Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (1): 126-133. doi: 10.19723/j.issn.1671-167X.2022.01.020
Previous Articles Next Articles
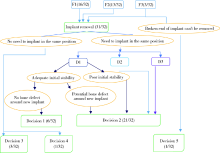
Clinical classification and treatment decision of implant fracture
- Fourth Clinical Division, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100025, China
CLC Number:
- R783
| [1] | Albrektsson T, Zarb GA, Worthington P, et al. The long-term efficacy of currently used dental implants: A review and proposed criteria of success[J]. Int J Oral Maxillofac Implants, 1986, 1(1):11-25. |
| [2] | 林野, 李健慧, 邱立新. 口腔种植修复临床效果十年回顾研究[J]. 中华口腔医学杂志, 2006, 41(3):131-135. |
| [3] |
Berglundh T, Persson L, Bjorn K. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years[J]. J Clin Periodontol, 2002, 29(Suppl 3):197-212
doi: 10.1034/j.1600-051X.29.s3.12.x |
| [4] |
Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw[J]. Int J Oral Surg, 1981, 10(6):387-416.
pmid: 6809663 |
| [5] | Rangert B. Force and moments on branemark implants[J]. Int J Oral Maxillofac Implants, 1989, 4(3):241-247. |
| [6] |
Takeuchi K, Ohara T, Furuta M, et al. Tooth loss and risk of dementia in the community: The hisayama study[J]. J Am Geriatr Soc, 2017, 65(5):95-100.
doi: 10.1111/jgs.14791 pmid: 28272750 |
| [7] | Lee JH, Kin YT, Jeong SN, et al. Incidence and pattern of implant fractures: A long-term follow-up multicenter study[J]. Clin Oral Implants Res, 2018, 20(4):463-469. |
| [8] | Misch CE, Strong JT, Bidez MW. Dental implant prosthetics[M]. St. Louis Missouri: Mosby, 2015: 293-314. |
| [9] |
Chrcanovic BR, Kisch J, Albrektsson T, et al. Factors influencing the fracture of dental implants[J]. Clin Implant Dent Relat Res, 2017, 20(1):58-67.
doi: 10.1111/cid.2018.20.issue-1 |
| [10] | Eckert SE, Salinas TJ, Aka K. Dental implant complications: Etiology, prevention, and treatment, 2[M]. Hoboken New Jersey: John Wiley & Sons, Ltd, 2015: 132-144. |
| [11] |
Alkharrat AR, Schmitter M, Rues S, et al. Fracture behavior of all-ceramic, implant-supported, and tooth-implant-supported fixed dental prostheses[J]. Clin Oral Investig, 2018, 22(4):1663-1673.
doi: 10.1007/s00784-017-2233-9 |
| [12] |
Gealh WC, Valéria M, Barbi F, et al. Osseointegrated implant fracture: Causes and Treatment[J]. J Oral Implantol, 2011, 37(4):499-503.
doi: 10.1563/AAID-JOI-D-09-00135.1 |
| [13] | 张磊, 冯海兰. 种植固定修复后机械并发症的预防和处理[J]. 中华口腔医学杂志, 2016, 51(1):10-14. |
| [14] |
Schwarz MS. Mechanical complications of dental implants[J]. Clin Oral Implants Res, 2000, 11(Suppl 1):156-158.
doi: 10.1034/j.1600-0501.2000.011S1156.x |
| [15] | 尉华杰, 朱一博, 王兴. 19枚种植体负重不同时间后折裂折断的临床分析[J]. 中华口腔医学杂志, 2018, 53(12):815-820. |
| [16] | Quek HC, Tan KB, Nicholls JI. Load fatigue performance of four implant-abutment interface designs: Effect of torque level and implant system[J]. Int J Oral Maxillofac Implants, 2008, 23(2):253-262. |
| [17] | Wiskott HWA, Jaquet R, Scherrer SS, et al. Resistance of internal-connection implant connectors under rotational fatigue loading[J]. Int J Oral Maxillofac Implants, 2007, 22(2):249-257. |
| [18] |
Shemtov-Yona K, Rittel D, Machtei EE, et al. Effect of dental implant diameter on fatigue performance. Part Ⅱ: Failure analysis[J]. Clin Implant Dent Relat Res, 2014, 16(2):178-184.
doi: 10.1111/cid.2014.16.issue-2 |
| [19] |
Gratton DG, Aquilino SA, Stanford CM. Micromotion and dynamic fatigue properties of the dental implant-abutment interface[J]. J Prosthet Dent, 2001, 85(1):47-52.
pmid: 11174678 |
| [20] |
Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Branemark system[J]. Clin Oral Implants Res, 2010, 3(3):104-111.
doi: 10.1034/j.1600-0501.1992.030302.x |
| [21] | Morgan MJ, James DF, Pilliar RM. Fractures of the fixture component of an osseointegrated implant[J]. Int J Oral Maxillofac Implants, 1993, 8(4):409-414. |
| [22] |
Silva NR, Nourian P, Coelho PG, et al. Impact fracture resistance of two titanium-abutment systems versus a single-piece ceramic implant[J]. Clin Implant Dent Relat Res, 2011, 13(2):168-173.
doi: 10.1111/cid.2011.13.issue-2 |
| [23] |
Steinebrunner L, Wolfart S, Ludwig K, et al. Implant-abutment interface design affects fatigue and fracture strength of implants[J]. Clin Oral Implants Res, 2009, 19(12):1276-1284.
doi: 10.1111/clr.2008.19.issue-12 |
| [24] | Rangert B. Bending overload and implant fracture: a retrospective clinical analysis[J]. Int J Oral Maxillofac Implants, 1995, 10(3):326-334. |
| [25] |
Muroff F, Fredrick I. Removal and replacement of a fractured dental implant: case report[J]. Implant Dent, 2003, 12(3):206-210.
pmid: 14560479 |
| [26] | Balshi TJ, Hernandez FE, Pryszlak DC, et al. An analysis and management of fractured implants: A clinical report[J]. Int J Oral Maxillofac Implants, 1996, 11(5):660-666. |
| [1] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [2] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [3] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [4] | LI Peng,PIAO Mu-zi,HU Hong-cheng,WANG Yong,ZHAO Yi-jiao,SHEN Xiao-jing. Radiography study on osteotome sinus floor elevation with placed implant simultaneously with no graft augmentation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 95-101. |
| [5] | Zhong ZHANG,Huan-xin MENG,Jie HAN,Li ZHANG,Dong SHI. Effect of vertical soft tissue thickness on clinical manifestation of peri-implant tissue in patients with periodontitis [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 332-338. |
| [6] | Chun-ping LIN,Song-he LU,Jun-xin ZHU,Hong-cheng HU,Zhao-guo YUE,Zhi-hui TANG. Influence of thread shapes of custom-made root-analogue implants on stress distribution of peri-implant bone: A three-dimensional finite element analysis [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1130-1137. |
| [7] | Qian WANG,Dan LI,Zhi-hui TANG. Sinus floor elevation and simultaneous dental implantation: A long term retrospective study of sinus bone gain [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 925-930. |
| [8] | Xiao-qian LIU,Qiu-wen CHEN,Hai-lan FENG,Bing WANG,Jian QU,Zhen SUN,Mo-di HENG,Shao-xia PAN. Oral hygiene maintenance of locator attachments implant overdentures in edentulous population: A longitudinal study [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 136-144. |
| [9] | Zhi-yong△ ZHANG,Tian MENG,Quan CHEN,Wen-shu LIU,Yu-huan CHEN. Retrospective analysis of early dental implant failure [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1088-1091. |
| [10] | LIU Jing-yin, CHEN Fei, GE Yan-jun, WEI Ling, PAN Shao-xia, FENG Hai-lan. Influence of implants prepared by selective laser melting on early bone healing [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 117-122. |
| [11] | LIANG Nai-wen, SHI Lei,HUANG Ying,DENG Xu-liang. Role of different scale structures of titanium implant in the biological behaviors of human umbilical vein endothelial cells [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 43-048. |
| [12] | LI Bei-bei, LIN Ye, CUI Hong-yan, HAO Qiang, XU Jia-bin, DI Ping. Clinical evaluation of “All-on-Four” provisional prostheses reinforced with carbon fibers [J]. Journal of Peking University(Health Sciences), 2016, 48(1): 133-137. |
| [13] | CUI Hong-Yan, DI Ping, LI Jian-Hui, LIN Ye, LIU Rong-Rong. Application of spark erosion technology in manufacture of implant prosthesis [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 336-339. |
| [14] | HAN Jie, CHEN Zhi-Bin, LI Wei, MENG Huan-Xin. Determination of bone metabolic marker levels in perio-implant crevicular fluid and analysis of dental implants stability by resonance frequency in the early stage of healing [J]. Journal of Peking University(Health Sciences), 2015, 47(1): 37-41. |
| [15] | WU Min-Jie, ZHANG Xiang-Hao, ZOU Li-Dong, LIANG Feng. Clinical observation of the reliability of gingival contour by using temporary crown after loading 1 year [J]. Journal of Peking University(Health Sciences), 2014, 46(6): 954-957. |
|
||