Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 470-478. doi: 10.19723/j.issn.1671-167X.2020.03.012
Previous Articles Next Articles
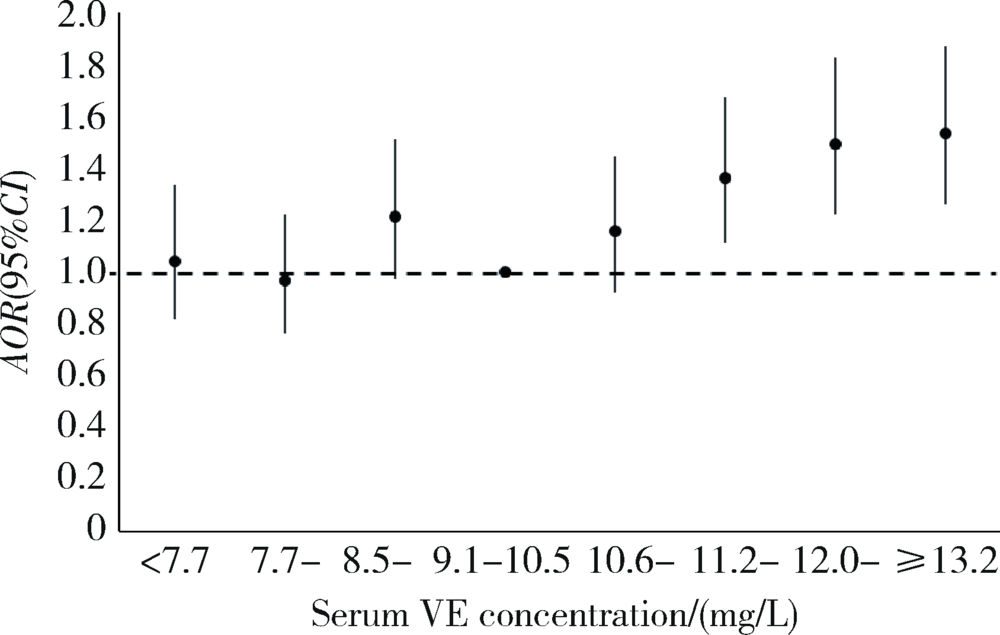
Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy
Wen-ying MENG1,Wan-tong HUANG2,Jie ZHANG2,Ming-yuan JIAO3,Lei JIN4,Lei JIN2,△( )
)
- 1. Department of Obstetrics, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
2. Institute of Reproductive and Child Health, National Health Commission Key Laboratory of Reproductive Health, Peking University, Beijing 100191, China; Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
3. Department of Clinical Laboratory, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
4. Department of Maternal Health Care, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
CLC Number:
- R172
| [1] | 谢幸, 苟文丽. 妇产科学[M]. 8版. 北京: 人民卫生出版社, 2013: 42, 64. |
| [2] | 中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南(2015)[J]. 中华围产医学杂志, 2016,19(3):161-169. |
| [3] |
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis[J]. Hypertens Res, 2017,40(3):213-220.
pmid: 27682655 |
| [4] | Ye C, Ruan Y, Zou L, et al. The 2011 survey on hypertensive disorders of pregnancy (HDP) in China: prevalence, risk factors, complications, pregnancy and perinatal outcomes[J]. PLoS One, 2014,9(6):e100180. |
| [5] |
You SH, Cheng PJ, Chung TT, et al. Population-based trends and risk factors of early- and late-onset preeclampsia in Taiwan 2001—2014[J]. BMC Pregnancy Childbirth, 2018,18(1):199.
pmid: 29855344 |
| [6] | Paré E, Parry S, McElrath TF, et al. Clinical risk factors for preeclampsia in the 21st century[J]. Obstet Gynecol, 2014,124(4):763-770. |
| [7] |
Redman CW, Sargent IL. Latest advances in understanding preeclampsia[J]. Science, 2005,308(5728):1592-1594.
pmid: 15947178 |
| [8] | 殷为, 钟梅. 妊娠期高血压疾病的病因、预测及诊疗进展[J]. 实用医学杂志, 2016,32(11):1887-1890. |
| [9] | 孙长颢. 营养与食品卫生学[M]. 8版. 北京: 人民卫生出版社, 2017: 93-95, 215. |
| [10] | 郭方, 李笑天. 叶酸及多种维生素的补充对妊娠期高血压疾病的预防作用[J]. 中国实用妇科与产科杂志, 2014,30(8):592-596. |
| [11] | Rumbold A, Ota E, Hori H, et al. Vitamin E supplementation in pregnancy[J]. Cochrane Database Syst Rev, 2015(9): CD004069. |
| [12] |
Zhang C, Williams MA, Sanchez SE, et al. Plasma concentrations of carotenoids, retinol, and tocopherols in preeclamptic and normotensive pregnant women[J]. Am J Epidemiol, 2001,153(6):572-580.
pmid: 11257065 |
| [13] | Roberts JM, Myatt L, Spong CY, et al. Vitamins C and E to prevent complications of pregnancy-associated hypertension[J]. N Engl J Med, 2010,362(14):1282-1291. |
| [14] | Poston L, Briley AL, Seed PT, et al. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP trial): randomised placebo-controlled trial[J]. Lancet, 2006,367(9517):1145-1154. |
| [15] |
Rajasingam D, Seed PT, Briley AL, et al. A prospective study of pregnancy outcome and biomarkers of oxidative stress in nulliparous obese women[J]. Am J Obstet Gynecol, 2009,200(4):395.
pmid: 19200933 |
| [16] | 康忠春, 陈远兰, 邹余粮. 妊娠子痫前期孕妇维生素A、E水平及其影响因素分析[J]. 临床医学研究与实践, 2018,3(30):142-144. |
| [17] | 张翠, 靳颖, 杨洁, 等. 河北省产妇2016年妊娠期高血压疾病患病情况分析[J]. 中国公共卫生, 2018,34(10):1395-1397. |
| [18] | 牛影, 徐叶清, 郝加虎, 等. 马鞍山市妇女孕前体质指数和孕期增重与妊娠期高血压疾病的队列研究[J]. 卫生研究, 2016,45(2):205-210. |
| [19] | 申南, 陆娣, 郑春梅, 等. 常规保健下不同年龄段孕妇妊娠早期血清维生素A、E水平分析[J]. 中国妇产科临床杂志, 2018,19(4):356-358. |
| [20] | 闫明, 张雯, 刘凯波, 等. 北京地区2010年—2017年增补叶酸预防神经管缺陷工作效果分析[J]. 中国优生与遗传杂志, 2019,27(3):339-341. |
| [21] | Schiff E, Friedman SA, Stampfer M, et al. Dietary consumption and plasma concentrations of vitamin E in pregnancies complicated by preeclampsia[J]. Am J Obstet Gynecol, 1996,175(4 Pt 1):1024-1028. |
| [22] |
Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies[J]. BMJ, 2016,353:i1753.
pmid: 27094586 |
| [23] | Rumbold AR, Crowther CA, Haslam RR, et al. Vitamins C and E and the risks of preeclampsia and perinatal complications[J]. N Engl J Med, 2006,354(17):1796-1806. |
| [24] | Bowman BA, Russell RM. 现代营养学[M]. 8版. 荫士安,汪之顼, 译. 北京: 化学工业出版社, 2004: 195. |
| [25] | Karpińska J, Mikołuć B, Motkowski R, et al. HPLC method for simultaneous determination of retinol, alpha-tocopherol and coenzyme Q10 in human plasma [J]. J Pharm Biomed Anal, 2006,42(2):232-236. |
| [26] | 马蕊, 刘建蒙, 李松, 等. 浙江省嘉兴地区妊娠高血压综合征发病状况研究[J]. 中华流行病学杂志, 2005,26(12):960-963. |
| [27] | Yusuf H, Subih HS, Obeidat BS, et al. Associations of macro and micronutrients and antioxidants intakes with preeclampsia: A case-control study in Jordanian pregnant women[J]. Nutr Metab Car-diovasc Dis, 2019,29(5):458-466. |
| [28] | 孟凡文, 陈森, 刘亚山, 等. 河北省5县区妊娠期高血压疾病的发病情况及危险因素分析[J]. 中国生育健康杂志, 2015,26(2):112-115. |
| [1] | Huichao MA,Jun LI,Yongqing WANG. Clinical characteristics of pregnancy complicated with inflammatory bowel disease [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 260-266. |
| [2] | Yangyang LI,Lin HOU,Zijun MA,Shanyamei HUANG,Jie LIU,Chaomei ZENG,Jiong QIN. Association of pregnancy factors with cow's milk protein allergy in infants [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 144-149. |
| [3] | Fang-ning YOU,Liang LUO,Xiang-jun LIU,Xue-wu ZHANG,Chun LI. Analysis of pregnancy outcomes, disease progression, and risk factors in patients with undifferentiated connective tissue disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1045-1052. |
| [4] | Yu-fei LI,Ya-ni YAN,Jia-yang JIN,Chun LI,Qiu-yan PEI. Clinical characteristics of fetal cardiac disease in patients with anti-SSA antibody positive [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1053-1057. |
| [5] | Chu-yun CHEN,Peng-fei SUN,Jing ZHAO,Jia JIA,Fang-fang FAN,Chun-yan WANG,Jian-ping LI,Yi-meng JIANG,Yong HUO,Yan ZHANG. Related factors of endogenous erythropoietin and its association with 10-year risks of cardiovascular disease in a community-based Chinese study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1068-1073. |
| [6] | Jie WU,Wen ZHANG,Shu LIANG,Yi-lu QIN,Wen-qiang FAN. Pregnancy-associated neuromyelitis optical spectrum disorder combined with primary Sjögren's syndrome: A critical illness case report [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1118-1124. |
| [7] | Jin-hui XU,Na HAN,Tao SU,Li-zi LIN,Yue-long JI,Shuang ZHOU,He-ling BAO,Zheng LIU,Shu-sheng LUO,Xiang-rong XU,Hai-jun WANG. Association of maternal isolated thyroid peroxidase antibody positive in the first trimester with fetal growth [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 886-892. |
| [8] | Yong-wei LIN,Ya-lin ZHOU,Run-long ZHAO,Ya-jun XU,Yan-ping LIU. Analysis on the iron status and associated factors during the first trimester of pregnancy [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 600-605. |
| [9] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [10] | Xi-ya SUN,Yi-lu CHEN,Lin ZENG,Li-ying YAN,Jie QIAO,Rong LI,Xu ZHI. Correlation analysis of vitamin D level and anti-Müllerian hormone in infertile female and the role in predicting pregnancy outcome [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 167-173. |
| [11] | Zhe LIANG,Fang-fang FAN,Yan ZHANG,Xian-hui QIN,Jian-ping LI,Yong HUO. Rate and characteristics of H-type hypertension in Chinese hypertensive population and comparison with American population [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1028-1037. |
| [12] | Chieko MORIMOTO,Yi-qin WANG,Rong ZHOU,Jian-liu WANG. Clinical analysis of fertility-sparing therapy of patients with complex atypical hyperplasia and endometrial cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 936-942. |
| [13] | Hong-xia ZHANG,Rui YANG,Shuo YANG,Ning-ning PAN,Lin-lin WANG,Rong LI. Clinical effect of fetal reduction by intracranial and intrathoracic KCl injection [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 943-947. |
| [14] | Yu-chao HUANG-FU,Yi-qing DU,Lu-ping YU,Tao XU. Risk factors of persistent hypertension in primary aldosteronism patients after surgery [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 686-691. |
| [15] | Yang-yang CHEN,Yu-bo ZHOU,Jing YANG,Yu-meng HUA,Peng-bo YUAN,Ai-ping LIU,Yuan WEI. Effects of gestational weight on the association between serum high sensitivity C reaction protein and gestational diabetes mellitus among twin gestations: A cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 427-433. |
|
||