781-786. |
| [6] | WANG Yu, GENG Yan, DENG Xue-rong, ZHANG Zhuo-li. Relationship between wrist bone mineral density and synovitis, erosion by ultrasonography in female rheumatoid arthritis patients [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 774-780. |
| [7] | WEI Pan, LU Song-He, FU Jing-Ya, YAN Zhi-Min, HUA Hong. Validation of the American College of Rheumatology Classification Criteria for primary Sjögren’s syndrome in Chinese patients [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 306-310. |
| [8] | YU Yang, SHENG Qin-Hui, ZHANG Bao-Wei, DING Wen-Hui. Left atrial size predicts adverse cardiac events in patients with non-obstruction hypertrophic cardiomyopathy [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 207-210. |
|
||