Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (2): 370-374. doi: 10.19723/j.issn.1671-167X.2023.02.026
Previous Articles Next Articles
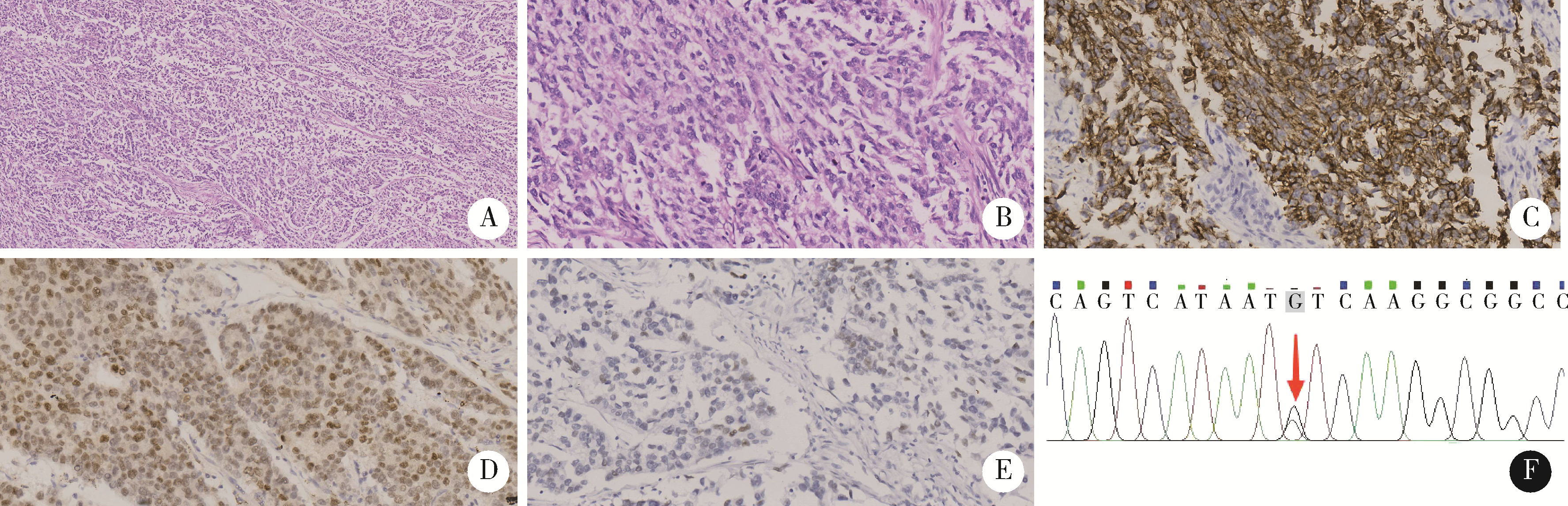
Uterine POLE mutant endometrioid carcinoma combined with human papilloma virus-associated cervical adenocarcinoma: A case report and literature review
Fang CAO1,2,Ming ZHONG3,Cong-rong LIU2,*( )
)
- 1. Department of Pathology, Hunan Cancer Hospital, Changsha 410000, China
2. Department of Pathology, Peking University School of Basic Medical Sciences/Peking University Third Hospital, Beijing 100191, China
3. Tai'an Center Hospital, Tai'an 271000, Shandong, China
CLC Number:
- R737.33
| 1 | 谢加琼, 莫婷, 任黔川. 宫颈癌肉瘤合并卵巢癌和子宫内膜癌1例[J]. 实用妇产科杂志, 2016, 32 (8): 637- 638. |
| 2 | Nakra T, Biswas R, Pandey R, et al. Synchronous endometrioid carcinoma of the endometrium and small cell neuroendocrine carcinoma of the cervix: A rare combination[J]. BMJ Case Rep, 2018, 2018: bcr2018227155. |
| 3 | Park ST , Song MJ , Lee CW , et al. Synchronous clear cell adenocarcinoma of the cervix and endometrioid carcinoma of the endometrium[J]. Eur J Gynaecol Oncol, 2011, 32 (5): 573- 575. |
| 4 | Stewart CJR , Crum CP , McCluggage WG , et al. Guidelines to aid in the distinction of endometrial and endocervical carcinomas, and the distinction of independent primary carcinomas of the endome-trium and adnexa from metastatic spread between these and other sites[J]. Int J Gynecol Pathol, 2019, 38 (Iss 1 Suppl 1): S75- S92. |
| 5 |
Jung H , Bae GE , Kim HM , et al. Clinicopathological and mole-cular differences between gastric-type mucinous carcinoma and usual-type endocervical adenocarcinoma of the uterine cervix[J]. Cancer Genomics Proteomics, 2020, 17 (5): 627- 641.
doi: 10.21873/cgp.20219 |
| 6 |
Wang F , Flanagan J , Su N , et al. RNAscope: A novel in situ RNA analysis platform for formalin-fixed, paraffin-embedded tissues[J]. J Mol Diagn, 2012, 14 (1): 22- 29.
doi: 10.1016/j.jmoldx.2011.08.002 |
| 7 |
Nuovo GJ , Plaia TW , Belinsky SA , et al. In situ detection of the hypermethylation-induced inactivation of the p16 gene as an early event in oncogenesis[J]. Proc Natl Acad Sci USA, 1999, 96 (22): 12754- 12759.
doi: 10.1073/pnas.96.22.12754 |
| 8 | WHO Classification of Tumours Editorial . Female genital tumours: WHO classification of tumours[M]. 5th ed Geneva: World Health Organization,, 2020. |
| 9 |
Crosbie EJ , Einstein MH , Franceschi S , et al. Human papillomavirus and cervical cancer[J]. Lancet, 2013, 382 (9895): 889- 899.
doi: 10.1016/S0140-6736(13)60022-7 |
| 10 | 程傲霜, 李晶, 林仲秋. 《2020 ESGO-ESTRO-ESP子宫内膜癌患者管理指南》解读[J]. 中国实用妇科与产科杂志, 2021, 37 (3): 336- 341. |
| [1] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [2] | HU Jun, ZHENG Pei-zi, ZHU Li-rong. Comparison of clinical pathological characteristics in ovarian preserving patients with stage ⅠB1 cervical adenocarcinoma and squamous cell carcinoma [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 783-787. |
| [3] | MA Ke, YANG Yi-he, YANG Xi, FENG Zhao-Yi, LIU Tong-yu, WEN Hong-wu, LIAO Qin-ping. Efficacy of postoperative simple chemotherapy and concurrent chemoradiotherapy in FIGO stage ⅠB2-ⅡB cervical cancer [J]. Journal of Peking University(Health Sciences), 2013, 45(6): 910-915. |
|
||