Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 1045-1052. doi: 10.19723/j.issn.1671-167X.2023.06.014
Previous Articles Next Articles
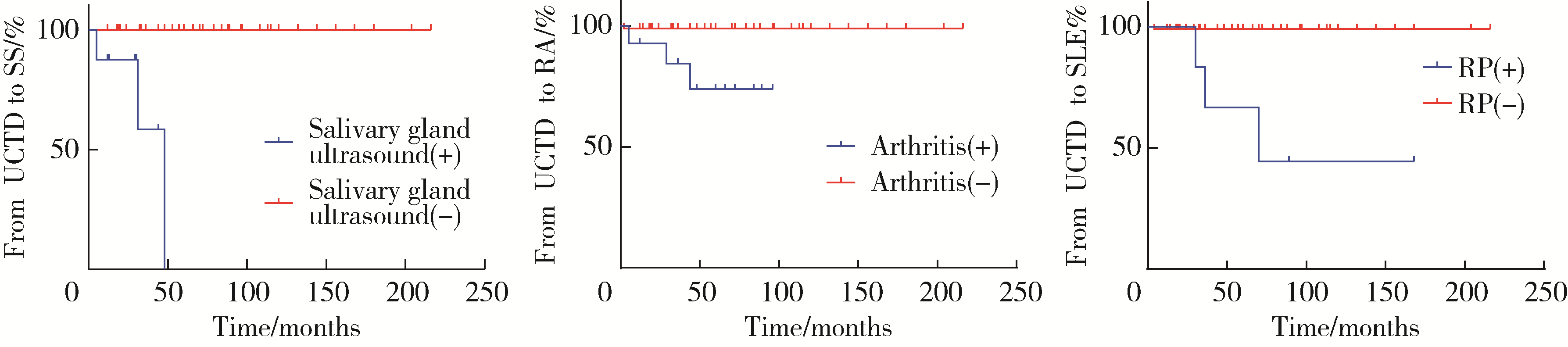
Analysis of pregnancy outcomes, disease progression, and risk factors in patients with undifferentiated connective tissue disease
Fang-ning YOU1,2,Liang LUO3,Xiang-jun LIU1,Xue-wu ZHANG1,Chun LI1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Beijing 100044, China
2. Department of Nephropathy and Rheumatology, Chongqing Hospital of Traditional Chinese Medicine, Chongqing 400011, China
3. Department of Chinese Medicine, the People's Hospital of Yubei District of Chongqing City, Chongqing 401120, China
CLC Number:
- R593.2
| 1 |
Mosca M , Tani C , Neri C , et al. Undifferentiated connective tissue diseases (UCTD)[J]. Autoimm Rev, 2006, 6 (1): 1- 4.
doi: 10.1016/j.autrev.2006.03.004 |
| 2 | García-González M , Rodríguez-Lozano B , Bustabad S , et al. Undifferentiated connective tissue disease: Predictors of evolution into definite disease[J]. Clin Exp Rheumatol, 2017, 35 (5): 739- 745. |
| 3 |
Mecacci F , Pieralli A , Bianchi B , et al. The impact of autoimmune disorders and adverse pregnancy outcome[J]. Semin Perinatol, 2007, 31 (4): 223- 226.
doi: 10.1053/j.semperi.2007.05.005 |
| 4 | Mosca M , Neri R , Bombardieri S . Undifferentiated connective tissue diseases (UCTD): A review of the literature and a proposal for preliminary classification criteria[J]. Clin Exp Rheumatol, 1999, 17 (5): 615- 620. |
| 5 |
Practice Committee of the American Society for Reproductive Medicine . Evaluation and treatment of recurrent pregnancy loss: A committee opinion[J]. Fertil Steril, 2012, 98 (5): 1103- 1111.
doi: 10.1016/j.fertnstert.2012.06.048 |
| 6 |
Vogel JP , Chawanpaiboon S , Moller AB , et al. The global epidemiology of preterm birth[J]. Best Pract Res Clin Obstet Gynaecol, 2018, 52, 3- 12.
doi: 10.1016/j.bpobgyn.2018.04.003 |
| 7 | Tyas BD , Lestari P , Akbar MIA . Maternal perinatal outcomes related to advanced maternal age in preeclampsia pregnant women[J]. J Family Reprod Health, 2019, 13 (4): 191- 200. |
| 8 |
Sharma D , Shastri S , Farahbakhsh N , et al. Intrauterine growth restriction: Part 1[J]. J Matern Fetal Neonatal Med, 2016, 29 (24): 3977- 3987.
doi: 10.3109/14767058.2016.1152249 |
| 9 |
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Obstetrics . Practice bulletin No.172: Premature rupture of membranes[J]. Obstet Gynecol, 2016, 128 (4): 165- 177.
doi: 10.1097/AOG.0000000000001712 |
| 10 | Sheldon WR , Blum J , Vogel JP , et al. Postpartum haemorrhage management, risks, and maternal outcomes: Findings from the World Health Organization Multicountry Survey on Maternal and Newborn Health[J]. BJOG, 2014, 121 (Suppl 1): 5- 13. |
| 11 |
Robinson GE . Pregnancy loss[J]. Best Pract Res Clin Obstet Gynaecol, 2014, 28 (1): 169- 178.
doi: 10.1016/j.bpobgyn.2013.08.012 |
| 12 |
Bertino E , Spada E , Occhi L , et al. Neonatal anthropometric charts: The Italian neonatal study compared with other European studies[J]. J Pediatr Gastroenterol Nutr, 2010, 51 (3): 353- 361.
doi: 10.1097/MPG.0b013e3181da213e |
| 13 |
Krasevec J , Blencowe H , Coffey C , et al. Study protocol for UNICEF and WHO estimates of global, regional, and national low birthweight prevalence for 2000 to 2020[J]. Gates Open Res, 2022, 6, 80- 93.
doi: 10.12688/gatesopenres.13666.1 |
| 14 | World Health Organization (WHO). Sixty-third world health assembly. Birth defects[R]. Geneva: WHO, 2010. |
| 15 |
Ostensen M , Andreoli L , Brucato A , et al. State of the art: Reproduction and pregnancy in rheumatic diseases[J]. Autoimmun Rev, 2015, 14 (5): 376- 386.
doi: 10.1016/j.autrev.2014.12.011 |
| 16 |
Goldenberg RL , Culhane JF , Iams JD , et al. Epidemiology and causes of preterm birth[J]. Lancet, 2008, 371 (9606): 75- 84.
doi: 10.1016/S0140-6736(08)60074-4 |
| 17 |
Radin M , Schreiber K , Cecchi I , et al. A Multicentre study of 244 pregnancies in undifferentiated connective tissue disease: Maternal/fetal outcomes and disease evolution[J]. Rheumatology (Oxford), 2020, 59 (9): 2412- 2418.
doi: 10.1093/rheumatology/kez620 |
| 18 |
Muñoz Muñoz1 C , Ahmed K , Thomas M , et al. Comparing pregnancy outcomes in patients with criteria and non-criteria autoimmune disease: A systematic review[J]. Lupus, 2022, 31 (1): 5- 18.
doi: 10.1177/09612033211061850 |
| 19 |
Haase I , Fischer-Betz R . State of the art: Fertility and pregnancy in rheumatic diseases[J]. Z Rheumatol, 2021, 80 (8): 699- 706.
doi: 10.1007/s00393-021-01073-5 |
| 20 |
Luo L , Li XR , Li C , et al. Risk factors for adverse pregnancy outcomes in women with rheumatoid arthritis and follow-up of their offspring[J]. Clin Rheumatol, 2022, 41 (10): 3135- 3141.
doi: 10.1007/s10067-022-06233-9 |
| 21 |
Erden A , Apaydın H , Fanouriakis A , et al. Performance of the systemic lupus erythematosus risk probability index in a cohort of undifferentiated connective tissue disease[J]. Rheumatology (Oxford), 2022, 61 (9): 3606- 3613.
doi: 10.1093/rheumatology/keac005 |
| 22 |
张晓英, 温鸿雁, 陈俊伟, 等. 未分化结缔组织病合并骨髓增生异常综合征1例[J]. 北京大学学报(医学版), 2012, 44 (2): 316- 319.
doi: 10.3969/j.issn.1671-167X.2012.02.033 |
| 23 |
Lin L , Wei Y , Zhu W , et al. Prevalence, risk factors and associated adverse pregnancy outcomes of anaemia in Chinese pregnant women: A multicentre retrospective study[J]. BMC Pregnancy Childbirth, 2018, 18 (1): 111- 118.
doi: 10.1186/s12884-018-1739-8 |
| 24 |
Li M , Huang SJ . Innate immunity, coagulation and placenta related adverse pregnancy outcomes[J]. Thromb Res, 2009, 124 (6): 656- 662.
doi: 10.1016/j.thromres.2009.07.012 |
| 25 | 孔德璇, 张志坤, 李慧东. 系统性红斑狼疮与孕产妇不良妊娠结局的相关性[J]. 中国妇幼保健, 2022, 37 (10): 1865- 1868. |
| 26 |
Klein A , Molad Y . Hematological manifestations among patients with rheumatic diseases[J]. Acta Haematol, 2021, 144 (4): 403- 412.
doi: 10.1159/000511759 |
| 27 |
Wang F , Jia W , Fan M , et al. Single cell immune landscape of human recurrent miscarriage[J]. Genomics Proteomics Bioinformatics, 2021, 19 (2): 208- 222.
doi: 10.1016/j.gpb.2020.11.002 |
| 28 | Cavazzana I , Franceschini F , Belfiore N , et al. Undifferentiated connective tissue disease with antibodies to Ro/SSa: Clinical features and follow-up of 148 patients[J]. Clin Exp Rheumatol, 2001, 19 (4): 403- 409. |
| 29 |
Tektonidou MG , Andreoli L , Limper M , et al. EULAR recommendations for the management of antiphospholipid syndrome in adults[J]. Ann Rheum Dis, 2019, 78 (10): 1296- 1304.
doi: 10.1136/annrheumdis-2019-215213 |
| 30 |
Duan JN , Ma D , Wen XT , et al. Hydroxychloroquine prophylaxis for preeclampsia, hypertension and prematurity in pregnant patients with systemic lupus erythematosus: A meta-analysis[J]. Lupus, 2021, 30 (7): 1163- 1174.
doi: 10.1177/09612033211007199 |
| [1] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [2] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [3] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [4] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [5] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [6] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [7] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
| [8] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [9] | Jinrong ZHU,Yana ZHAO,Wei HUANG,Weiwei ZHAO,Yue WANG,Song WANG,Chunyan SU. Clinical characteristics of COVID-19 infection in patients undergoing hemodialysis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 267-272. |
| [10] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [11] | Xiaoqian SI,Xiujuan ZHAO,Fengxue ZHU,Tianbing WANG. Risk factors for acute respiratory distress syndrome in patients with traumatic hemorrhagic shock [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 307-312. |
| [12] | Yangyang LI,Lin HOU,Zijun MA,Shanyamei HUANG,Jie LIU,Chaomei ZENG,Jiong QIN. Association of pregnancy factors with cow's milk protein allergy in infants [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 144-149. |
| [13] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [14] | Liang LUO,Yun LI,Hong-yan WANG,Xiao-hong XIANG,Jing ZHAO,Feng SUN,Xiao-ying ZHANG,Ru-lin JIA,Chun LI. Anti-endothelial cell antibodies in predicting early miscarriage [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1039-1044. |
| [15] | Yu-fei LI,Ya-ni YAN,Jia-yang JIN,Chun LI,Qiu-yan PEI. Clinical characteristics of fetal cardiac disease in patients with anti-SSA antibody positive [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1053-1057. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 193
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 322
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||