Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (3): 523-529. doi: 10.19723/j.issn.1671-167X.2021.03.014
Previous Articles Next Articles
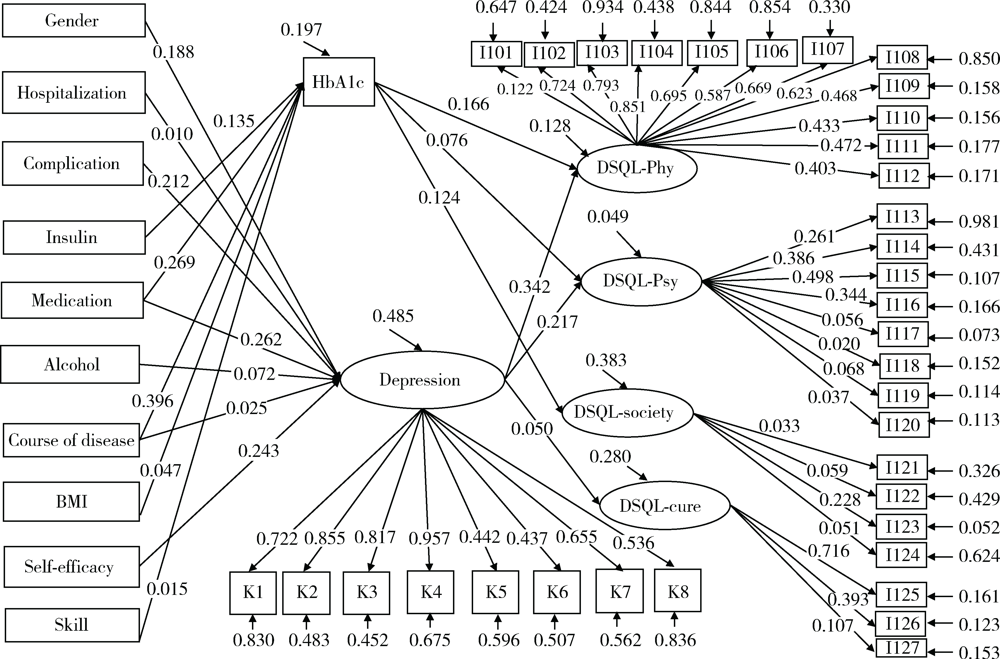
Factors associated with quality of life in 747 patients with type 2 diabetes in Tongzhou District and Shunyi District of Beijing
FAN Li-shi1,GAO Min1,Edwin B. FISHER2,SUN Xin-ying1,Δ( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. Department of Health Behavior, Gillings School of Global Public Health, University of North Carolina-Chapel Hill, North Carolina 27599-7440, USA
CLC Number:
- R587.1
| [1] |
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications[J]. Nat Rev Endocrinol, 2018,14(2):88-98.
doi: 10.1038/nrendo.2017.151 pmid: 29219149 |
| [2] | Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study[J]. BMJ, 2020,369:m997. |
| [3] | 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华内分泌代谢杂志, 2021,37(4):311-398. |
| [4] | 高蕾莉, 纪立农, 陆菊明, 等. 2009—2012年我国2型糖尿病患者药物治疗与血糖控制状况调查[J]. 中国糖尿病杂志, 2014,22(7):594-598. |
| [5] | Bajaj S. RSSDI clinical practice recommendations for the management of type 2 diabetes mellitus 2017[J]. Int J Diabetes Dev Ctries, 2018,38(Suppl 1):1-115. |
| [6] | 许燕川, 马米果, 黄小碟. 543例糖尿病患者生活质量及其影响因素调查分析[J]. 预防医学情报杂志, 2020,36(9):1222-1227. |
| [7] | 王冯彬, 高敏, 陈雪莹, 等. 社区2型糖尿病患者家庭支持与饮食行为的相关性研究[J]. 中国健康教育, 2020,36(4):300-304. |
| [8] | 高敏, 陈雪莹, 孙信, 等. 2型糖尿病患者的抑郁症状与人格特质和运动行为的关系[J]. 中国心理卫生杂志, 2021,35(4):271-276. |
| [9] | 中华医学会糖尿病学分会, 中华医学会内分泌学分会. 中国成人2型糖尿病患者糖化血红蛋白控制目标及达标策略专家共识[J]. 中华糖尿病杂志, 2020,12(1):1-12. |
| [10] | 庄鵷, 田冰洁, 王绮, 等. 老年2型糖尿病患者生存质量现状及影响因素研究[J]. 上海护理, 2021,21(2):30-34. |
| [11] | 汪爱茹, 唐婷婷, 周珈瑀, 等. 2型糖尿病患者心理状况和生存质量的相关性研究[J]. 四川医学, 2020,41(4):407-411. |
| [12] | 姜乾金. 应激(压力)系统模型:理论与实践[C]// 中国心理学会. 第十七届全国心理学学术会议论文摘要集. 北京: 中国心理学会, 2014: 1. |
| [13] | 许国敏, 程煜. 动态血糖监测联合心理疏导对2型糖尿病患者血糖控制、负性情绪及生活质量的影响[J]. 中国健康心理学杂志, 2020,28(12):1797-1802. |
| [14] |
Wong MC, Wu CH, Wang HH, et al. Association between the 8-item Morisky medication adherence scale (MMAS-8) score and glycaemic control among Chinese diabetes patients[J]. J Clin Pharmacol, 2015,55(3):279-287.
doi: 10.1002/jcph.v55.3 |
| [15] | 曹昭春. 上海市社区2型糖尿病患者血糖控制现况及影响因素分析[D]. 上海: 上海交通大学, 2019. |
| [16] | 李玉东. 南阳地区空巢老年糖尿病患者自我管理水平与生活质量相关性研究[J]. 护士进修杂志, 2019,34(13):1228-1230, 1243. |
| [17] | 蒋明晖, 张桥, 朱汝霞, 等. 南宁城乡2型糖尿病患者生存质量及其影响因素分析[J]. 右江民族医学院学报, 2018,40(4):359-362. |
| [18] | 李黎, 黄少冰, 陈焕萍, 等. 珠海市某基层医院2型糖尿病患者生活质量调查及其影响因素分析[J]. 中国当代医药, 2020,27(12):156-158. |
| [19] | 刘芳, 张英娴, 卫海燕. 1型糖尿病儿童血糖控制及生活质量状况调查[J]. 滨州医学院学报, 2019,42(1):24-26. |
| [20] | 王吉英, 肖光青, 王彦, 等. 社区糖尿病患者自我管理现状和护理指导需求的影响因素分析[J]. 中华现代护理杂志, 2020,26(15):2061-2065. |
| [21] | 姚静静, 孙强, 李奇, 等. 2型糖尿病患者自我效能与服药依从性关系[J]. 中国公共卫生, 2019,35(11):1471-1473. |
| [22] |
van Dooren FE, Denollet J, Verhey FR, et al. Psychological and personality factors in type 2 diabetes mellitus, presenting the rationale and exploratory results from The Maastricht Study, a population-based cohort study[J]. BMC Psychiatry, 2016,16:17.
doi: 10.1186/s12888-016-0722-z pmid: 26817600 |
| [1] | Min WANG, Qian LI. Path analysis of influencing factors of mental resilience in adolescents with depression [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 809-814. |
| [2] | Huameng TANG,Dianqi YUAN,Mingxing WANG,Hanbing YANG,Chao GUO. Sequential mediating role of digital participation and health lifestyle in the relationship between socioeconomic status and depression of older adults [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 230-238. |
| [3] | Jin-hui LAI,Qi WANG,Jia-xiang JI,Ming-rui WANG,Xin-wei TANG,Ke-xin XU,Tao XU,Hao HU. Effects of delayed ureteral stents removal during the COVID-19 pandemic on the quality of life and psychological status of postoperative patients with urinary calculi [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 857-864. |
| [4] | Wen YUAN,Yi ZHANG,Li CHEN,Jia-nuo JIANG,Man-man CHEN,Jie-yu LIU,Tao MA,Qi MA,Meng-jie CUI,Tong-jun GUO,Xin-xin WANG,Yan-hui DONG,Jun MA. Association of body fat distribution with depression and social anxiety in children and adolescents: A cross-sectional study based on dual-energy X-ray detection [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 429-435. |
| [5] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1086-1093. |
| [6] | WANG Jia-wen,LIU Jing-chao,MENG Ling-feng,ZHANG Wei,LIU Xiao-dong,ZHANG Yao-guang. Quality of life and related factors in patients with interstitial cystitis/bladder pain syndrome [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 653-658. |
| [7] | Yi-fan WANG,Zhen FAN,Yao-bin CHENG,Yue-bo JIN,Yang HUO,Jing HE. Investigation of sleep disturbance and related factors in patients with primary Sjögren’s syndrome [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1063-1068. |
| [8] | Yan GENG,Zhi-bo SONG,Xiao-hui ZHANG,Xue-rong DENG,Yu WANG,Zhuo-li ZHANG. Depression and anxiety in patients with psoriatic arthritis: Prevalence and associated factors [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1048-1055. |
| [9] | Duan YI,Wei ZHU,Xiu-li MENG,Xiao-guang LIU,Shui-qing LI,Bin ZHU,Dong-lin JIA. Analysis of anxiety, depression and related factors in patients with chronic lumbocrural pain before minimally invasive surgery [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 285-289. |
| [10] | Xin-yan CHE,Shi-liang WU,Yu-ke CHEN,Yan-bo HUANG,Yang YANG. A survey of risk factors and quality of life in female medical staff with urinary incontinence [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 706-710. |
| [11] | Li WANG,Chao GAO,Di ZHU,Li-hong CHEN. Effect of functional exercises on patients with rheumatoid arthritis: a meta-analysis [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 991-997. |
| [12] | MIAO Xiao-hui, LIAN Zhiyun, LIU Ju, CHEN Hong-xi, SHI Zi-yan, ZHOU Hong-yu, YANG Rong. Investigation and analysis of health-related quality of life in myasthenia gravis patients with myasthenia gravis quality of life-15 Chinese version [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 514-520. |
| [13] | LEI Jie,LIU Mu-qing,FU Kai-yuan. Disturbedsleep, anxiety and stress are possible risk indicators for temporomandibular disorders with myofascialpain [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 692-696. |
| [14] | YU Jie, WAN Feng, XIE Ji-yan, WU Song, CUI Zhong-qi, XU Min, ZHANG Zhe, GAO Wei. Role of EuroSCORE and SinoSCORE in prediction of early postoperative quality of life in patients after coronary artery bypass surgery [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 769-773. |
| [15] | LIU Yi-Xuan, ZHANG Yong-Shen, DUAN Li-Ping, ZHANG Lu, YANG Chang-Qing. Effect of inherent depression on chronic visceral hypersensitivity induced by colon acetate stimulation in neonatal rats [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 289-294. |
|
||