Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 1039-1044. doi: 10.19723/j.issn.1671-167X.2023.06.013
Previous Articles Next Articles
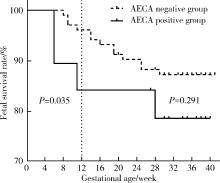
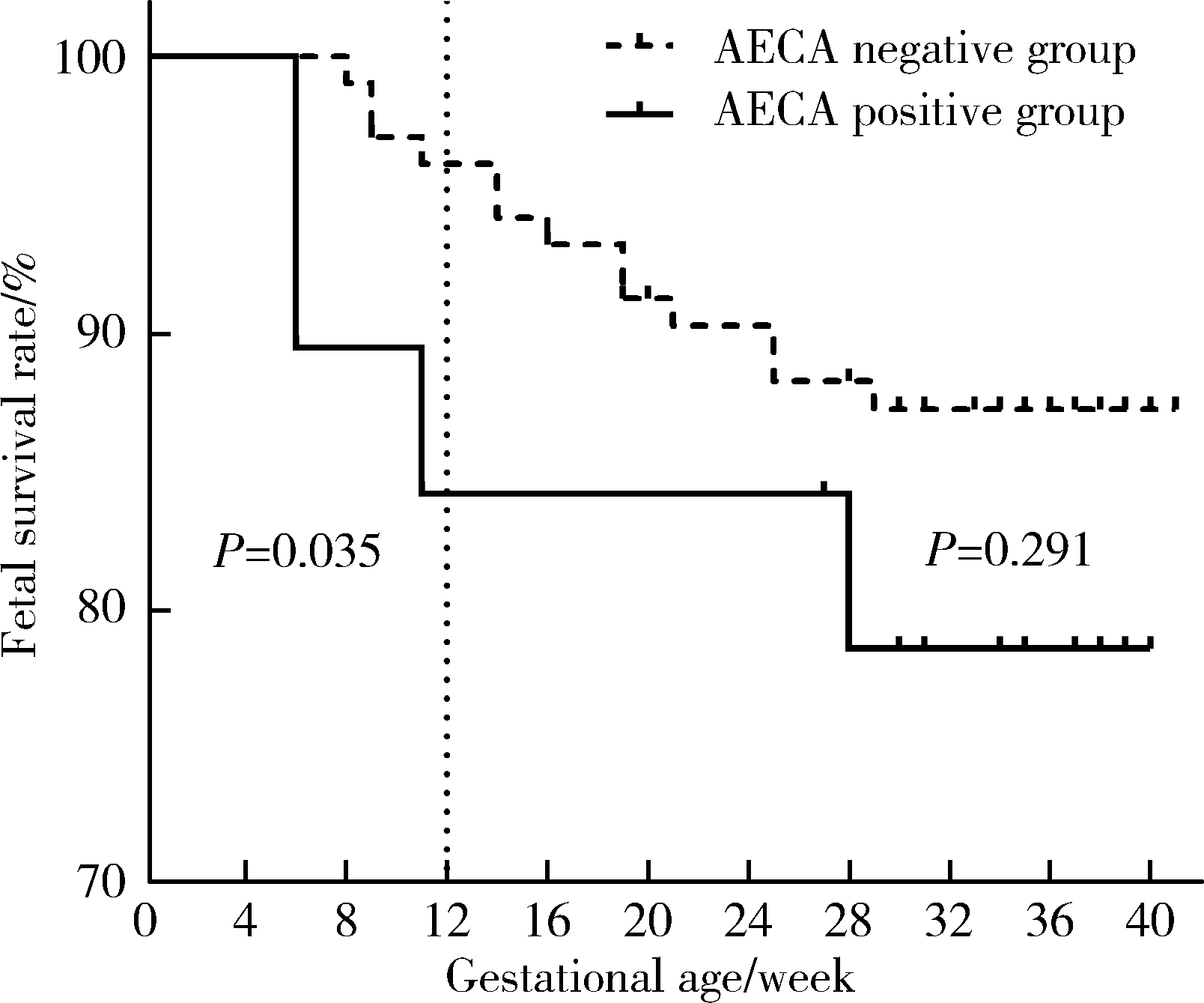
Anti-endothelial cell antibodies in predicting early miscarriage
Liang LUO1,2,Yun LI1,Hong-yan WANG1,Xiao-hong XIANG1,Jing ZHAO1,Feng SUN1,Xiao-ying ZHANG1,*( ),Ru-lin JIA1,*(
),Ru-lin JIA1,*( ),Chun LI1
),Chun LI1
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Beijing 100044, China
2. Department of Chinese Medicine, the People's Hospital of Yubei District of Chongqing City, Chongqing 401120, China
CLC Number:
- R593.2
| 1 |
Madendag IC , Sahin ME , Madendag Y , et al. Evaluation of the levels of secretory leukocyte protease inhibitor in the cervical mucus of women with unexplained infertility[J]. J Obstet Gynaecol Res, 2020, 46 (7): 1128- 1132.
doi: 10.1111/jog.14299 |
| 2 |
Yang XL , Chen F , Yang XY , et al. Efficacy of low-molecular-weight heparin on the outcomes of in vitro fertilization/intracytoplasmic sperm injection pregnancy in non-thrombophilic women: A meta-analysis[J]. Acta Obstet Gynecol Scand, 2018, 97 (9): 1061- 1072.
doi: 10.1111/aogs.13359 |
| 3 |
Quenby S , Gallos ID , Dhillon-Smith RK , et al. Miscarriage matters: The epidemiological, physical, psychological, and economic costs of early pregnancy loss[J]. Lancet, 2021, 397 (10285): 1658- 1667.
doi: 10.1016/S0140-6736(21)00682-6 |
| 4 |
Jiang L , Xu X , Cao Z , et al. Comparison of frozen embryo transfer outcomes between uterine infusion of granulocyte colony-stimulating factor and growth hormone application in patients with thin endometrium: A retrospective study[J]. Front Endocrinol (Lausanne), 2021, 12, 725202.
doi: 10.3389/fendo.2021.725202 |
| 5 |
Qu P , Yan M , Zhao D , et al. Association between pre-pregnancy body mass index and miscarriage in an assisted reproductive technology population: A 10-year cohort study[J]. Front Endocrinol (Lausanne), 2021, 12, 646162.
doi: 10.3389/fendo.2021.646162 |
| 6 |
Shankarkumar U , Pradhan VD , Patwardhan MM , et al. Autoantibody profile and other immunological parameters in recurrent spontaneous abortion patients[J]. Niger Med J, 2011, 52 (3): 163- 166.
doi: 10.4103/0300-1652.86126 |
| 7 | Lindqvist KJ , Osterland CK . Human antibodies to vascular endothelium[J]. Clin Exp Immunol, 1971, 9 (6): 753- 760. |
| 8 | Alessandri C , Bombardieri M , Valesini G . Pathogenic mechanisms of anti-endothelial cell antibodies (AECA): Their prevalence and clinical relevance[J]. Adv Clin Chem, 2006, 42, 297- 326. |
| 9 | 杜欣莹, 管立学, 王美, 等. 血清抗内皮细胞抗体定量分析与复发性自然流产相关性研究[J]. 中国优生与遗传杂志, 2009, 17 (6): 23- 25. |
| 10 |
Cacciola R , Gentilini Cacciola E , Vecchio V , et al. Impact of anti-endothelial cell antibodies (AECAs) in patients with polycythemia vera and thrombosis[J]. Diagnostics (Basel), 2022, 12 (5): 1077.
doi: 10.3390/diagnostics12051077 |
| 11 |
Roussev RG , Stern JJ , Kaider BD . Anti-endothelial cell antibo-dies: Another cause for pregnancy loss?[J]. Am J Reprod Immunol, 1998, 39 (2): 89- 95.
doi: 10.1111/j.1600-0897.1998.tb00340.x |
| 12 | 蒋莎, 李娜, 张杨, 等. Toll样受体4通过调节性T细胞引起不明原因复发性流产的机制研究进展[J]. 中华生殖与避孕杂志, 2018, 38 (10): 6. |
| 13 |
Zilla P , von Oppell U , Deutsch M . The endothelium: A key to the future[J]. J Card Surg, 1993, 8 (1): 32- 60.
doi: 10.1111/j.1540-8191.1993.tb00574.x |
| 14 |
Youinou P , Le Dantec C , Bendaoud B , et al. Endothelium, a target for immune-mediated assault in connective tissue disease[J]. Autoimmun Rev, 2006, 5 (3): 222- 228.
doi: 10.1016/j.autrev.2005.06.012 |
| 15 | 张梦莹, 李志, 吕坤, 等. 系统性红斑狼疮患者血清抗内皮细胞抗体和抗β2糖蛋白Ⅰ抗体水平及其对人脐静脉内皮细胞增殖的影响[J]. 中国临床药理学与治疗学, 2013, 18 (2): 142- 146. |
| 16 | Hussain M , Chen P , Zhang Y , et al. Moesin expression is correlated with its involvement in patients with Behcet' s disease[J]. Arch Med Sci, 2020, 16 (4): 924- 930. |
| 17 | Mutoh T , Shirai T , Ishii T , et al. Identification of two major autoantigens negatively regulating endothelial activation in Takayasu arteritis[J]. Nat Commun, 2020, 11 (1): 1253. |
| 18 | Meyer O , Kaiser P , Haim T , et al. Anti-vascular endothelial cell antibodies (AECA): Comparison of two assay methods and clinical applications[J]. Rev Rhum Engl Ed, 1995, 62 (11): 737- 747. |
| 19 | Blank M , Krause I , Goldkorn T , et al. Monoclonal anti-endothe-lial cell antibodies from a patient with Takayasu arteritis activate endothelial cells from large vessels[J]. Arthritis Rheum, 1999, 42 (7): 1421- 1432. |
| 20 | Thomas AM , Gerogianni A , McAdam MB , et al. Complement component C5 and TLR molecule CD14 mediate heme-induced thromboinflammation in human blood[J]. J Immunol, 2019, 203 (6): 1571- 1578. |
| 21 | Belizna C , Duijvestijn A , Hamidou M , et al. Antiendothelial cell antibodies in vasculitis and connective tissue disease[J]. Ann Rheum Dis, 2006, 65 (12): 1545- 1550. |
| 22 | 母洪洪, 张湘燕, 张程. 抗内皮细胞抗体检测临床应用研究进展[J]. 现代医药卫生, 2020, 36 (30): 374- 376. |
| 23 | Akhtar MA , Agrawal R , Brown J , et al. Thyroxine replacement for subfertile women with euthyroid autoimmune thyroid disease or subclinical hypothyroidism[J]. Cochrane Database Syst Rev, 2019, 6 (6): CD011009. |
| 24 | Arachchillage D , Pericleous C . Evolution of antiphospholipid syndrome[J]. Semin Thromb Hemost, 2023, 49 (3): 295- 304. |
| 25 | Poorolajal J , Cheraghi P , Cheraghi Z , et al. Predictors of miscarriage: A matched case-control study[J]. Epidemiol Health, 2014, 36, e2014031. |
| 26 | Walter K . Early pregnancy loss[J]. JAMA, 2023, 329 (16): 1426. |
| [1] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [2] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [3] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [4] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [5] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [6] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [7] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
| [8] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [9] | Jinrong ZHU,Yana ZHAO,Wei HUANG,Weiwei ZHAO,Yue WANG,Song WANG,Chunyan SU. Clinical characteristics of COVID-19 infection in patients undergoing hemodialysis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 267-272. |
| [10] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [11] | Xiaoqian SI,Xiujuan ZHAO,Fengxue ZHU,Tianbing WANG. Risk factors for acute respiratory distress syndrome in patients with traumatic hemorrhagic shock [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 307-312. |
| [12] | Yangyang LI,Lin HOU,Zijun MA,Shanyamei HUANG,Jie LIU,Chaomei ZENG,Jiong QIN. Association of pregnancy factors with cow's milk protein allergy in infants [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 144-149. |
| [13] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [14] | Yu-fei LI,Ya-ni YAN,Jia-yang JIN,Chun LI,Qiu-yan PEI. Clinical characteristics of fetal cardiac disease in patients with anti-SSA antibody positive [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1053-1057. |
| [15] | Hui WEI, Ci-dan-yang-zong, Yi-xi-la-mu, Bai-ma-yang-jin. Risk factors associated with different types of Henoch-Schönlein purpura in Tibetan patients at high altitude [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 923-928. |
|
||