Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (6): 1049-1054. doi: 10.19723/j.issn.1671-167X.2021.06.007
Previous Articles Next Articles
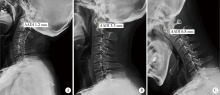
Analysis of cervical instability and clinical characteristics in treatment-naive rheumatoid arthritis patients
ZHANG Lu1,HU Xiao-hong2,CHEN Cheng1,CAI Yue-ming1,WANG Qing-wen1,ZHAO Jin-xia3,△( )
)
- 1. Department of Rheumatology & Immunology, Shenzhen 518036, Guangdong, China
2. Department of medical imaging, Peking University Shenzhen Hospital, Shenzhen 518036, Guangdong, China
3. Department of Rheumatology & Immunology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R593.22
| [1] | Yang SY, Boniello AJ, Poorman CE, et al. A review of the diagnosis and treatment of atlantoaxial dislocations[J]. Global Spine, 2014, 4(3):197-210. |
| [2] |
Olinger CR, Bransford R. Upper cervical trauma[J]. Orthop Clin North Am, 2021, 52(4):451-479.
doi: 10.1016/j.ocl.2021.05.013 |
| [3] |
Hedequist D, Bekelis K, Emans J, et al. Single stage reduction and stabilization of basilar invagination after failed prior fusion surgery in children with Down’s syndrome[J]. Spine (Phila Pa 1976), 2010, 35(4):E128-133.
doi: 10.1097/BRS.0b013e3181bad0c2 |
| [4] | 张璐, 刘湘源. 不可忽视类风湿关节炎的颈椎受累[J]. 中华风湿病学杂志, 2015, 19(4):217-218. |
| [5] | 张璐, 胡小红, 王庆文, 等. 类风湿关节炎合并颈椎失稳的人群分布及临床特征[J]. 北京大学学报(医学版), 2020, 52(6):50-55. |
| [6] |
Bodakçi E, Üsküdar CD, Ertürk A, et al. Can neck pain be an initial symptom of rheumatoid arthritis? A case report and literature review[J]. Rheumatol Int, 2018, 38(5):925-931.
doi: 10.1007/s00296-018-4019-z pmid: 29589114 |
| [7] |
Baek IW, Joo YB, Park KS, et al. Risk factors for cervical spine instability in patients with rheumatoid arthritis[J]. Clin Rheumatol, 2021, 40(2):547-555.
doi: 10.1007/s10067-020-05243-9 |
| [8] |
Mori Y, Izumiyama T, Baba K, et al. Evaluation of risk factors of vertebral fracture in Japanese female patients with glucocorticoid-induced osteoporosis[J]. J Orthop Surg Res, 2020, 15(1):290.
doi: 10.1186/s13018-020-01813-4 pmid: 32727595 |
| [9] |
Sandström T, Rantalaiho V, Yli-Kerttula T, et al. Cervical spine involvement among patients with rheumatoid arthritis treated actively with treat-to-target strategy: 10-year results of the NEO-RACo study[J]. J Rheumatol, 2020. 47(8):1160-1164.
doi: 10.3899/jrheum.190139 pmid: 31732558 |
| [10] |
Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative[J]. Ann Rheum Dis, 2010, 69(9):1580-1588.
doi: 10.1136/ard.2010.138461 pmid: 20699241 |
| [11] | Joaquim AF, Ghizoni E, Tedeschi H, et al. Radiological evaluation of cervical spine involvement in rheumatoid arthritis[J]. Neurosurg Focus, 2015, 38(4):E4. |
| [12] |
Shlobin NA, Dahdaleh NS. Cervical spine manifestations of rheumatoid arthritis: A review[J]. Neurosurg Rev, 2021, 44(4):1957-1965.
doi: 10.1007/s10143-020-01412-1 |
| [13] |
Drosos AA, Pelechas E, Voulgari PV. Radiological findings of the cervical spine in rheumatoid arthritis: What a rheumatologist should know[J]. Curr Rheumatol Rep, 2020, 22(6):19.
doi: 10.1007/s11926-020-00894-8 |
| [14] |
Zhang T, Pope J. Cervical spine involvement in rheumatoid arthritis over time: Results from a meta-analysis[J]. Arthritis Res Ther, 2015, 17(1):148.
doi: 10.1186/s13075-015-0643-0 |
| [15] | Mańczak M, Gasik R. Cervical spine instability in the course of rheumatoid arthritis-imaging methods[J]. Reumatologia, 2017, 55(4):201-207. |
| [16] |
Zhu S, Xu W, Luo Y, et al. Cervical spine involvement risk factors in rheumatoid arthritis: A meta-analysis[J]. Int J Rheum Dis, 2017, 20(5):541-549.
doi: 10.1111/apl.2017.20.issue-5 |
| [17] |
Na MK, Chun HJ, Bak KH, et al. Risk factors for the development and progression of atlantoaxial subluxation in surgically treated rheumatoid arthritis patients, considering the time interval between rheumatoid arthritis diagnosis and surgery[J]. J Korean Neurosurg Soc, 2016, 59(6):590-596.
doi: 10.3340/jkns.2016.59.6.590 |
| [18] |
Möller B, Everts-graber J, Florentinus S, et al. Low hemoglobin and radiographic damage progression in early rheumatoid arthritis: secondary analysis from a phase Ⅲ trial[J]. Arthritis Care Res (Hoboken), 2018, 70(6):861-868.
doi: 10.1002/acr.v70.6 |
| [1] | Dongwu LIU, Jie CHEN, Mingli GAO, Jing YU. Rheumatoid arthritis with Castleman-like histopathology in lymph nodes: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 928-931. |
| [2] | Huina HUANG,Jing ZHAO,Xiangge ZHAO,Ziran BAI,Xia LI,Guan WANG. Regulatory effect of lactate on peripheral blood CD4+ T cell subsets in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 519-525. |
| [3] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [4] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [5] | Qi WU,Yue-ming CAI,Juan HE,Wen-di HUANG,Qing-wen WANG. Correlation between dyslipidemia and rheumatoid arthritis associated interstitial lung disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 982-992. |
| [6] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Correlation analysis between body mass index and clinical characteristics of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 993-999. |
| [7] | Yin-ji JIN,Lin SUN,Jin-xia ZHAO,Xiang-yuan LIU. Significance of IgA isotype of anti-v-raf murine sarcoma viral oncogene homologue B1 antibody in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 631-635. |
| [8] | Wen-xin CAI,Shi-cheng LI,Yi-ming LIU,Ru-yu LIANG,Jing LI,Jian-ping GUO,Fan-lei HU,Xiao-lin SUN,Chun LI,Xu LIU,Hua YE,Li-zong DENG,Ru LI,Zhan-guo LI. A cross-sectional study on the clinical phenotypes of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1068-1073. |
| [9] | Fang CHENG,Shao-ying YANG,Xing-xing FANG,Xuan WANG,Fu-tao ZHAO. Role of the CCL28-CCR10 pathway in monocyte migration in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1074-1078. |
| [10] | Rui LIU,Jin-xia ZHAO,Liang YAN. Clinical characteristics of patients with rheumatoid arthritis complicated with venous thrombosis of lower extremities [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1079-1085. |
| [11] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1086-1093. |
| [12] | GAO Chao,CHEN Li-hong,WANG Li,YAO Hong,HUANG Xiao-wei,JIA Yu-bo,LIU Tian. Validation of the Pollard’s classification criteria (2010) for rheumatoid arthritis patients with fibromyalgia [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 278-282. |
| [13] | ZHONG Hua,XU Li-ling,BAI Ming-xin,SU Yin. Effect of chemokines CXCL9 and CXCL10 on bone erosion in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1026-1031. |
| [14] | LOU Xue,LIAO Li,LI Xing-jun,WANG Nan,LIU Shuang,CUI Ruo-mei,XU Jian. Methylation status and expression of TWEAK gene promoter region in peripheral blood of patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1020-1025. |
| [15] | LUO Liang,HUO Wen-gang,ZHANG Qin,LI Chun. Clinical characteristics and risk factors of rheumatoid arthritis with ulcerative keratitis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1032-1036. |
|
||