Journal of Peking University(Health Sciences) ›› 2020, Vol. 52 ›› Issue (1): 90-96. doi: 10.19723/j.issn.1671-167X.2020.01.014
Previous Articles Next Articles
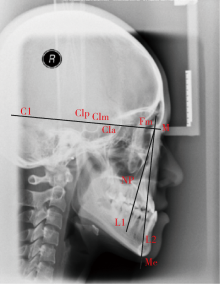
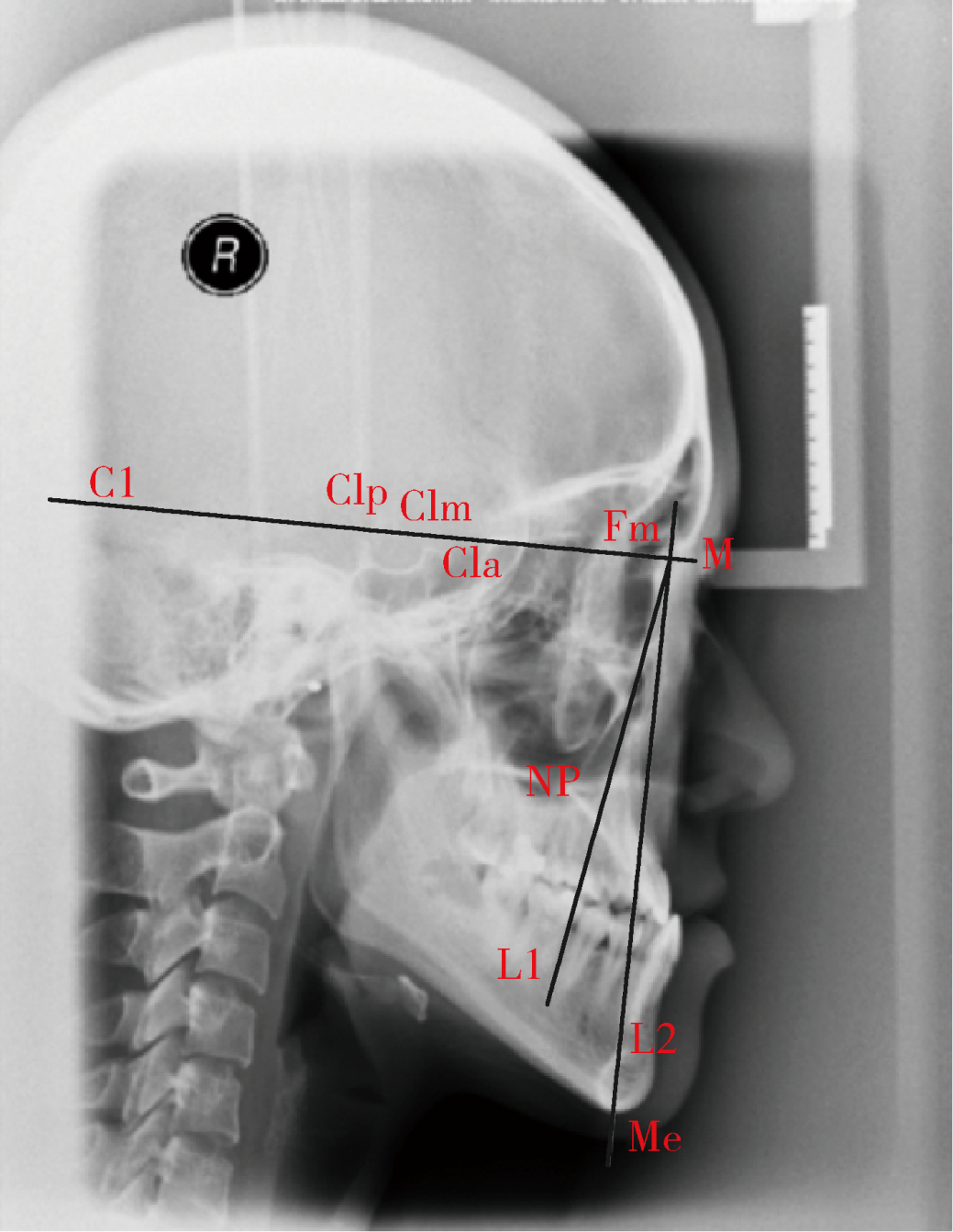
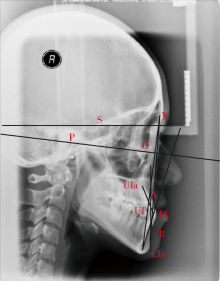
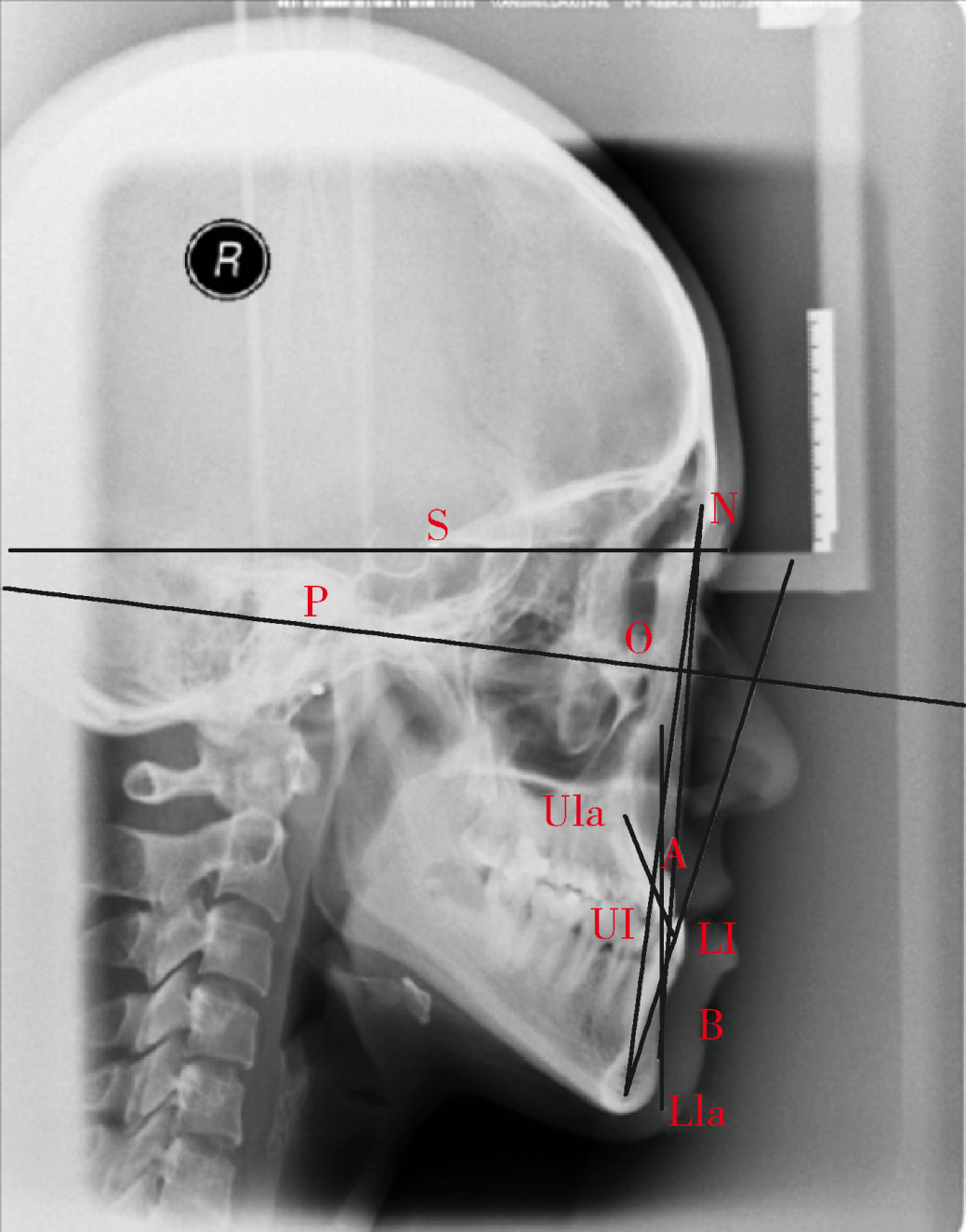
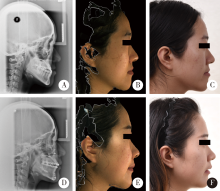
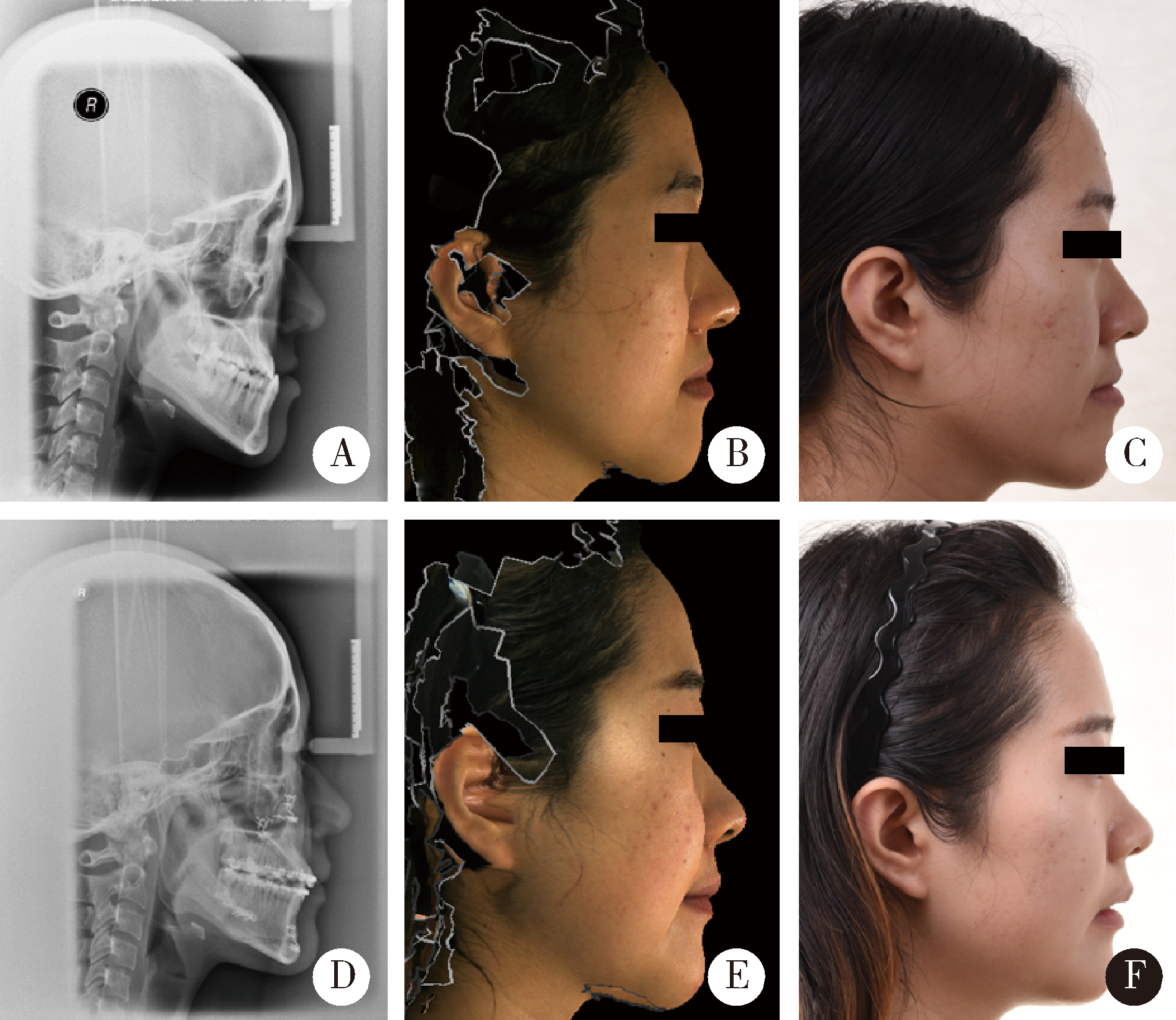
Feasibility of Delaire cephalometric analysis to predict the ideal sagittal position of the maxilla and chin for surgery-first patients in orthognathic surgery
Xian-tao SUN,Wei HE,Xiao-jing LIU,Zi-li LI( ),Xing WANG
),Xing WANG
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Disease & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.2
| [1] | Hussels W, Nanda RS . Analysis of factors affecting angle ANB[J]. Am J Orthod, 1984,85(5):411-423. |
| [2] | Resnick CM, Kim S, Yorlets RR , et al. Evaluation of Andrews’ analysis as a predictor of ideal sagittal maxillary positioning in orthognathic surgery[J]. J Oral Maxillofac Surg, 2018,76(10):2169-2176. |
| [3] | Resnick CM, Daniels KM, Vlahos M . Does Andrews facial analysis predict esthetic sagittal maxillary position?[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2018,125(4):376-381. |
| [4] | Resnick CM, Calabrese CE, Resnick AS . Maxillary sagittal position in relation to the forehead: A target for orthognathic surgery[J]. J Craniofac Surg, 2018,29(3):688-691. |
| [5] | Jiang Z, Tan L, Hu L , et al. Clinician, dental student, and orthognathic patient perception of black-and-white silhouette lateral profile dimensions of ideal chin position in a Chinese population[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2018,125(1):e1-e7. |
| [6] | Ghaleb N, Bouserhal J, Bassil-Nassif N . Aesthetic evaluation of profile incisor inclination[J]. Eur J Orthod, 2011,33(3):228-235. |
| [7] | Webb MA, Cordray FE, Rossouw PE . Upper-incisor position as a determinant of the ideal soft-tissue profile[J]. J Clin Orthod, 2016,50(11):651-662. |
| [8] | Tourne LP, Bevis RL, Cavanaugh G . A validity test of cephalometric variables as a measure of clinical applicability in anteroposterior profile assessment[J]. Int J Adult Orthodon Orthognath Surg, 1993,8(2):95-112. |
| [9] | Tulloch C, Phillips C, Dann C . Cephalometric measures as indicators of facial attractiveness[J]. Int J Adult Orthodon Orthognath Surg, 1993,8(3):171-179. |
| [10] | 王涛 . Delaire颅颌面整体平衡理论与正颌外科策略[J]. 中国口腔颌面外科杂志, 2005,3(2):155-158. |
| [11] | Doğan S, Ertürk N . Delaire’s architectural and structural cranio-facial analysis in cephalometric evaluation[J]. Turkish J Orthod, 1989,2(1):103. |
| [12] | Bell WH, Ferraro JW . Modern practice in orthognathic and reconstructive surgery[J]. Plast Reconstr Surg, 1993,92(2):362. |
| [13] | Yang L, Xiao YD, Liang YJ , et al. Does the surgery-first approach produce better outcomes in orthognathic surgery? A systematic review and meta-analysis[J]. J Oral Maxillofac Surg, 2017,75(11):2422-2429. |
| [14] | Park JK, Choi JY, Yang IH , et al. Patient’s satisfaction in skeletal class Ⅲ cases treated with two-jaw surgery using orthognathic quality of life questionnaire: Conventional three-stage method versus surgery-first approach[J]. J Craniofac Surg, 2015,26(7):2086-2093. |
| [15] | Yamauchi K, Takahashi T, Yamaguchi Y , et al. Effect of “surgery first” orthognathic approach on temporomandibular symptoms and function: A comparison with “orthodontic first” approach[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2019,127(5):387-392. |
| [16] | Lo SH, Chen YA, Yao CF , et al. Is skeletal stability after bimaxillary surgery for skeletal class III deformity related to surgical occlusal contact?[J]. Int J Oral Maxillofac Surg, 2019,48(10):1329-1336. |
| [17] | Lee SH, Kil TJ, Park KR , et al. Three-dimensional architectural and structural analysis: A transition in concept and design from Delaire’s cephalometric analysis[J]. Int J Oral Maxillofac Surg, 2014,43(9):1154-1160. |
| [18] | 陈梦苇, 宋锦磷, 王涛 , 等. 重庆地区正常牙合人群颅颌面硬组织结构特征的Delaire头影测量初步研究[J]. 第三军医大学学报, 2008,30(4):351-354. |
| [19] | Tanaka JL, Ono E, Filho Medici E , et al. Influence of the facial pattern on ANB, AF-BF, and Wits appraisal[J]. World J Orthod, 2006,7(4):369-375. |
| [20] | 吴笑尘, 刘筱菁, 李自力 , 等. 一种头影测量分析法矢状向参考线在中国美貌人群中特点初探[J]. 中华口腔正畸学杂志, 2015,22(4):211-214. |
| [21] | Olate S, Zaror C, Blythe JN , et al. A systematic review of soft-to-hard tissue ratios in orthognathic surgery. Part Ⅲ: Double jaw surgery procedures[J]. J Craniomaxillofac Surg, 2016,44(10):1599-1606. |
| [22] | San Miguel Moragas J, Oth O, Buttner M , et al. A systematic review on soft-to-hard tissue ratios in orthognathic surgery part Ⅱ: Chin procedures[J]. J Craniomaxillofac Surg, 2015,43(8):1530-1540. |
| [1] | Lei HOU,Guo-hua YE,Xiao-jing LIU,Zi-li LI. Evaluation of mandibular stability and condylar volume after orthognathic surgery in patients with severe temporomandibular joint osteoarthrosis [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 113-118. |
| [2] | Xiu-jing WANG,Yi-mei ZHANG,Yan-heng ZHOU. Orthodontic-orthognathic treatment stability in skeletal class Ⅲ malocclusion patients [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 86-92. |
| [3] | WU Ling, LIU Xiao-jing, LI Zi-li, WANG Xing. Evaluation of accuracy of virtual occlusal definition in Angle class Ⅰ molar relationship [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 154-159. |
| [4] | WANG Zhe, ZHU Liu-ning, ZHOU Lin, YI Biao. Feasibility of integrating 3D photos and cone-beam computed tomography images used to evaluate changes of soft and hard tissue after orthognathic surgery [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 544-549. |
| [5] | HE Ying, GUO Chuan-Bin, DENG Xu-Liang, WANG Xing, WANG Xiao-Xia. Three-dimensional measurement and facial symmetry analysis for the craniofacial structure of people in North China with normal occlusion [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 708-713. |
| [6] | CHEN Shuo, LIU Xiao-Jing, LI Zi-Li, LIANG Cheng, WANG Xiao-Xia, FU Kai-Yuan, YI Biao. Three-dimensional evaluation of condylar morphology remodeling after orthognathic surgery in mandibular retrognathism by cone-beam computed tomography [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 703-707. |
|
||