Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (3): 434-442. doi: 10.19723/j.issn.1671-167X.2022.03.007
Previous Articles Next Articles
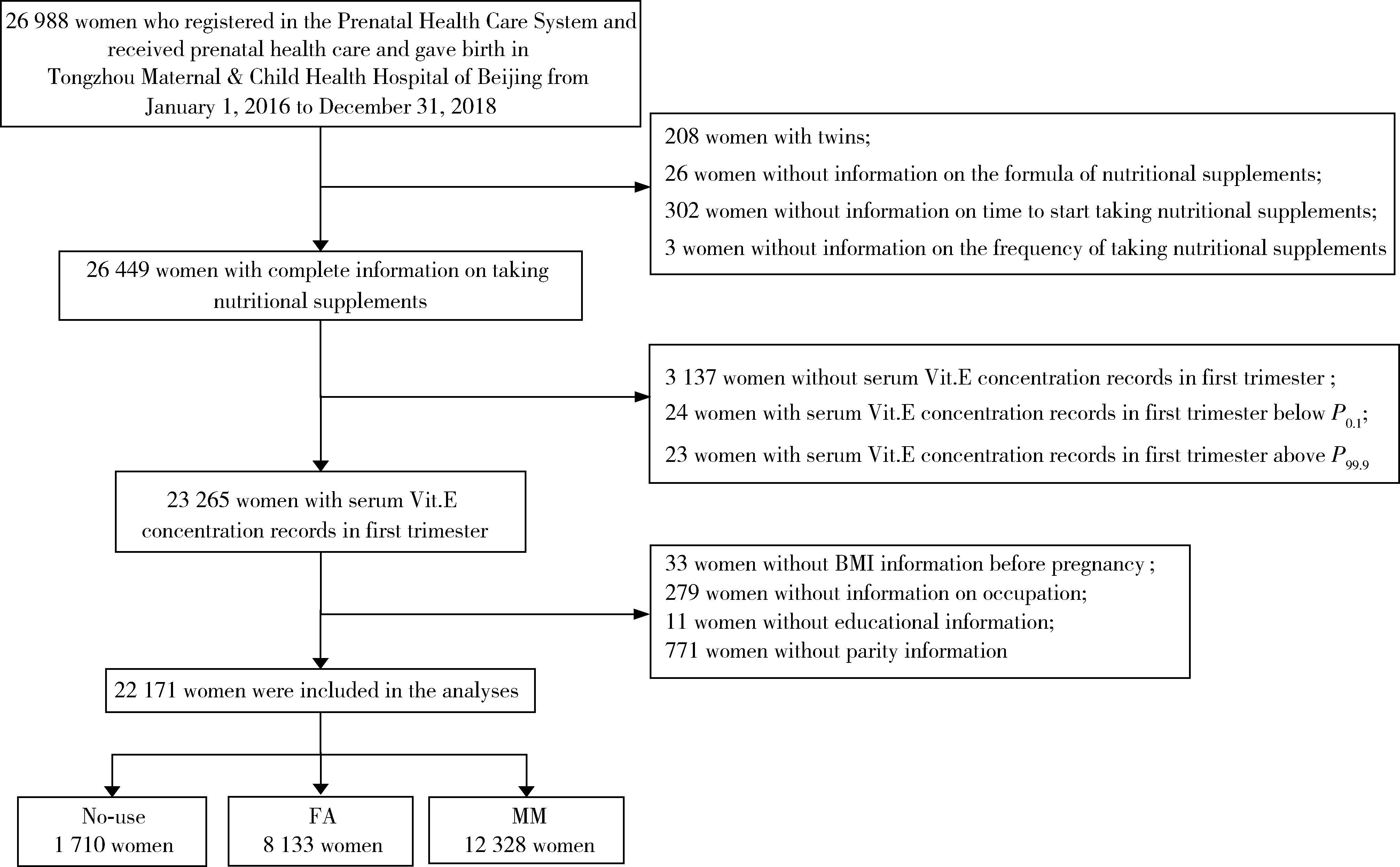
Relationship between micronutrients supplementation during periconceptional period and serum concentration of vitamin E in the 1st trimester of gestational period
Yun-fei XING1,Chun-yi LIU1,Wen-ying MENG2,Jie ZHANG1,Ming-yuan JIAO3,Lei JIN4,Lei JIN1,*( )
)
- 1. Institute of Reproductive and Child Health, Peking University; National Health Commission Key Laboratory of Reproductive Health, Beijing 100191, China
2. Department of Obstetrics, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
3. Department of Clinical Laboratory, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
4. Department of Maternal Health Care, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
CLC Number:
- R169
| 1 |
Steegers-Theunissen RP , Twigt J , Pestinger V , et al. The periconceptional period, reproduction and long-term health of offspring: The importance of one-carbon metabolism[J]. Hum Reprod Update, 2013, 19 (6): 640- 655.
doi: 10.1093/humupd/dmt041 |
| 2 | Chen H , Qian N , Yan L , et al. Role of serum vitamin A and E in pregnancy[J]. Exp Ther Med, 2018, 16 (6): 5185- 5189. |
| 3 | 李俊, 郑春梅, 倪君君, 等. 2013-2016年北京地区孕妇维生素A、维生素E营养水平[J]. 卫生研究, 2019, 48 (1): 56- 60. |
| 4 | 李浩, 倪君君, 郑春梅. 2016年我国北方地区孕妇维生素A、E营养状况调查[J]. 中国医药导报, 2019, 16 (9): 64- 67. |
| 5 | 申南, 陆娣, 郑春梅, 等. 常规保健下不同年龄段孕妇妊娠早期血清维生素A、E水平分析[J]. 中国妇产科临床杂志, 2018, 19 (4): 356- 358. |
| 6 | 贾军恒, 田文琴, 强莉. 不同孕期妇女血清维生素A、维生素E水平的临床观察[J]. 中国妇幼保健, 2019, 34 (3): 509- 511. |
| 7 | 钮慧远, 薛秀平, 仲晓慧. 2017-2018年淮安地区孕妇维生素A、维生素E水平及其影响因素[J]. 卫生研究, 2020, 49 (1): 41- 43. |
| 8 | 孟文颖, 黄琬桐, 张杰, 等. 孕早期血清维生素E水平与妊娠期高血压疾病发病风险的关系[J]. 北京大学学报(医学版), 2020, 52 (3): 470- 478. |
| 9 |
Sharifipour F , Abedi P , Ciahkal SF , et al. Serum vitamin E level and gestational diabetes mellitus: A systematic review and meta-analysis[J]. J Diabetes Metab Disord, 2020, 19 (2): 1787- 1795.
doi: 10.1007/s40200-020-00582-5 |
| 10 | 施文瑶, 施晓华, 朱晓燕, 等. 孕期血清维生素A、D、E水平与妊娠期糖尿病的相关性研究[J]. 中国卫生检验杂志, 2021, 31 (4): 473- 475. |
| 11 |
Pazdro R , Burgess JR . The role of vitamin E and oxidative stress in diabetes complications[J]. Mech Ageing Dev, 2010, 131 (4): 276- 286.
doi: 10.1016/j.mad.2010.03.005 |
| 12 |
Nourooz-Zadeh J , Rahimi A , Tajaddini-Sarmadi J , et al. Relationships between plasma measures of oxidative stress and metabo-lic control in NIDDM[J]. Diabetologia, 1997, 40 (6): 647- 653.
doi: 10.1007/s001250050729 |
| 13 | Kutbi HA , Hammouda SA . Plasma concentrations of vitamin A and E and risk of dysglycemia in first-trimester pregnant Saudi women[J]. Diabetol Metab Syndr, 2020, (12): 17. |
| 14 | 吕祺, 阴春霞, 周硕, 等. 孕妇血清维生素D和维生素E水平与妊娠期高血压疾病发生的相关性[J]. 中国妇幼保健, 2021, 36 (16): 3662- 3665. |
| 15 |
Gilboa SM , Lee KA , Cogswell ME , et al. Maternal intake of vitamin E and birth defects, national birth defects prevention study, 1997 to 2005[J]. Birth Defects Res A Clin Mol Teratol, 2014, 100 (9): 647- 657.
doi: 10.1002/bdra.23247 |
| 16 | Rigotti A . Absorption, transport, and tissue delivery of vitamin E[J]. Molecular aspects of medicine, 2007, 28 (5): 423- 436. |
| 17 |
Traber MG , Rader D , Acuff RV , et al. Vitamin E dose-response studies in humans with use of deuterated RRR-alpha-tocopherol[J]. Am J Clin Nutr, 1998, 68 (4): 847- 853.
doi: 10.1093/ajcn/68.4.847 |
| 18 |
李军生. 维生素E吸收与代谢机制的研究进展[J]. 中国现代应用药学, 2005, 22 (6): 457- 461.
doi: 10.3969/j.issn.1007-7693.2005.06.008 |
| 19 | 陈曦, 宫照龙, 沈葹. 超高效液相色谱-三重四级杆串联质谱法测定血清中维生素A和维生素E[J]. 卫生研究, 2021, 50 (2): 301- 307. |
| 20 | 金蕾, 王程, 张杰, 等. 妇女围受孕期叶酸服用情况及其对胎儿神经管缺陷的预防效果[J]. 北京大学学报(医学版), 2020, 52 (4): 719- 725. |
| 21 |
Wang L , Leng J , Liu H , et al. Association between hypertensive disorders of pregnancy and the risk of postpartum hypertension: A cohort study in women with gestational diabetes[J]. J Hum Hypertens, 2017, 31 (11): 725- 730.
doi: 10.1038/jhh.2017.46 |
| 22 | 闫明, 张雯, 刘凯波, 等. 北京地区2010-2017年增补叶酸预防神经管缺陷工作效果分析[J]. 中国优生与遗传杂志, 2019, 27 (3): 339- 341. |
| 23 |
Bian H , Tang Y , Zhou Y , et al. Demographic variations and temporal trends in prenatal use of multiple micronutrient supplements in Beijing, 2013-2017[J]. Public Health Nutr, 2021, 24 (5): 826- 833.
doi: 10.1017/S1368980020004905 |
| 24 |
Schulze KJ , Mehra S , Shaikh S , et al. Antenatal multiple micronutrient supplementation compared to iron-folic acid affects micronutrient status but does not eliminate deficiencies in a randomized controlled trial among pregnant women of rural bangladesh[J]. J Nutr, 2019, 149 (7): 1260- 1270.
doi: 10.1093/jn/nxz046 |
| 25 | Colapinto CK , O'Connor DL , Dubois L , et al. Prevalence and correlates of folic acid supplement use in Canada[J]. Health Rep, 2012, 23 (2): 39- 44. |
| [1] | Yue WEI,Lan YAO,Xi LU,Jun WANG,Li LIN,Kun-peng LIU. Evaluation of gastric emptying after drinking carbohydrates before cesarean section by gastric ultrasonography [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1082-1087. |
| [2] | Yin-xiao BAI,Chun-yi LIU,Jie ZHANG,Wen-ying MENG,Lei JIN,Lei JIN. Association between periconceptional supplementation of folic acid or multiple-micronutrients containing folic acid and preterm delivery in women [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 495-501. |
| [3] | Lei JIN,Cheng WANG,Jie ZHANG,Wen-ying MENG,Jia-yu ZHANG,Jin-hui YU,Gui-yin LIN,Ming-kun TONG,Lei JIN. Maternal periconceptional folic acid supplementation and its effects on the prevalence of fetal neural tube defects [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 719-725. |
| [4] | Wen-ying MENG,Wan-tong HUANG,Jie ZHANG,Ming-yuan JIAO,Lei JIN,Lei JIN. Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 470-478. |
| [5] | Zhang-jian CHEN,Shuo HAN,Pai ZHENG,Shu-pei ZHOU,Guang JIA. Effect of subchronic combined oral exposure of titanium dioxide nanoparticles and glucose on levels of serum folate and vitamin B12 in young SD rats [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 451-456. |
| [6] | SUN Ying, JIN Lei. Blood manganese levels among pregnant women and the associated factors in three counties of northern China [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 463-468. |
| [7] | YUAN Meng-meng, WANG Meng, LIU Jun-yi, ZHANG Zhi-li. Optimization of alkaline hydrolysis based on the side chain of diethyl ester 4-amino-N5 -formyl-N8,N10 -dideazatetrahydrofolic acid [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 714-718. |
| [8] | LIU Xin, DU Yi-qing, LI Yuan-xin, WANG Meng, ZHANG Zhi-li, WANG Xiao-wei, LIU Jun-yi, TIAN Chao. Improved synthesis process of diethyl N-[4-[(2,4-diaminopyrido[3,2-d]pyrimidin-6-yl)methylamino]benzoyl]-L-glutamate [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 842-845. |
|
||