Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (2): 357-361. doi: 10.19723/j.issn.1671-167X.2023.02.023
Previous Articles Next Articles
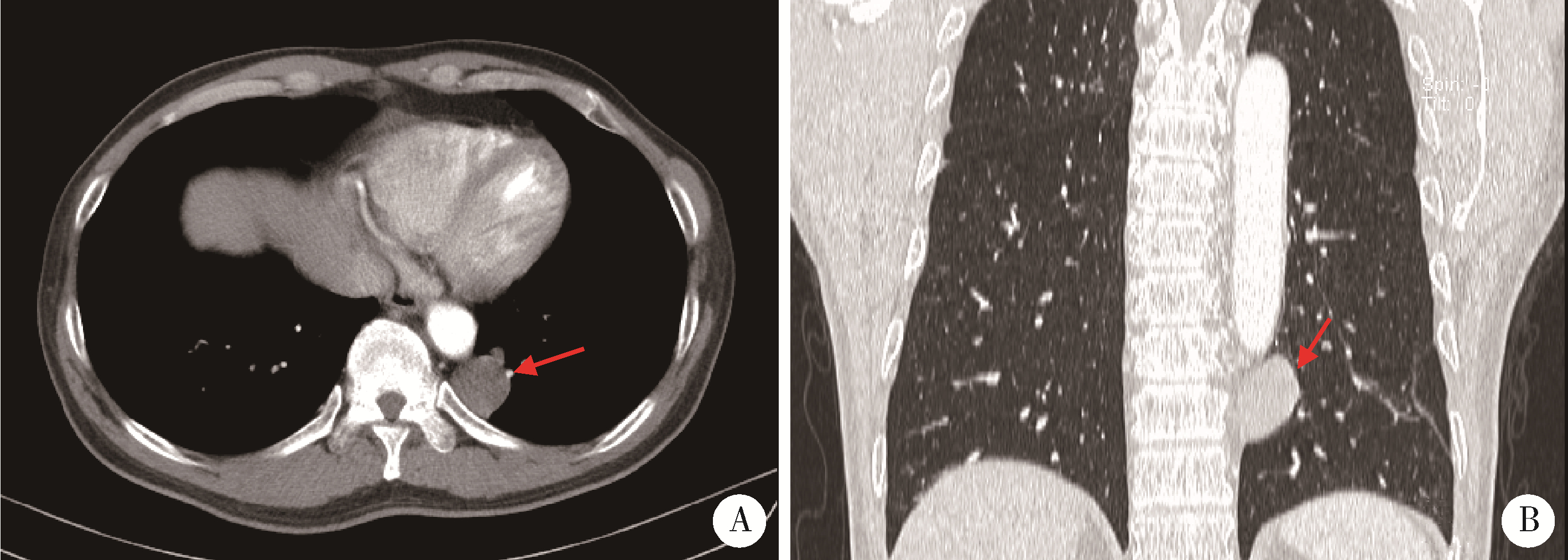
Solid placental transmogrification of the lung: A case report and literature review
Xue-mei HA1,Yong-zheng YAO2,Li-hua SUN1,Chun-yang XIN1,Yan XIONG3,*( )
)
- 1. Department of Pathology, Miyun District Hospital of Beijing, Beijing 101500, China
2. Department of Thoracic Surgery, Miyun District Hospital of Beijing, Beijing 101500, China
3. Department of Pathology, Peking University First Hospital, Beijing 100034, China
CLC Number:
- R734.2
| 1 | McChesney T . Placental transmogrification of the lung: A unique case with remarkable histopathologic features[J]. Lab Invest, 1979, 40, 245- 246. |
| 2 |
Mark EJ , Muller KM , McChesney T , et al. Placentoid bullous lesion of the lung[J]. Hum Pathol, 1995, 26 (1): 74- 79.
doi: 10.1016/0046-8177(95)90117-5 |
| 3 |
Saito Y , Ikeya T , Hoshi E , et al. Placental transmogrification of the lung presenting as a small solitary nodule[J]. Ann Thorac Surg, 2009, 87 (3): 950- 952.
doi: 10.1016/j.athoracsur.2008.07.063 |
| 4 |
Ma DJ , Liu HS , Li SQ , et al. Placental transmogrification of the lung: Case report and systematic review of the literature[J]. Medicine (Baltimore), 2017, 96 (35): e7733.
doi: 10.1097/MD.0000000000007733 |
| 5 |
Yang M , Zhang XT , Liu XF , et al. Placental transmogrification of the lung presenting as a peripheral solitary nodule in a male with the history of trauma: A case report[J]. Medicine (Baltimore), 2018, 97 (18): e0661.
doi: 10.1097/MD.0000000000010661 |
| 6 |
Foschini G , Rodríguez CM , Rubio MM , et al. Placental transmogrification of the lung[J]. Arch Bronconeumol, 2022, 58 (5): 433.
doi: 10.1016/j.arbres.2021.04.004 |
| 7 |
Kim JW , Park IH , Kwon W , et al. Placental transmogrification of the lung[J]. Korean J Radiol, 2013, 14 (6): 977- 980.
doi: 10.3348/kjr.2013.14.6.977 |
| 8 |
Cavazza A , Lantuejoul S , Sartori G , et al. Placental transmogrification of the lung: Clinicopathologic, immunohistochemical and molecular study of two cases, with particular emphasis on the interstitial clear cells[J]. Hum Pathol, 2004, 35 (4): 517- 521.
doi: 10.1016/j.humpath.2003.10.023 |
| 9 |
Ferretti GR , Kocier M , Moro-Sibilot D , et al. Placental transmogrication of the lung: CT-pathologic correlation of a rare pulmonary nodule[J]. AJR Am J Roentgenol, 2004, 183 (1): 99- 101.
doi: 10.2214/ajr.183.1.1830099 |
| 10 |
Xu R , Murray M , Jagirdar J , et al. Placental transmogrification of the lung is a histologic pattern frequently associated with pulmonary fibrochondromatous hamartoma[J]. Arch Pathol Lab Med, 2002, 126 (5): 562- 566.
doi: 10.5858/2002-126-0562-PTOTLI |
| 11 |
Shapiro M , Vidal C , Lipskar AM , et al. Placental transmogrification of the lung presenting as emphysema and a lung mass[J]. Ann Thorac Surg, 2009, 87 (2): 615- 616.
doi: 10.1016/j.athoracsur.2008.05.076 |
| 12 | Narula N , Ngu S , Sharma D , et al. Placental transmogrification of the lung associated with unilateral pleural effusion: A case report with a comprehensive review of the literature[J]. Respir Med Case Rep, 2019, 26, 161- 164. |
| 13 |
Marchevsky AM , Guintu R , Koss M , et al. Swyer-James (MacLeod) syndrome with placental transmogrification of the lung: A case report and review of the literature[J]. Arch Pathol Lab Med, 2005, 129 (5): 686- 689.
doi: 10.5858/2005-129-0686-SMSWPT |
| 14 |
Hamza A , Khawar S , Khurram MS , et al. Pulmonary placental trans-mogrification associated with adenocarcinoma of the lung: A case report with a comprehensive review of the literature[J]. Autops Case Rep, 2017, 7 (3): 44- 49.
doi: 10.4322/acr.2017.027 |
| 15 | Mudawi D , Touqeer R , Montero-Fernandez A , et al. Image of the month: Placental transmogrification of the lung: A rare cause of cystic lung disease[J]. Clin Med (Lond), 2020, 20 (6): 603- 604. |
| 16 |
Jenkins JM , Attia RQ , Green A , et al. A case of pulmonary placental transmogrification[J]. Asian Cardiovasc Thorac Ann, 2016, 24 (8): 811- 813.
doi: 10.1177/0218492316661462 |
| 17 |
Horsley WS , Gal AA , Mansour KA , et al. Unilateral giant bullous emphysema with placental transmogrification of the lung[J]. Ann Thorac Surg, 1997, 64 (1): 226- 228.
doi: 10.1016/S0003-4975(97)00274-9 |
| 18 |
Fidler ME , Koomen M , Sebek B , et al. Placental transmogrification of the lung, a histologic variant of giant bullous emphysema. Clinicopathological study of three further cases[J]. Am J Surg Pathol, 1995, 19 (5): 563- 570.
doi: 10.1097/00000478-199505000-00008 |
| 19 |
Moneghini L , Tosi D , Graziani D , et al. CD10 and CD34 as markers in vascular malformations with PIK3CA and TEK mutations[J]. Hum Pathol, 2020, 99, 98- 106.
doi: 10.1016/j.humpath.2020.04.001 |
| 20 |
Kadota K , Buitrago D , Lee MC , et al. Tumoral CD10 expression correlates with high-grade histology and increases risk of recurrence in patients with stage Ⅰ lung adenocarcinoma[J]. Lung Cancer, 2015, 89 (3): 329- 336.
doi: 10.1016/j.lungcan.2015.06.003 |
| [1] | Hua ZHONG, Yuan LI, Liling XU, Mingxin BAI, Yin SU. Application of 18F-FDG PET/CT in rheumatic diseases [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 853-859. |
| [2] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [3] | Qi WU,Yue-ming CAI,Juan HE,Wen-di HUANG,Qing-wen WANG. Correlation between dyslipidemia and rheumatoid arthritis associated interstitial lung disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 982-992. |
| [4] | Wen-gen LI,Xiao-dong GU,Rui-qiang WENG,Su-dong LIU,Chao CHEN. Expression and clinical significance of plasma exosomal miR-34-5p and miR-142-3p in systemic sclerosis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1022-1027. |
| [5] | Bo-han NING,Qing-xia ZHANG,Hui YANG,Ying DONG. Endometrioid adenocarcinoma with proliferated stromal cells, hyalinization and cord-like formations: A case report [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 366-369. |
| [6] | Wei-hua HOU,Shu-jie SONG,Zhong-yue SHI,Mu-lan JIN. Clinicopathological features of Helicobacter pylori-negative early gastric cancer [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 292-298. |
| [7] | Qi SHEN,Yi-xiao LIU,Qun HE. Mucinous tubular and spindle cell carcinoma of kidney: Clinicopathology and prognosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 276-282. |
| [8] | Qian SU,Xin PENG,Chuan-xiang ZHOU,Guang-yan YU. Clinicopathological characteristics and prognosis of non-Hodgkin lymphoma in oral and maxillofacial regions: An analysis of 369 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 13-21. |
| [9] | Er-shu BO,Peng HONG,Yu ZHANG,Shao-hui DENG,Li-yuan GE,Min LU,Nan LI,Lu-lin MA,Shu-dong ZHANG. Clinicopathological features and prognostic analysis of papillary renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 615-620. |
| [10] | ZHANG Pu-li,YANG Hong-xia,ZHANG Li-ning,GE Yong-peng,PENG Qing-lin,WANG Guo-chun,LU Xin. Value of serum YKL-40 in the diagnosis of anti-MDA5-positive patients with dermatomyositis complicated with severe pulmonary injury [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1055-1060. |
| [11] | XIA Fang-fang,LU Fu-ai,LV Hui-min,YANG Guo-an,LIU Yuan. Clinical characteristics and related factors of systemic lupus erythematosus with interstitial pneumonia [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 266-272. |
| [12] | Hong ZHU,Li-juan ZHAO,Yan ZHOU,Yao CHEN. Significance of anti-carbamylated protein antibodies in patients with rheumatoid arthritis-associated intersitial lung disease [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1003-1007. |
| [13] | Qian SU,Xin PENG,Chuan-xiang ZHOU,Guang-yan YU. Clinicopathological features and possible prognostic factors in parotid lymphomas [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 35-42. |
| [14] | NI Lian-fang, WANG He, LI Hong, ZHANG Zhi-gang, LIU Xin-min. Clinical analysis of pulmonary cryptococcosis in non-human immunodeficiency virus infection patients [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 855-860. |
| [15] | HUANG Zi-xiong, DU Yi-qing, ZHANG Xiao-peng, LIU Shi-jun, XU Tao. Clinical and pathological analysis of renal cell carcinoma bone metastasis [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 811-815. |
|
||