Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 492-499. doi: 10.19723/j.issn.1671-167X.2020.03.015
Previous Articles Next Articles
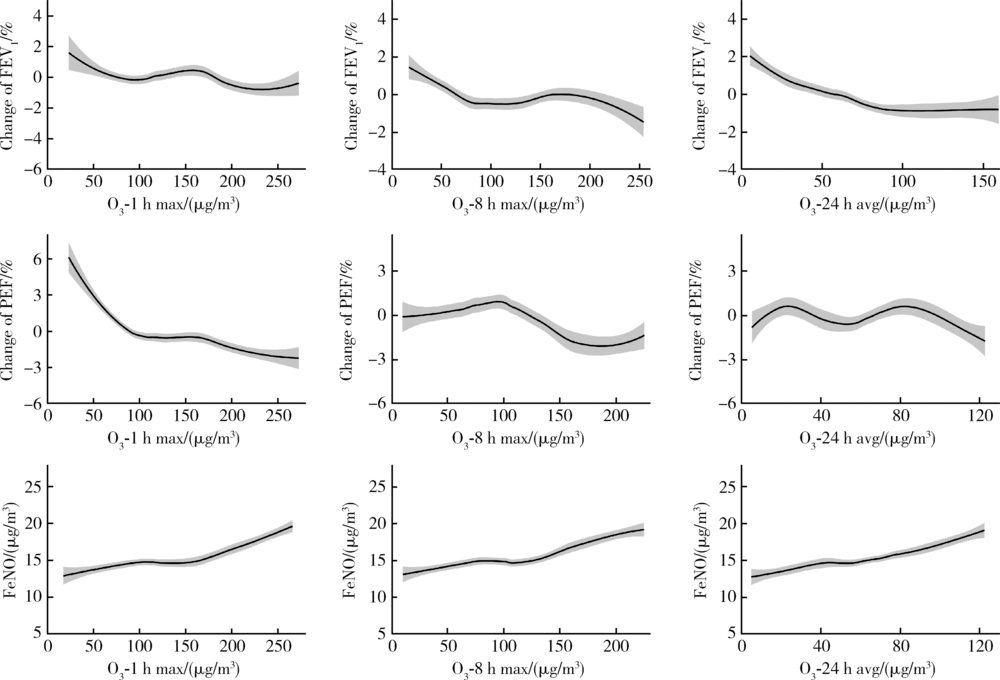
Monitoring metrics for short-term exposure to ambient ozone and pulmonary function and airway inflammation in healthy young adults
Jia-hui CHEN,Da-yu HU,Xu JIA,Wei NIU,Fu-rong DENG,Xin-biao GUO( )
)
- Department of Occupational and Environmental Health Sciences, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- X5
| [1] |
Dales R, Chen L, Frescura AM, et al. Acute effects of outdoor air pollution on forced expiratory volume in 1 s: a panel study of schoolchildren with asthma[J]. Eur Respir J, 2009,34(2):316-323.
doi: 10.1183/09031936.00138908 |
| [2] | 邸沂遥. 空气污染对哮喘患者肺功能、FeNO和血清IgE水平的影响[D]. 石家庄: 河北医科大学, 2016. |
| [3] |
Sinharay R, Gong J, Barratt B, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study[J]. Lancet, 2018,391(10118):339-349.
doi: 10.1016/S0140-6736(17)32643-0 pmid: 29221643 |
| [4] |
Yoda Y, Otani N, Sakurai S, et al. Acute effects of summer air pollution on pulmonary function and airway inflammation in healthy young women[J]. J Epidemiol, 2014,24(4):312-320.
pmid: 24857953 |
| [5] |
Bai L, Su X, Zhao D, et al. Exposure to traffic-related air pollution and acute bronchitis in children: season and age as modifiers[J]. J Epidemiol Community Health, 2018,72(5):426-433.
pmid: 29440305 |
| [6] |
Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015[J]. Lancet, 2017,389(10082):1907-1918.
doi: 10.1016/S0140-6736(17)30505-6 pmid: 28408086 |
| [7] | 崔娟, 王黎君. 1990年与2013年中国大气臭氧污染导致慢性阻塞性肺疾病的疾病负担分析[J]. 中华预防医学杂志, 2016,50(5):391-396. |
| [8] |
Guo Y, Zeng H, Zheng R, et al. The association between lung cancer incidence and ambient air pollution in China: a spatiotemporal analysis[J]. Environ Res, 2016,144(Pt A):60-65.
pmid: 26562043 |
| [9] |
Yang C, Yang H, Guo S, et al. Alternative ozone metrics and daily mortality in Suzhou: the China air pollution and health effects study (CAPES)[J]. Sci Total Environ, 2012,426:83-89.
doi: 10.1016/j.scitotenv.2012.03.036 pmid: 22521098 |
| [10] | Tolbert PE, Klein M, Metzger KB, et al. Interim results of the study of particulates and health in Atlanta (SOPHIA)[J]. J Expo Anal Environ Epidemiol, 2000,10(5):446-460. |
| [11] |
Li H, Wu S, Pan L, et al. Short-term effects of various ozone metrics on cardiopulmonary function in chronic obstructive pulmonary disease patients: results from a panel study in Beijing, China[J]. Environ Pollut, 2018,232:358-366.
doi: 10.1016/j.envpol.2017.09.030 pmid: 28987568 |
| [12] |
Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study[J]. Epidemiology, 2005,16(4):436-445.
doi: 10.1097/01.ede.0000165817.40152.85 pmid: 15951661 |
| [13] |
Thurston GD, Ito K. Epidemiological studies of acute ozone exposures and mortality[J]. J Expo Anal Environ Epidemiol, 2001,11(4):286-294.
pmid: 11571608 |
| [14] |
Anderson GB, Bell ML. Does one size fit all? The suitability of standard ozone exposure metric conversion ratios and implications for epidemiology[J]. J Expo Sci Environ Epidemiol, 2010,20(1):2-11.
doi: 10.1038/jes.2008.69 pmid: 18985076 |
| [15] |
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry[J]. Eur Respir J, 2005,26(2):319-338.
doi: 10.1183/09031936.05.00034805 pmid: 16055882 |
| [16] |
ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005[J]. Am J Respir Crit Care Med, 2005,171(8):912-930.
doi: 10.1164/rccm.200406-710ST pmid: 15817806 |
| [17] | 王亭槐. 生理学[M]. 9版. 北京: 人民卫生出版社, 2018: 156. |
| [18] |
Adman MA, Hashim JH, Manaf MRA, et al. Associations between air pollutants and peak expiratory flow and fractional exhaled nitric oxide in students[J]. Int J Tuberc Lung Dis, 2020,24(2):189-195.
doi: 10.5588/ijtld.19.0096 pmid: 32127103 |
| [19] | 杨克敌. 环境卫生学[M]. 8版. 北京: 人民卫生出版社, 2017: 95. |
| [20] |
Huang J, Song Y, Chu M, et al. Cardiorespiratory responses to low-level ozone exposure: the in door ozone study in children (DOSE)[J]. Environ Int, 2019,131:105021.
pmid: 31349208 |
| [21] |
Altug H, Gaga EO, Dogeroglu T, et al. Effects of ambient air pollution on respiratory tract complaints and airway inflammation in primary school children[J]. Sci Total Environ, 2014,479/480:201-209.
doi: 10.1016/j.scitotenv.2014.01.127 |
| [22] | 张嘉尧. 臭氧对人群的急性健康影响研究[D]. 南京: 南京医科大学, 2019. |
| [23] |
Zhang J, Sun H, Chen Q, et al. Effects of individual ozone exposure on lung function in the elderly: a cross-sectional study in China[J]. Environ Sci Pollut Res Int, 2019,26(12):11690-11695.
doi: 10.1007/s11356-019-04324-w pmid: 30806931 |
| [24] |
Devlin RB, Duncan KE, Jardim M, et al. Controlled exposure of healthy young volunteers to ozone causes cardiovascular effects[J]. Circulation, 2012,126(1):104-111.
doi: 10.1161/CIRCULATIONAHA.112.094359 pmid: 22732313 |
| [25] |
Kariisa M, Foraker R, Pennell M, et al. Short- and long-term effects of ambient ozone and fine particulate matter on the respiratory health of chronic obstructive pulmonary disease subjects[J]. Arch Environ Occup Health, 2015,70(1):56-62.
doi: 10.1080/19338244.2014.932753 pmid: 25136856 |
| [26] | 赵丽敏, 马利军. 呼出气一氧化氮检测及临床意义[J]. 中华实用诊断与治疗杂志, 2011,25(5):422-423. |
| [27] |
Nickmilder M, de Burbure C, Carbonnelle S, et al. Increase of exhaled nitric oxide in children exposed to low levels of ambient ozone[J]. J Toxicol Environ Health A, 2007,70(3-4):270-274.
doi: 10.1080/15287390600884834 pmid: 17365589 |
| [28] |
Berhane K, Zhang Y, Linn WS, et al. The effect of ambient air pollution on exhaled nitric oxide in the children’s health study[J]. Eur Respir J, 2011,37(5):1029-1036.
doi: 10.1183/09031936.00081410 pmid: 20947676 |
| [29] |
Day DB, Xiang J, Mo J, et al. Association of ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults[J]. JAMA Intern Med, 2017,177(9):1344-1353.
doi: 10.1001/jamainternmed.2017.2842 pmid: 28715576 |
| [30] |
Bell ML, Hobbs BF, Ellis H. Metrics matter: conflicting air quality rankings from different indices of air pollution[J]. J Air Waste Manag Assoc, 2005,55(1):97-106.
doi: 10.1080/10473289.2005.10464596 pmid: 15704544 |
| [1] | Tenglong YAN,Jiayu XU,Tian CHEN,Xin YANG,Weiwei WANG,Shupei ZHOU,Piye NIU,Guang JIA,Jiao XIA. Effects of PM2.5 and O3 sub-chronic combined exposure on ATP amount and ATPase activities in rat nasal mucosa [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 687-692. |
| [2] | ZHANG Hong,DONG Ji-yuan,WANG Jian-jun,FAN Lin-xia,QU Qiang,LIU Yang. Short-term effects and seasonal variation of ozone on daily hospital outpatient visits for childhood asthma in Lanzhou [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 227-235. |
| [3] | Jia-xing LIU,Gui-ping HU,Lin ZHAO,Yong-ming ZHANG,Li WANG,Guang JIA,Rui-xiang LIU,Hui-min FENG,Hua-dong XU. Early effects of low-level long-term occupational chromate exposure on workers’ health [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 307-314. |
| [4] | GAO Xin, SHANG Jing, YANG Jing-Lin, LI Qian, CHEN Tian, PANG Yuan-Jie, ZHANG Wen-Xiao, LUAN Xian-Guo, ZHU Tong, JIA Guang. Comparison of genetic damage in mice exposed to black carbon and ozone-oxidized black carbon [J]. Journal of Peking University(Health Sciences), 2014, 46(3): 400-404. |
|
||