Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (6): 1055-1060. doi: 10.19723/j.issn.1671-167X.2021.06.008
Previous Articles Next Articles
Value of serum YKL-40 in the diagnosis of anti-MDA5-positive patients with dermatomyositis complicated with severe pulmonary injury
ZHANG Pu-li1,2,YANG Hong-xia1,2,ZHANG Li-ning1,2,GE Yong-peng1,PENG Qing-lin1,WANG Guo-chun1,LU Xin1,△( )
)
- 1. Department of Rheumatology, China-Japan Friendship Hospital, Beijing 100029, China
2. Peking University China-Japan Friendship School of Clinical Medicine, Beijing 100029, China
CLC Number:
- R593.26
| [1] |
Gupta R, Kumar S, Gow P, et al. Anti-MDA5-associated dermatomyositis[J]. Intern Med J, 2020, 50(4):484-487.
doi: 10.1111/imj.v50.4 |
| [2] |
Lian X, Zou J, Guo Q, et al. Mortality risk prediction in amyopathic dermatomysitis associated with interstitial lung disease: The FLAIR model[J]. Chest, 2020, 158(4):1535-1545.
doi: 10.1016/j.chest.2020.04.057 |
| [3] | Ge YP, Shu XM, He LR, et al. Infection is not rare in patients with idiopathic inflammatory myopathies[J/OL]. Clin Exp Rheumatol, 2021(2021-07-21)[2021-08-01]. https://pubmed.ncbi.nlm.nih.gov/34369354/. |
| [4] |
Wu C, Wang Q, He L, et al. Hospitalization mortality and associated risk factors in patients with polymyositis and dermatomyositis: A retrospective case-control study[J]. PLoS One, 2018, 13(2):e0192491.
doi: 10.1371/journal.pone.0192491 |
| [5] | Yeo IJ, Lee CK, Han SB, et al. Roles of chitinase 3-like 1 in the development of cancer, neurodegenerative diseases, and inflammatory diseases[J/OL]. Pharmacol Ther, 2019, 203(2019-07-26)[2021-08-01]. https://doi.org/10.1016/j.pharmthera.2019.107394. |
| [6] |
Furuhashi K, Suda T, Nakamura Y, et al. Increased expression of YKL-40, a chitinase-like protein, in serum and lung of patients with idiopathic pulmonary fibrosis[J]. Respir Med, 2010, 104(8):1204-1210.
doi: 10.1016/j.rmed.2010.02.026 pmid: 20347285 |
| [7] |
Kornblit B, Hellemann D, Munthe-Fog L, et al. Plasma YKL-40 and CHI3L1 in systemic inflammation and sepsis-experience from two prospective cohorts[J]. Immunobiology, 2013, 218(10):1227-1234.
doi: 10.1016/j.imbio.2013.04.010 pmid: 23706599 |
| [8] |
Spoorenberg SM, Vestjens SM, Rijkers GT, et al. YKL-40, CCL18 and SP-D predict mortality in patients hospitalized with community-acquired pneumonia[J]. Respirology, 2017, 22(3):542-550.
doi: 10.1111/resp.12924 pmid: 27782361 |
| [9] | Hozumi H, Fujisawa T, Enomoto N, et al. Clinical utility of YKL-40 in polymyositis/dermatomyositis-associated interstitial lung disease[J]. J Rheumatol, 2017, 44(9):1394-1401. |
| [10] |
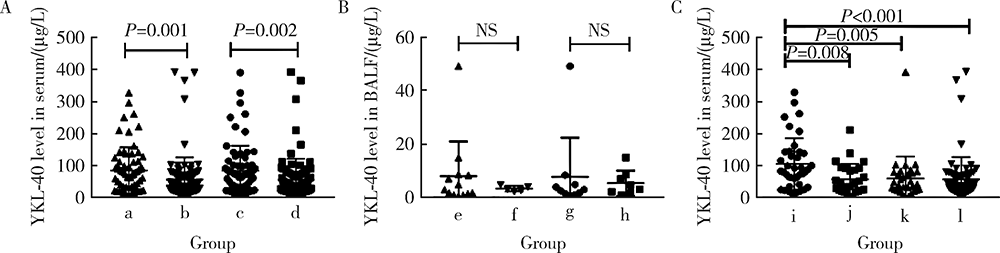
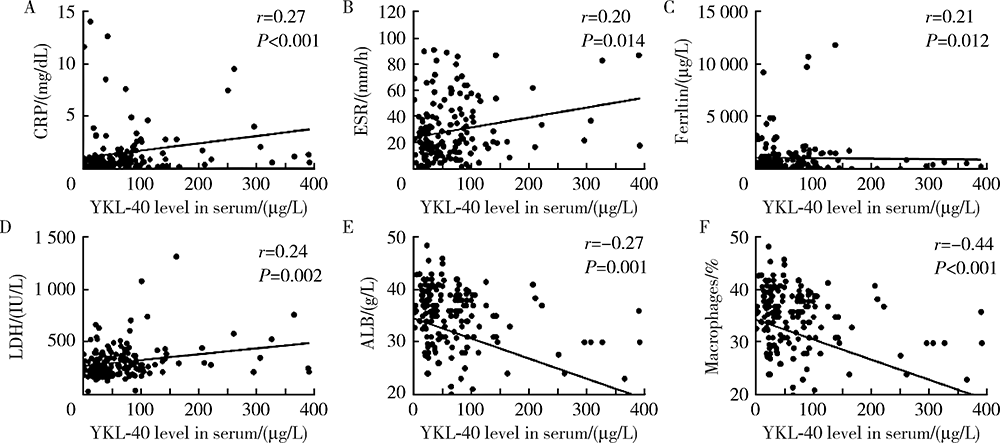
Jiang L, Wang Y, Peng Q, et al. Serum YKL-40 level is associated with severity of interstitial lung disease and poor prognosis in dermatomyositis with anti-MDA5 antibody[J]. Clin Rheumatol, 2019, 38(6):1655-1663.
doi: 10.1007/s10067-019-04457-w pmid: 30739212 |
| [11] |
Lundberg IE, Tjärnlund A, Bottai M, et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups[J]. Ann Rheum Dis, 2017, 76(12):1955-1964.
doi: 10.1136/annrheumdis-2017-211468 pmid: 29079590 |
| [12] |
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias[J]. Am J Respir Crit Care Med, 2013, 188(6):733-748.
doi: 10.1164/rccm.201308-1483ST |
| [13] |
Moghadam-Kia S, Oddis CV, Aggarwal R. Anti-MDA5 antibody spectrum in western world[J]. Curr Rheumatol Rep, 2018, 20(12):78.
doi: 10.1007/s11926-018-0798-1 pmid: 30382445 |
| [14] |
Sugiyama Y, Yoshimi R, Tamura M, et al. The predictive prognostic factors for polymyositis/dermatomyositis-associated interstitial lung disease[J]. Arthritis Res Ther, 2018, 20(1):7.
doi: 10.1186/s13075-017-1506-7 pmid: 29325580 |
| [15] |
James AJ, Reinius LE, Verhoek M, et al. Increased YKL-40 and chitotriosidase in asthma and chronic obstructive pulmonary disease[J]. Am J Respir Crit Care Med, 2016, 193(2):131-142.
doi: 10.1164/rccm.201504-0760OC |
| [16] |
Korthagen NM, van Moorsel CH, Barlo NP, et al. Serum and BALF YKL-40 levels are predictors of survival in idiopathic pulmonary fibrosis[J]. Respir Med, 2011, 105(1):106-113.
doi: 10.1016/j.rmed.2010.09.012 pmid: 20888745 |
| [17] | Fantino E, Gangell CL, Hartl D, et al. Airway, but not serum or urinary, levels of YKL-40 reflect inflammation in early cystic fibrosis lung disease[J/OL]. BMC Pulm Med, 2014, 14: 28[2021-08-01]. https://doi.org/10.1186/1471-2466-14-28. |
| [18] |
Wang HL, Hsiao PC, Tsai HT, et al. Usefulness of plasma YKL-40 in management of community-acquired pneumonia severity in patients[J]. Int J Mol Sci, 2013, 14(11):22817-22825.
doi: 10.3390/ijms141122817 |
| [19] |
Yang X, Sheng G. YKL-40 levels are associated with disease severity and prognosis of viral pneumonia, but not available in bacterial pneumonia in children[J]. BMC Pediatr, 2018, 18(1):381.
doi: 10.1186/s12887-018-1345-y |
| [20] | Long X, Xuan H, Ohshimo S, et al. Serum YKL-40 as predictor of outcome in hypersensitivity pneumonitis[J/OL]. Eur Respir J, 2016, 49(2): 1501924 [2021-08-01]. https://doi.org/10.1183/13993003.01924-2015. |
| [21] |
Shirakashi M, Nakashima R, Tsuji H, et al. Efficacy of plasma exchange in anti-MDA5-positive dermatomyositis with interstitial lung disease under combined immunosuppressive treatment[J]. Rheumatology (Oxford), 2020, 59(11):3284-3292.
doi: 10.1093/rheumatology/keaa123 |
| [1] | Xiao-yan XING,Jun-xiao ZHANG,Feng-yun-zhi ZHU,Yi-fan WANG,Xin-yao ZHOU,Yu-hui LI. Clinical analysis of 5 cases of dermatomyositis complicated with macrophage activation syndrome [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1214-1218. |
| [2] | Yu-zhou GAN,Yu-hui LI,Li-hua ZHANG,Lin MA,Wen-wen HE,Yue-bo JIN,Yuan AN,Zhan-guo LI,Hua YE. Comparison of clinical and immunological features between clinically amyopathic dermatomyositis and typical dermatomyositis [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1001-1008. |
| [3] | Jing XU,Jing XU,He LI,Jie TANG,Jian-long SHU,Jing ZHANG,Lian-jie SHI,Sheng-guang LI. Dermatomyositis combined with IgA vasculitis: A case report [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1173-1177. |
| [4] | Yi-ying YANG,Xiao-xia ZUO,Hong-lin ZHU,Si-jia LIU. Advances in epigenetic markers of dermatomyositis/polymyositis [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 374-377. |
| [5] | YU Jian-feng, JIN Yue-bo, HE Jing, AN Yuan, LI Zhan-guo. Changes of serum Krebs von den Lungen-6 levels in interstitial lung disease associated with dermatomyositis and secondary Sjögren’s syndrome: a case report [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 910-914. |
| [6] | LIU Shuang, AN Yuan, JIA Yuan, LI Zhan-Guo. A case of clinical overlap syndrome of rheumatoid arthritis and amyopathic dermatomyositis with multiple pulmonary injuries [J]. Journal of Peking University(Health Sciences), 2014, 46(5): 805-808. |
|
||