Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (5): 1006-1012. doi: 10.19723/j.issn.1671-167X.2022.05.030
Previous Articles Next Articles
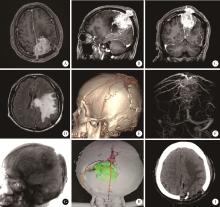
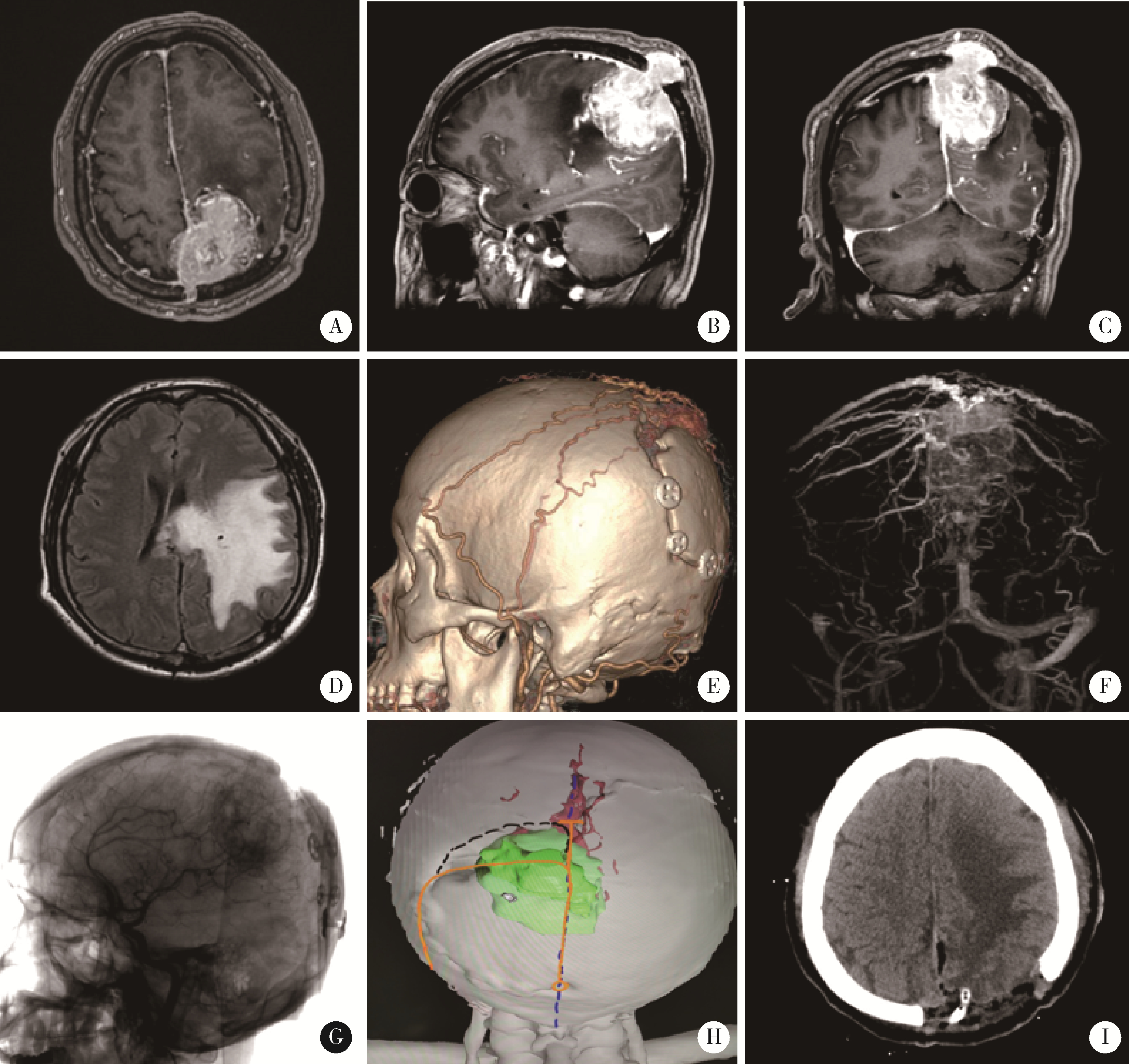
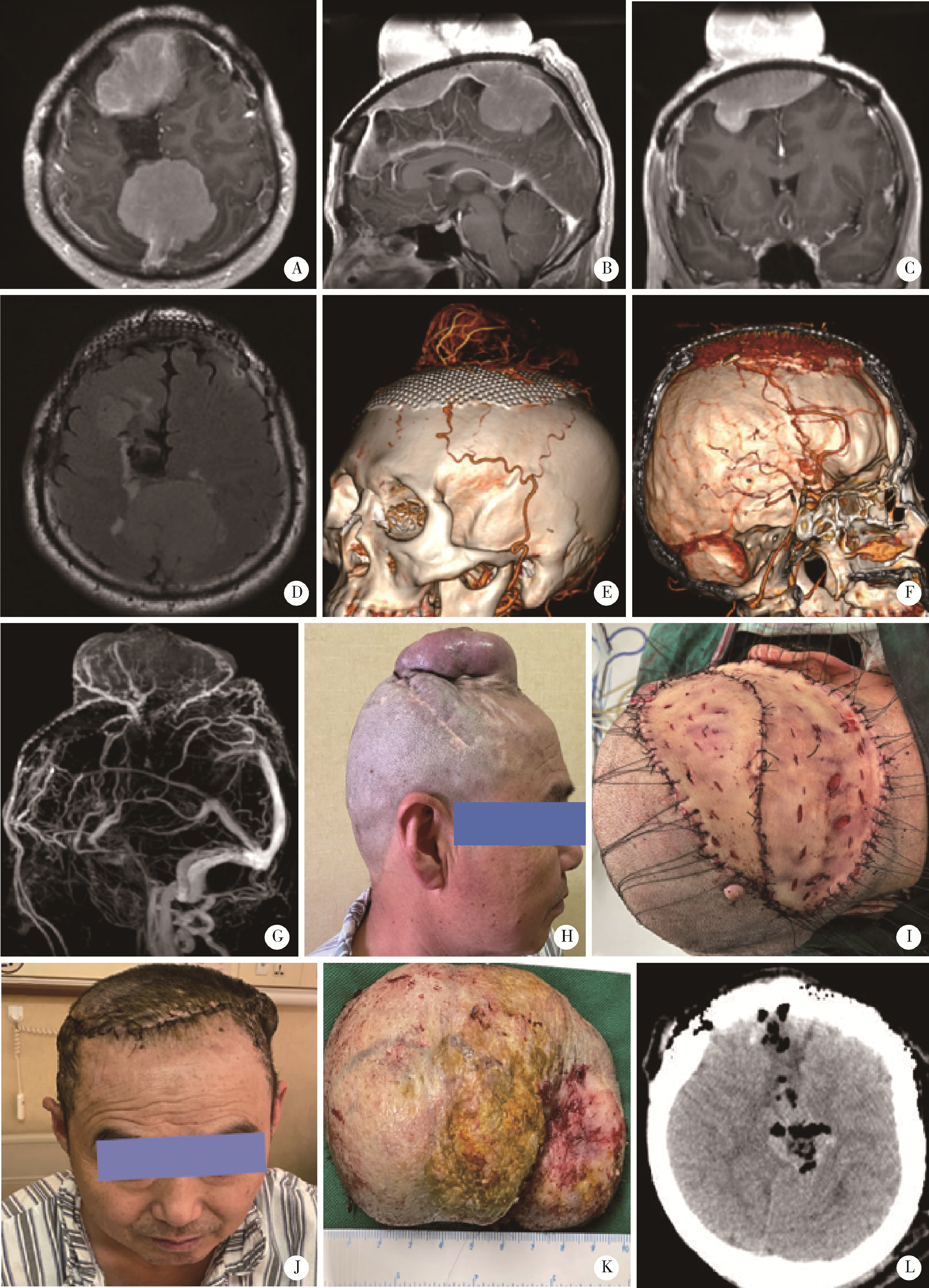
Surgical treatment of large and giant recurrent meningiomas near the middle and posterior third part of the superior sagittal sinus with extracranial invading
Su-hua CHEN1,2,Jun YANG1,2,*( ),Xin CHEN1,2,Chen-long YANG1,2,Jian-jun SUN1,2,Guo-zhong LIN1,2,Tao YU1,2,Xin YANG3,Yun-feng HAN1,2,Chao WU1,2,Yu SI1,2,Kai-ming MA1,2
),Xin CHEN1,2,Chen-long YANG1,2,Jian-jun SUN1,2,Guo-zhong LIN1,2,Tao YU1,2,Xin YANG3,Yun-feng HAN1,2,Chao WU1,2,Yu SI1,2,Kai-ming MA1,2
- 1. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
2. Center of Precision Neurosurgery and Oncology, Peking University Health Science Center, Beijing 100191, China
3. Department of Plastic Surgery, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R739.4
| 1 | 崔晟华, 陈坚, 梁日初. 22例复发脑膜瘤再手术疗效分析[J]. 临床神经外科杂志, 2011, 8 (2): 81- 83. |
| 2 |
Ehresman JS , Garzon-Muvdi T , Rogers D , et al. The relevance of Simpson grade resections in modern neurosurgical treatment of World Health Organization grade Ⅰ, Ⅱ, and Ⅲ meningiomas[J]. World Neurosurg, 2018, 109, e588- e593.
doi: 10.1016/j.wneu.2017.10.028 |
| 3 | 林国中, 孙建军, 陈素华, 等. 侵及上矢状窦大型和巨大型脑膜瘤的显微外科治疗[J]. 中华神经外科杂志, 2020, 36 (3): 243- 247. |
| 4 |
Sindou MP , Alvernia JE . Results of attempted radical tumor removal and venous repair in 100 consecutive meningiomas involving the major dural sinuses[J]. J Neurosurg, 2006, 105 (4): 514- 525.
doi: 10.3171/jns.2006.105.4.514 |
| 5 | 徐子明, 余新光, 朱儒远. 中央回区矢状窦旁脑膜瘤的显微手术治疗[J]. 中华显微外科杂志, 2003, 26 (1): 28- 30. |
| 6 | 刘厚杰, 李德志, 李学记, 等. 颅底内外沟通脑膜瘤的诊断和个体化治疗[J]. 中国微侵袭神经外科杂志, 2021, 26 (2): 53- 57. |
| 7 | 刘忆, 漆松涛. "脑膜尾征"与脑膜瘤部位及其病理类型的关系[J]. 中国临床神经外科杂志, 2010, 15 (6): 321- 323.321-323, 341 |
| 8 | Muto J , Mine Y , Nishiyama Y , et al. Intraoperative real-time near-infrared image-guided surgery to identify intracranial menin-giomas via microscope[J]. Front Neurosci, 2022, 5 (16): 837349. |
| 9 | 陈劲草, 雷霆, 陈坚, 等. 上矢状窦旁脑膜瘤致上矢状窦阻塞时侧支静脉通路的意义[J]. 中国临床神经外科杂志, 2004, 9 (1): 8- 10. |
| 10 | Raza SM , Gallia GL , Brem H , et al. Perioperative and long-term outcomes from the management of parasagittal meningiomas invading the superior sagittal sinus[J]. Neurosurgery, 2010, 67 (4): 885- 893. |
| 11 | Ohba S , Kobayashi M , Horiguchi T , et al. Long-term surgical outcome and biological prognostic factors in patients with skull base meningiomas[J]. J Neurosurg, 2011, 114 (5): 1278- 1287. |
| 12 | Williams EA , Santagata S , Wakimoto H , et al. Distinct genomic subclasses of high-grade/progressive meningiomas: NF2-associa-ted, NF2-exclusive, and NF2-agnostic[J]. Acta Neuropathol Commun, 2020, 8 (1): 171. |
| 13 | Goldbrunner R , Stavrinou P , Jenkinson MD , et al. EANO guideline on the diagnosis and management of meningiomas[J]. Neuro Oncol, 2021, 23 (11): 1821- 1834. |
| 14 | Louis DN , Perry A , Wesseling P , et al. The 2021 WHO classification of tumors of the central nervous system: a summary[J]. Neuro Oncol, 2021, 23 (8): 1231- 1251. |
| [1] | Yuqing LI,Biao WANG,Peng QIAO,Wei WANG,Xing GUAN. Medium to long-term efficacy of tension-free vaginal tape procedure in the treatment of female recurrent stress urinary incontinence [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 600-604. |
| [2] | Chieko MORIMOTO,Yi-qin WANG,Rong ZHOU,Jian-liu WANG. Clinical analysis of fertility-sparing therapy of patients with complex atypical hyperplasia and endometrial cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 936-942. |
| [3] | Yue WANG,Shuang ZHANG,Hong ZHANG,Li LIANG,Ling XU,Yuan-jia CHENG,Xue-ning DUAN,Yin-hua LIU,Ting LI. Clinicopathological features and prognosis of hormone receptor-positive/human epidermal growth factor receptor 2-negative breast cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 853-862. |
| [4] | LIU Lei,QIN Yan-chun,WANG Guo-liang,ZHANG Shu-dong,HOU Xiao-fei,MA Lu-lin. Strategy of reoperation for pheochromocytoma and paraganglioma [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 793-797. |
| [5] | Huan-bin YU,Wen-jie WU,Xiao-ming LV,Yan SHI,Lei ZHENG,Jian-guo ZHANG. 125I seed brachytherapy for recurrent salivary gland carcinoma after external radiotherapy [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 919-923. |
| [6] | Xu-chu ZHANG,Jian-hua ZHANG,Rong-fu WANG,Yan FAN,Zhan-li FU,Ping YAN,Guang-yu ZHAO,Yan-xia BAI. Diagnostic value of 18F-FDG PET/CT and tumor markers (CEA, CA19-9, CA24-2) in recurrence and metastasis of postoperative colorectal moderately differentiated adenocarcinoma [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1071-1077. |
| [7] | Shuai XU,Yang-shuo WANG,Shu LI,Hai-ying LIU. Guillain-Barre syndrome complicated on post-operation with renal carcinoma and meningioma: a case report [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 775-777. |
| [8] | Qi TANG,Rong-cheng LIN,Lin YAO,Zheng ZHANG,Han HAO,Cui-jian ZHANG,Lin CAI,Xue-song LI,Zhi-song HE,Li-qun ZHOU. Clinicopathologic features and prognostic analyses of locally recurrent renal cell carcinoma patients after initial surgery [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 628-631. |
| [9] | XING Yun-chao, XIONG Geng-yan, FANG Dong, ZHANG Zheng, CAI Lin, ZHANG Lei, HE Zhi-song, LI Xue-song, ZHOU Li-qun. Preoperative prognostic factors and preoperative risk stratification of upper tract urothelial carcinoma [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1032-1037. |
| [10] | CHEN Li-hua, YANG Yi, WEI Qun, LI Yun-jun, LI Wen-de, GAO Jin-bao,YU Bin, ZHAO Hao, XU Ru-xiang. Microsurgical management of petroclival meningiomas combined trans-subtemporal and suboccipital retrosigmoid keyhole approach [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 738-742. |
| [11] | LIU Yu-Qing, LU Jian, ZHAO Lei, HOU Xiao-Fei, MA Lu-Lin. Prognostic factors for intravesical recurrence after surgery for upper tract urothelial carcinoma in renal transplant recipients [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 605-610. |
| [12] | YANG Yang, XIAO Yun-Xiang, ZHOU Li-Qun, HE Zhi-Song, JIN Jie. Long-term outcome of isolated local recurrence following radical nephrectomy [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 528-531. |
|
||