| [1] |
Silu CHEN, Haiju WANG, Yucai WU, Zhihua LI, Yanbo HUANG, Yuhui HE, Yangyang XU, Xuesong LI, Hua GUAN.
Etiological analysis of hydronephrosis in adults: A single-center cross-sectional study
[J]. Journal of Peking University (Health Sciences), 2024, 56(5): 913-918.
|
| [2] |
Wei ZUO,Fei GAO,Chang-wei YUAN,Sheng-wei XIONG,Zhi-hua LI,Lei ZHANG,Kun-lin YANG,Xin-fei LI,Liang LIU,Lai WEI,Peng ZHANG,Bing WANG,Ya-ming GU,Hong-jian ZHU,Zheng ZHAO,Xue-song LI.
Trends in upper urinary tract reconstruction surgery over a decade based on a multi-center database
[J]. Journal of Peking University (Health Sciences), 2022, 54(4): 692-698.
|
| [3] |
Zhi-hua LI,Chun-ru XU,Yin LIU,Hua GUAN,Meng ZHANG,Xin-yan CHE,Qi TANG,Yan-bo HUANG,Xue-song LI,Li-qun HOU.
Correlation between daily fluid intake behavioral habits and pathological characteristics of upper tract urothelial carcinoma
[J]. Journal of Peking University (Health Sciences), 2022, 54(4): 621-627.
|
| [4] |
Xiang DAI,Fei WANG,Yi-qing DU,Yu-xuan SONG,Tao XU.
Correlation between adipokine and clinicopathological features and prognosis in upper tract urothelial carcinoma
[J]. Journal of Peking University (Health Sciences), 2022, 54(4): 605-614.
|
| [5] |
Si-da CHENG,Xin-fei LI,Sheng-wei XIONG,Shu-bo FAN,Jie WANG,Wei-jie ZHU,Zi-ao LI,Guang-pu DING,Ting YU,Wan-qiang LI,Yong-ming SUN,Kun-lin YANG,Lei ZHANG,Han HAO,Xue-song LI,Li-qun ZHOU.
Robot-assisted laparoscopic upper urinary tract reconstruction surgery: A review of 108 cases by a single surgeon
[J]. Journal of Peking University (Health Sciences), 2020, 52(4): 771-779.
|
| [6] |
Jun-hui ZHANG,Yi-hang JIANG,Yu-guang JIANG,Ji-qing ZHANG,Ning KANG.
Clinical outcomes of simultaneous bilateral endoscopic surgery for bilateral upper urinary tract calculi
[J]. Journal of Peking University (Health Sciences), 2020, 52(4): 672-677.
|
| [7] |
Bing-wei HUANG,Jie WANG,Peng ZHANG,Zhe LI,Si-cheng BI,Qiang WANG,Cai-bo YUE,Kun-lin YANG,Xue-song LI,Li-qun ZHOU.
Application of indocyanine green in complex upper urinary tract repair surgery
[J]. Journal of Peking University (Health Sciences), 2020, 52(4): 651-656.
|
| [8] |
Bao GUAN,Mai WENG,Hang FAN,Ding PENG,Dong FANG,Geng-yan XIONG,Xue-song LI,Li-qun ZHOU.
Evaluating the impact of preoperative anemia on the prognosis of upper tract urothelial carcinoma following radical nephroureterectomy: A single-center retrospective study of 686 patients
[J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1056-1061.
|
| [9] |
Si-da CHENG,Wan-qiang LI,Li MU,Guang-pu DING,Bo ZHANG,Cheng SHEN,Ze-wei YING,Kun-lin YANG,Han HAO,Xue-song LI,Li-qun ZHOU.
Application of totally extraperitoneal renal autotransplantation with Boari flap-pelvis anastomosis in upper urinary tract urothelial carcinomas treatment
[J]. Journal of Peking University(Health Sciences), 2019, 51(4): 758-763.
|
| [10] |
Run-zhuo MA,Hai-zhui XIA,Min LU,Zhi-ying ZHANG,Qi-ming ZHANG,Jian LU,Guo-liang WANG,Lu-lin MA.
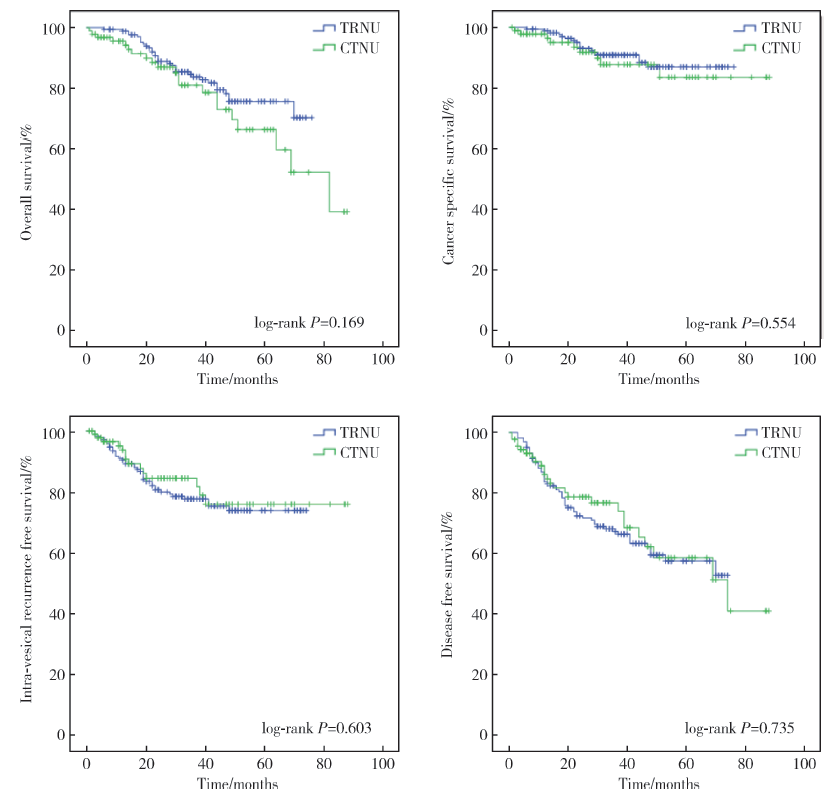
Impact of diagnostic ureteroscopy and biopsy on radical nephroureterectomy of upper tract urothelial carcinoma
[J]. Journal of Peking University(Health Sciences), 2019, 51(4): 665-672.
|
| [11] |
Guang-pu DING,Si-da CHENG,Dong FANG,Kun-lin YANG,Xue-song LI,Hui-xia ZHOU,Qian ZHANG,Xiong-jun YE,Li-qun ZHOU.
Review of upper urinary modified minimal invasive surgical technology
[J]. Journal of Peking University(Health Sciences), 2019, 51(4): 610-614.
|
| [12] |
TANG Xing-guo, YAN Ye, QIU Min, LU Jian, LU Min, HOU Xiao-fei, HUANG Yi, MA Lu-lin.
Retrospective study of young bladder urothelial carcinoma from a single center within 16 years
[J]. Journal of Peking University(Health Sciences), 2018, 50(4): 630-633.
|
| [13] |
MA Run-zhuo, QIU Min, HE Wei, YANG Bin, XIA Hai-zhui, ZOU Da, LU Min, MA Lu-lin1, LU Jian.
Ureteroscope can assist risk stratification in upper tract urothelial carcinoma
[J]. Journal of Peking University(Health Sciences), 2017, 49(4): 632-637.
|
| [14] |
GUAN Bao, CAO Zhen-peng, PENG Ding, LI Yi-fan, ZHAN Yong-hao, LIU Li-bo, HE Shi-ming, XIONG Geng-yan, LI Xue-song, ZHOU Li-qun.
Prognostic factors of patients with T2N0M0 upper tract urothelial carcinoma: a single-center retrospective study of 235 patients
[J]. Journal of Peking University(Health Sciences), 2017, 49(4): 603-607.
|
| [15] |
LIU Jia-yuan, PENG Xiang, NING Xiang-hui, LI Teng, PENG Shuang-he, WANG Jiang-yi, LIU Sheng-jie, DING Yi, CAI Lin, GONG Kan.
Clinical value of fluorescence in situ hybridization positive of exfoliated urothelial cells in urothelial carcinoma
[J]. Journal of Peking University(Health Sciences), 2017, 49(4): 585-589.
|
 ),Xue-song LI2,△(
),Xue-song LI2,△( )
)