Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (1): 153-160. doi: 10.19723/j.issn.1671-167X.2022.01.024
Previous Articles Next Articles
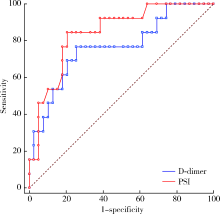
Clinical characteristics of influenza pneumonia in the elderly and relationship between D-dimer and disease severity
LI Jia1,XU Yu2,WANG You-ya3,GAO Zhan-cheng3,△( )
)
- 1. Department of Emergency, Peking University People’s Hospital, Beijing 100044, China
2. Department of Pulmonary and Critical Care Medicine, Beijing Jishuitan Hospital, Beijing 100035, China
3. Department of Pulmonary and Critical Care Medicine, Peking University People’s Hospital, Beijing 100044, China
CLC Number:
- R563.1
| [1] |
Luliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study[J]. Lancet, 2018, 391(10127):1285-1300.
doi: 10.1016/S0140-6736(17)33293-2 |
| [2] |
Gefenaite G, Pistol A, Popescu R, et al. Estimating burden of influenza-associated influenza-like illness and severe acute respiratory infection at public healthcare facilities in Romania during the 2011/12-2015/16 influenza seasons[J]. Influenza Other Respir Viruses, 2018, 12(1):183-192.
doi: 10.1111/irv.2018.12.issue-1 |
| [3] |
Loubet P, Samihlenzi N, Galtier F, et al. Factors associated with poor outcomes among adults hospitalized for influenza in France: A three-year prospective multicenter study[J]. J Clin Virol, 2016, 79:68-73.
doi: S1386-6532(16)30069-5 pmid: 27105315 |
| [4] | 中华人民共和国国家健康委员会. 流行性感冒诊疗方案(2018年版修订版)[J]. 中华临床感染病杂志, 2019, 12(1):1-5. |
| [5] | 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)[J]. 中华结核和呼吸杂志, 2016, 39(4):253-279. |
| [6] | 中华医学会血液学分会血栓与止血学组. 弥散性血管内凝血诊断中国专家共识(2017年版)[J]. 中华血液学杂志, 2017, 38(5):361-363. |
| [7] | Palevsky PM, Liu KD, Brophy PD, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury[J]. Am J Kindney Dis, 2013, 61(5):649-672. |
| [8] |
Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008[J]. Crit Care Med, 2008, 36(1):296-327.
pmid: 18158437 |
| [9] |
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: Advances in diagnosis and treatment[J]. JAMA, 2018, 319(7):698-710.
doi: 10.1001/jama.2017.21907 |
| [10] |
Childs A, Zullo AR, Joyce NR, et al. The burden of respiratory infections among older adults in long-term care: A systematic review[J]. BMC Geriatr, 2019, 19(1):210.
doi: 10.1186/s12877-019-1236-6 |
| [11] |
Chow EJ, Doyle JD, Uyeki TM. Influenza virus-related critical illness: prevention, diagnosis, treatment[J]. Crit Care, 2019, 23(1):214.
doi: 10.1186/s13054-019-2491-9 |
| [12] | Czaja CA, Miller L, Alden N, et al. Age-related differences in hospitalization rates, clinical presentation, outcomes among older adults hospitalized with influenza: U.S. Influenza Hospitalization Surveillance Network(FluSurv-NET)[J]. Open Forum Infect Dis, 2019, 6(7): ofz225. |
| [13] |
Matsuno O, Kataoka H, Takenaka R, et al. Influence of age on symptoms and laboratory findings at presentation in patients with influenza-associated pneumonia[J]. Arch Gerontol Geriatr, 2009, 49(2):322-325.
doi: 10.1016/j.archger.2008.11.015 |
| [14] |
Talbot HK. Influenza in older adults[J]. Infect Dis Clin North Am, 2017, 31(4):757-766.
doi: 10.1016/j.idc.2017.07.005 |
| [15] |
Aronen M, Viikari L, Kohonen I, et al. Respiratory tract virus infections in the elderly with pneumonia[J]. BMC Geriatrics, 2019, 19(1):111.
doi: 10.1186/s12877-019-1125-z pmid: 30991957 |
| [16] |
Chung JY, Hsu CC, Chen JH, et al. Shock index predicted mortality in geriatric patients with influenza in the emergency department[J]. Am J Emerg Med, 2019, 37(3):391-394.
doi: 10.1016/j.ajem.2018.05.059 |
| [17] |
van Asten L, Luna Pinzon A, de Lange DW, et al. Estimating severity of influenza epidemics from severe acute respiratory infections (SARI) in intensive care units[J]. Crit Care, 2018, 22(1):351.
doi: 10.1186/s13054-018-2274-8 |
| [18] |
Zhou F, Li H, Gu L, et al. Risk factors for nosocomial infection among hospitalised severe influenza A(H1N1)pdm09 patients[J]. Resp Med, 2018, 134:86-91.
doi: 10.1016/j.rmed.2017.11.017 |
| [19] |
Sahuquillo JM, Menéndez R, Méndez R, et al. Age-related risk factors for bacterial aetiology in community-acquired pneumonia[J]. Respirology, 2016, 21(8):1472-1479.
doi: 10.1111/resp.12851 pmid: 27417291 |
| [20] |
Daoud A, Laktineh A, Macrander C, et al. Pulmonary complications of influenza infection: A targeted narrative review[J]. Postgrad Med, 2019, 131(5):299-308.
doi: 10.1080/00325481.2019.1592400 pmid: 30845866 |
| [21] |
Nguyen JL, Yang W, Ito K, et al. Seasonal influenza infections and cardiovascular disease mortality[J]. JAMA Cardiol, 2016, 1(3):274-281.
doi: 10.1001/jamacardio.2016.0433 |
| [22] |
Kilic H, Kanbay A, Karalezli A, et al. Clinical characteristics of 75 pandemic H1N1 influenza patients from Turkey; risk factors for fatality[J]. Turk J Med Sci, 2015, 45(3):562-567.
doi: 10.3906/sag-1401-111 |
| [23] |
Ma S, Lai X, Chen Z, et al. Clinical characteristics of critically ill patients co-infected with SARS-CoV-2 and the influenza virus in Wuhan, China[J]. Int J Infect Dis, 2020, 96(1):683-687.
doi: 10.1016/j.ijid.2020.05.068 |
| [24] |
Zhang L, Yan X, Fan Q, et al. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19[J]. J Thromb Haemost, 2020, 18(6):1324-1329.
doi: 10.1111/jth.v18.6 |
| [25] |
Wang ZF, Su F, Lin XJ, et al. Serum D-dimer changes and prognostic implication in 2009 novel influenza A(H1N1)[J]. Thromb Res, 2011, 127(3):198-201.
doi: 10.1016/j.thromres.2010.11.032 pmid: 21216444 |
| [26] |
Kim MA, Park JS, Lee CW, et al. Pneumonia severity index in viral community acquired pneumonia in adults[J]. PLoS One, 2019, 14(3):e0210102.
doi: 10.1371/journal.pone.0210102 |
| [27] |
Dominguez-Cherit G, De la Torre A, Rishu A, et al. Influenza A(H1N1pdm09)-related critical illness and mortality in Mexico and Canada, 2014[J]. Crit Care Med, 2016, 44(10):1861-1870.
doi: 10.1097/CCM.0000000000001830 pmid: 27359085 |
| [1] | Jiajun LIU, Guokang LIU, Yuhu ZHU. Immune-related severe pneumonia: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 932-937. |
| [2] | Haoyu ZHANG,Yiwen SHI,Wei PAN,Aiping LIU,Xinying SUN,Man LI,Xuxi ZHANG. Factors associated with the care needs of the older adults based on different disability levels [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 431-440. |
| [3] | Ting JING,Hua JIANG,Ting LI,Qianqian SHEN,Lan YE,Yindan ZENG,Wenxin LIANG,Gang FENG,Man-Yau Szeto Ignatius,Yumei ZHANG. Relationship between serum 25-hydroxyvitamin D and handgrip strength in middle-aged and elderly people in five cities of Western China [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 448-455. |
| [4] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [5] | Huameng TANG,Dianqi YUAN,Mingxing WANG,Hanbing YANG,Chao GUO. Sequential mediating role of digital participation and health lifestyle in the relationship between socioeconomic status and depression of older adults [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 230-238. |
| [6] | Jinrong ZHU,Yana ZHAO,Wei HUANG,Weiwei ZHAO,Yue WANG,Song WANG,Chunyan SU. Clinical characteristics of COVID-19 infection in patients undergoing hemodialysis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 267-272. |
| [7] | Yuan PAN,Hang GU,Han XIAO,Lijun ZHAO,Yiman TANG,Wenshu GE. Ubiquitin-specific protease 42 regulates osteogenic differentiation of human adipose-derived stem cells [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 9-16. |
| [8] | Hui-li LIU,Yan-han LV,Xiao-xiao WANG,Min LI. Factors influencing the chronic post-surgical pain after laparoscopic surgery for elderly patients with urinary tract tumors [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 851-856. |
| [9] | Chun-su ZHU,Zhi-wei LIAN,Yi-min CUI. Association between depression and chronic diseases among middle-aged and older Chinese adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 606-611. |
| [10] | Xiao-juan ZHU,Hong ZHANG,Shuang ZHANG,Dong LI,Xin LI,Ling XU,Ting LI. Clinicopathological features and prognosis of breast cancer with human epidermal growth factor receptor 2 low expression [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 243-253. |
| [11] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [12] | Le-qing CAO,Jing-rui ZHOU,Yu-hong CHEN,Huan CHEN,Wei HAN,Yao CHEN,Yuan-yuan ZHANG,Chen-hua YAN,Yi-fei CHENG,Xiao-dong MO,Hai-xia FU,Ting-ting HAN,Meng LV,Jun KONG,Yu-qian SUN,Yu WANG,Lan-ping XU,Xiao-hui ZHANG,Xiao-jun HUANG. Relationship between treatment and prognosis in patients with late-onset severe pneumonia after allogeneic hematopoietic stem cell transplantation [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1013-1020. |
| [13] | Yue WANG,Shuang ZHANG,Hong ZHANG,Li LIANG,Ling XU,Yuan-jia CHENG,Xue-ning DUAN,Yin-hua LIU,Ting LI. Clinicopathological features and prognosis of hormone receptor-positive/human epidermal growth factor receptor 2-negative breast cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 853-862. |
| [14] | Guang-qi LIU,Yuan-jie PANG,Jiang WU,Min LV,Meng-ke YU,Yu-tong LI,Yang-mu HUANG. Trend analysis of influenza vaccination among hospitalized elderly people in Beijing, 2013-2019 [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 505-510. |
| [15] | Jing QIAN,You-jia WEI,Yi-jing CHENG,Yi ZHANG,Bo PENG,Chun-mei ZHU. Analysis of clinical features and risk factors of necrotizing pneumonia in children [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 541-547. |
|
||