Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (4): 614-620. doi: 10.19723/j.issn.1671-167X.2020.04.003
Previous Articles Next Articles
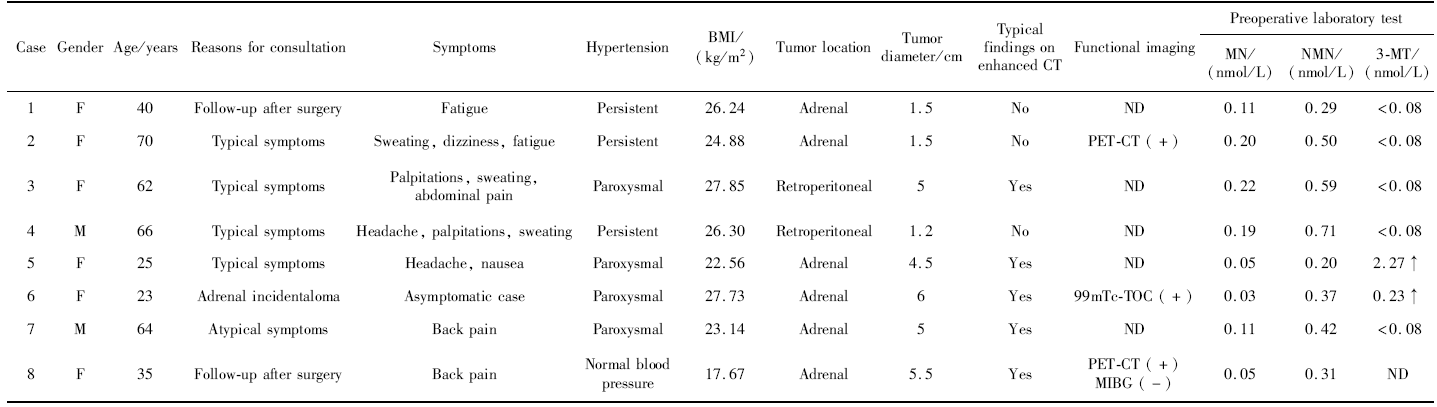
Clinical profile of pheochromocytoma and paraganglioma with normal plasma free metanephrines
Lu LIU1,Jie TIAN2,Kai WU1,Ying GAO1,△( ),Zheng ZHANG2,△(
),Zheng ZHANG2,△( ),Jun-qing ZHANG1,Xiao-hui GUO1
),Jun-qing ZHANG1,Xiao-hui GUO1
- 1. Department of Endocrinology, Peking University First Hospital, Beijing 100034, China
2. Department of Urology, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R736
| [1] |
Lenders JW, Pacak K, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: which test is best[J]. JAMA, 2002,287(11):1427-1434.
doi: 10.1001/jama.287.11.1427 pmid: 11903030 |
| [2] |
Unger N, Pitt C, Schmidt IL, et al. Diagnostic value of various biochemical parameters for the diagnosis of pheochromocytoma in patients with adrenal mass[J]. Eur J Endocrinol, 2006,154(3):409-417.
pmid: 16498054 |
| [3] | Hickman PE, Leong M, Chang J, et al. Plasma free metanephrines are superior to urine and plasma catecholamines and urine catecholamine metabolites for the investigation of phaeochromocytoma[J]. Pathology, 2009,41(2):173-177. |
| [4] |
Grouzmann E, Drouard-Troalen L, Baudin E, et al. Diagnostic accuracy of free and total metanephrines in plasma and fractionated metanephrines in urine of patients with pheochromocytoma[J]. Eur J Endocrinol, 2010,162(5):951-960.
pmid: 20142367 |
| [5] |
Unger N, Hinrichs J, Deutschbein T, et al. Plasma and urinary metanephrines determined by an enzyme immunoassay, but not serum chromogranin A for the diagnosis of pheochromocytoma in patients with adrenal mass[J]. Exp Clin Endocrinol Diabetes, 2012,120(8):494-500.
doi: 10.1055/s-0032-1309007 pmid: 22696168 |
| [6] | Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2014,99(6):1915-1942. |
| [7] | 中华医学会内分泌学分会肾上腺学组. 嗜铬细胞瘤和副神经节瘤诊断治疗的专家共识[J]. 中华内分泌代谢杂志, 2016,32(3):181-187. |
| [8] | Plouin PF, Amar L, Dekkers OM, et al. European society of endocrinology clinical practice guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma[J]. Eur J Endocrinol, 2016,174(5):G1-G10. |
| [9] |
Bozin M, Lamb A, Putra LJ. Pheochromocytoma with negative metanephrines: a rarity and the significance of dopamine secreting tumors[J]. Urol Case Rep, 2017,12:51-53.
pmid: 28337414 |
| [10] | 曹万里, 黄宝星, 成康, 等. 血浆游离甲氧肾上腺素和甲氧基去甲肾上腺素正常的嗜铬细胞瘤/副神经节瘤患者的临床特点[J]. 中华临床医师杂志: 电子版, 2015,9(2):200-205. |
| [11] | 刘颖姝, 李乐乐, 窦京涛, 等. 偶发嗜铬细胞瘤患者术中血流动力学变化的相关因素[J]. 中华医学杂志, 2018,98(36):2905-2909. |
| [12] | Poudyal S, Pradhan M, Chapagain S, et al. Marker-negative pheochromocytoma associated with inferior vena cava thrombosis[J/OL]. Case Rep Urol, 2017, 2017: 6270436(2017-06-15)[2020-03-01]. https://www.hindawi.com/journals/criu/2017/6270436/. |
| [13] |
Lopez-Gomez J, Salazar-Alvarez MA, Adame RY, et al. Metasta-tic pheochromocytoma to liver without elevation of metanephrines and catecholamines[J]. Int J Surg Case Rep, 2016,29:71-75.
pmid: 27821293 |
| [14] | Kota SK, Kota SK, Panda S, et al. Pheochromocytoma: an uncommon presentation of an asymptomatic and biochemically silent adrenal incidentaloma[J]. Malays J Med Sci, 2012,19(2):86-91. |
| [15] |
Heavner MG, Krane LS, Winters SM, et al. Pheochromocytoma diagnosed pathologically with previous negative serum markers[J]. J Surg Oncol, 2015,112(5):492-495.
pmid: 26384104 |
| [16] |
Eisenhofer G, Lenders JW, Goldstein DS, et al. Pheochromocytoma catecholamine phenotypes and prediction of tumor size and location by use of plasma free metanephrines[J]. Clin Chem, 2005,51(4):735-744.
pmid: 15718487 |
| [17] |
Pillai D, Ross HA, Kratzsch J, et al. Proficiency test of plasma free and total metanephrines: report from a study group[J]. Clin Chem Lab Med, 2009,47(6):786-790.
pmid: 19445649 |
| [18] | Pillai D, Callen S. Pilot quality assurance programme for plasma metanephrines[J]. Ann Clin Biochem, 2010,47(Pt 2):137-142. |
| [1] | Xinxin CHEN, Zhe TANG, Yanchun QIAO, Wensheng RONG. Caries experience and its correlation with caries activity of 4-year-old children in Miyun District of Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 833-838. |
| [2] | Hua ZHONG, Yuan LI, Liling XU, Mingxin BAI, Yin SU. Application of 18F-FDG PET/CT in rheumatic diseases [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 853-859. |
| [3] | Zhengfang LI,Cainan LUO,Lijun WU,Xue WU,Xinyan MENG,Xiaomei CHEN,Yamei SHI,Yan ZHONG. Application value of anti-carbamylated protein antibody in the diagnosis of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 729-734. |
| [4] | Hai-hong YAO,Fan YANG,Su-mei TANG,Xia ZHANG,Jing HE,Yuan JIA. Clinical characteristics and diagnostic indicators of macrophage activation syndrome in patients with systemic lupus erythematosus and adult-onset Still's disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 966-974. |
| [5] | Yan XIONG,Xin LI,Li LIANG,Dong LI,Li-min YAN,Xue-ying LI,Ji-ting DI,Ting LI. Evaluation of accuracy of pathological diagnosis based on thyroid core needle biopsy [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 234-242. |
| [6] | Xue-mei HA,Yong-zheng YAO,Li-hua SUN,Chun-yang XIN,Yan XIONG. Solid placental transmogrification of the lung: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 357-361. |
| [7] | Bo-han NING,Qing-xia ZHANG,Hui YANG,Ying DONG. Endometrioid adenocarcinoma with proliferated stromal cells, hyalinization and cord-like formations: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 366-369. |
| [8] | Rui-jie CAO,Zhong-qiang YAO,Peng-qing JIAO,Li-gang CUI. Comparison of diagnostic efficacy of different classification criteria for Takayasu arteritis in Chinese patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1128-1133. |
| [9] | Zhe HAO,Shu-hua YUE,Li-qun ZHOU. Application of Raman-based technologies in the detection of urological tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 779-784. |
| [10] | Bo YU,Yang-yu ZHAO,Zhe ZHANG,Yong-qing WANG. Infective endocarditis in pregnancy: A case report [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 578-580. |
| [11] | MENG Guang-yan,ZHANG Yun-xiao,ZHANG Yu-xin,LIU Yan-ying. Clinical characteristics of central nervous system involvement in IgG4 related diseases [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1043-1048. |
| [12] | ZHAI Li,QIU Nan,SONG Hui. Multicentric reticulohistiocytosis: A case report [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1183-1187. |
| [13] | LIU Lei,QIN Yan-chun,WANG Guo-liang,ZHANG Shu-dong,HOU Xiao-fei,MA Lu-lin. Strategy of reoperation for pheochromocytoma and paraganglioma [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 793-797. |
| [14] | YUAN Yuan,LANG Ning,YUAN Hui-shu. CT spectral curve in differentiating spinal tumor metastasis and infections [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 183-187. |
| [15] | Qi KANG,Ji-xin ZHANG,Ying GAO,Jun-qing ZHANG,Xiao-hui GUO. Analysis of diagnosis and treatment of 100 patients with Hürthle cell adenoma [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1098-1101. |
|
||