Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (2): 299-307. doi: 10.19723/j.issn.1671-167X.2023.02.014
Previous Articles Next Articles
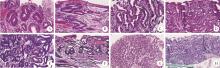
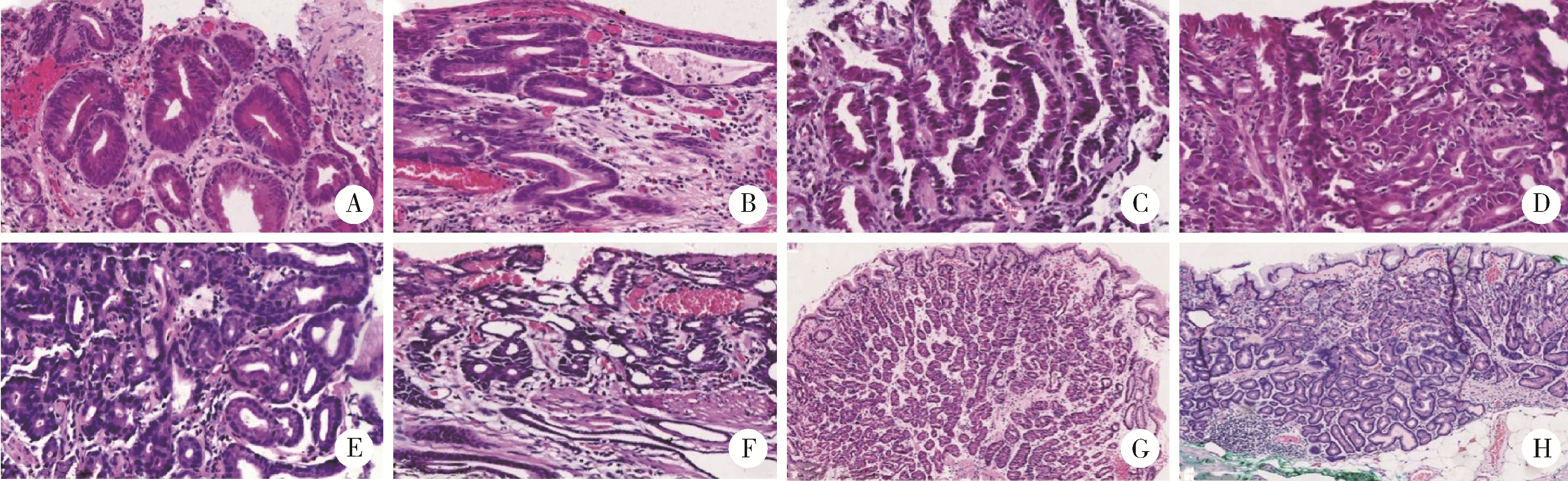
Pathological evaluation of endoscopic submucosal dissection for early gastric cancer and precancerous lesion in 411 cases
Ju-mei LIU1,Li LIANG1,Ji-xin ZHANG1,Long RONG2,Zi-yi ZHANG1,You WU1,Xu-dong ZHAO2,Ting LI1,*( )
)
- 1. Department of Pathology, Peking University First Hospital, Beijing 100034, China
2. Center of Endoscopy, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R735.2
| 1 |
Japanese Gastric Cancer Association . Japanese gastric cancer treatment guidelines 2018 (5th edition)[J]. Gastric Cancer, 2021, 24 (1): 1- 21.
doi: 10.1007/s10120-020-01042-y |
| 2 |
Banks M , Graham D , Jansen M , et al. British society of gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma[J]. Gut, 2019, 68 (9): 1545- 1575.
doi: 10.1136/gutjnl-2018-318126 |
| 3 |
北京市科委重大项目《早期胃癌治疗规范研究》专家组. 早期胃癌内镜下规范化切除的专家共识意见(2018, 北京)[J]. 中华消化内镜杂志, 2018, 36 (6): 381- 392.
doi: 10.3760/cma.j.issn.1007-5232.2018.06.001 |
| 4 |
赫捷, 陈万青, 李兆申, 等. 中国胃癌筛查与早诊早治指南制定专家组, 中国胃癌筛查与早诊早治指南制定工作组.中国胃癌筛查与早诊早治指南(2022, 北京)[J]. 中华消化外科杂志, 2022, 21 (7): 827- 851.
doi: 10.3760/cma.j.cn115610-20220624-00370 |
| 5 |
Lim H , Jung HY , Park YS , et al. Discrepancy between endos-copic forceps biopsy and endoscopic resection in gastric epithelial neoplasia[J]. Surg Endosc, 2014, 28 (4): 1256- 1262.
doi: 10.1007/s00464-013-3316-6 |
| 6 |
Lu C , Lv X , Lin Y , et al. Retrospective study: The diagnostic accuracy of conventional forceps biopsy of gastric epithelial compared to endoscopic submucosal dissection (STROBE compliant)[J]. Medicine, 2016, 95 (30): e4353.
doi: 10.1097/MD.0000000000004353 |
| 7 |
Wu S , Zhu X , Xiang L , et al. The Diagnostic accuracy of conventional forceps biopsy compared to ESD[J]. Open medicine (Warsaw, Poland), 2017, 12, 261- 265.
doi: 10.1515/med-2017-0039 |
| 8 |
Ono H , Yao K , Fujishiro M , et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition)[J]. Dig Endosc, 2021, 33 (1): 4- 20.
doi: 10.1111/den.13883 |
| 9 |
梁丽, 张继新, 戎龙, 等. 80例早期胃癌及癌前病变内镜黏膜下剥离术标本的处理及病理学评估[J]. 中华消化内镜杂志, 2016, 33 (9): 589- 597.
doi: 10.3760/cma.j.issn.1007-5232.2016.09.004 |
| 10 |
梁丽, 于妍斐, 张继新, 等. 113例早期结直肠癌及癌前病变内镜黏膜下剥离术标本处理及病理学评估[J]. 中华消化内镜杂志, 2018, 35 (7): 470- 476.
doi: 10.3760/cma.j.issn.1007-5232.2018.07.004 |
| 11 |
Nagtegaal ID , Odze RD , Klimstra D , et al. The 2019 WHO classification of tumours of the digestive system[J]. Histopathology, 2020, 76 (2): 182- 188.
doi: 10.1111/his.13975 |
| 12 |
Sano T , Aiko T . New Japanese classifications and treatment guidelines for gastric cancer: Revision concepts and major revised points[J]. Gastric Cancer, 2011, 14 (2): 97- 100.
doi: 10.1007/s10120-011-0040-6 |
| 13 |
Sung H , Ferlay J , Siegel RL , et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71 (3): 209- 249.
doi: 10.3322/caac.21660 |
| 14 |
Ito Y , Miyashiro I , Ishikawa T , et al. Determinant factors on differences in survival for gastric cancer between the United States and Japan using nationwide databases[J]. J Epidemiol, 2021, 31 (4): 241- 248.
doi: 10.2188/jea.JE20190351 |
| 15 |
Hong S , Won YJ , Lee JJ , et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2018[J]. Cancer Res Treat, 2021, 53 (2): 301- 315.
doi: 10.4143/crt.2021.291 |
| 16 | 曹晖, 张子臻, 赵恩昊, 等. 对早期胃癌内镜治疗的评价、思考及展望[J]. 中国实用外科杂志, 2022, 42 (10): 1097- 1103. |
| 17 |
Hasuike N , Ono H , Boku N , et al. A non-randomized confirmatory trial of an expanded indication for endoscopic submucosal dissection for intestinal-type gastric cancer (cT1a): The Japan clinical oncology group study (JCOG0607)[J]. Gastric Cancer, 2018, 21 (1): 114- 123.
doi: 10.1007/s10120-017-0704-y |
| 18 |
Lee CK , Chung IK , Lee SH , et al. Is endoscopic forceps biopsy enough for a definitive diagnosis of gastric epithelial neoplasia[J]. J Gastroenterol Hepatol, 2010, 25 (9): 1507- 1513.
doi: 10.1111/j.1440-1746.2010.006367.x |
| 19 |
Zhao G , Xue M , Hu Y , et al. How Commonly is the diagnosis of gastric low grade dysplasia upgraded following endoscopic resection? A meta-analysis[J]. PLoS One, 2015, 10 (7): e0132699.
doi: 10.1371/journal.pone.0132699 |
| 20 |
Jung SH , Chung WC , Lee KM , et al. Risk factors in malignant transformation of gastric epithelial neoplasia categorized by the revised Vienna classification: endoscopic, pathological, and immunophenotypic features[J]. Gastric Cancer, 2010, 13 (2): 123- 130.
doi: 10.1007/s10120-010-0550-7 |
| 21 |
Sung JK . Diagnosis and management of gastric dysplasia[J]. Korean J Intern Med, 2016, 31 (2): 201- 209.
doi: 10.3904/kjim.2016.021 |
| 22 |
国家消化系疾病临床医学研究中心(上海), 国家消化道早癌防治中心联盟, 中华医学会消化病学分会幽门螺杆菌学组, 等. 中国胃黏膜癌前状态和癌前病变的处理策略专家共识(2020年)[J]. 中华消化杂志, 2020, 40 (11): 731- 741.
doi: 10.3760/cma.j.cn311367-20200915-00554 |
| 23 | De Marco MO , Tustumi F , Brunaldi VO , et al. Prognostic factors for ESD of early gastric cancers: A systematic review and meta-analysis[J]. Endosc Int Open, 2020, 8 (9): e1144- e1155. |
| [1] | Wei-hua HOU,Shu-jie SONG,Zhong-yue SHI,Mu-lan JIN. Clinicopathological features of Helicobacter pylori-negative early gastric cancer [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 292-298. |
| [2] | XUE Jiang,ZHANG Jian-yun,SHI Rui-rui,XIE Xiao-yan,BAI Jia-ying,LI Tie-jun. Clinicopathological analysis of 105 patients with fibrous dysplasia of cranio-maxillofacial region [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 54-61. |
| [3] | WU Jun-yi,YU Miao,SUN Shi-chen,FAN Zhuang-zhuang,ZHENG Jing-lei,ZHANG Liu-tao,FENG Hai-lan,LIU Yang,HAN Dong. Detection of EDA gene mutation and phenotypic analysis in patients with hypohidrotic ectodermal dysplasia [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 24-33. |
| [4] | KE Yan,ZHANG Qiang,MA Yun-qing,LI Ru-jun,TAO Ke,GUI Xian-ge,LI Ke-peng,ZHANG Hong,LIN Jian-hao. Short-term outcomes of total hip arthroplasty in the treatment of Tönnis grade 3 hip osteoarthritis in patients with spondyloepiphyseal dysplasia [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 175-182. |
| [5] | Ying-chao WU,Yun-long CAI,Long RONG,Ji-xin ZHANG,Jin LIU,Xin WANG. Characteristics of lymph node metastasis and evaluating the efficacy of endoscopic submucosal dissection in early gastric cancer [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1093-1097. |
| [6] | Sha ZHU,Zong-sheng XU,Qing XIA,Xiao-jing FANG,Dan-hua ZHAO,Xian-zeng LIU. Clinico-pathological features of temporal lobe epilepsy with enlarged amygdala [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 824-828. |
| [7] | Xin LIU,Jing ZHANG,Ye WANG,He-jun ZHANG,Shi-gang DING,Li-ya Zhou. Characteristics analysis of early gastric cancer under white light endoscopy [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 302-306. |
| [8] | Rui LIU,Jia-yu ZHAI,Xiang-yuan LIU,Zhong-qiang YAO. Progressive pseudorheumatoid dysplasia misdiagnosed asankylosing spondylitis: a case report [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1112-1116. |
| [9] | LI Shi-jie, WANG Jing, LI Zi-yu, BU Zhao-de, SU Xiang-qian, LI Zhong-wu, WU Qi. Application of endoscopic submucosal dissection in treatment of early gastric cancer [J]. Journal of Peking University(Health Sciences), 2015, 47(6): 945-951. |
| [10] | WU Feng-liang, JIANG Liang, YANG Shao-min,LIU Chen,LIU Xiao-guang, WEI Feng,YU Miao, LIU Zhong-jun. Medical therapy of polyostotic fibrous dysplasia of the spinal column [J]. Journal of Peking University(Health Sciences), 2013, 45(6): 950-955. |
|
||