Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (1): 177-181. doi: 10.19723/j.issn.1671-167X.2022.01.028
Previous Articles Next Articles
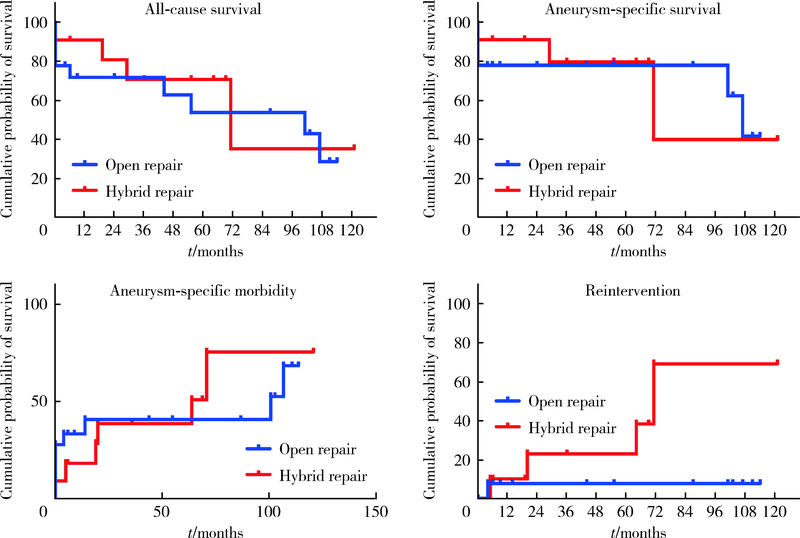
Comparison of the outcomes between open and hybrid approaches in the treatment of thoracoabdominal aortic aneurysms repair
LI Wei-hao,LI Wei( ),ZHANG Xue-min,LI Qing-le,JIAO Yang,ZHANG Tao,JIANG Jing-jun,ZHANG Xiao-ming
),ZHANG Xue-min,LI Qing-le,JIAO Yang,ZHANG Tao,JIANG Jing-jun,ZHANG Xiao-ming
- Department of Vascular Surgery, Peking University People’s Hospital, Beijing 100044, China
CLC Number:
- R654.3
| [1] | 张小明, 张永保, 李清乐, 等. 胸腹主动脉瘤的治疗[J]. 中国血管外科杂志: 电子版, 2014, 6(3):137-142. |
| [2] | 来志超, 孙晓宁, 古丽丹娜·沙艳, 等. 胸腹主动脉瘤的手术方式与外科治疗选择[J]. 中国血管外科杂志: 电子版, 2018, 10(4):233-236. |
| [3] | 赵纪春, 陈熹阳. 胸腹主动脉瘤: 杂交手术现状[J]. 中华血管外科杂志, 2016, 1(2):78-81. |
| [4] |
Di Marco L, Murana G, Leone A, et al. Hybrid repair of thoracoabdominal aneurysm: An alternative strategy for preventing major complications in high risk patients[J]. Int J Cardiol, 2018, 271:31-35.
doi: S0167-5273(18)31046-5 pmid: 30223362 |
| [5] |
Jain A, Flohr TF, Johnston WF, et al. Staged hybrid repair of extensive thoracoabdominal aortic aneurysms secondary to chronic aortic dissection[J]. J Vasc Surg, 2016, 63(1):62-69.
doi: 10.1016/j.jvs.2015.08.060 |
| [6] | Coselli JS, Amarasekara HS, Zhang Q, et al. The impact of preoperative chronic kidney disease on outcomes after Crawford extent Ⅱ thoracoabdominal aortic aneurysm repairs[J]. J Thorac Cardiovasc Surg, 2018, 156(6): 2053-2064. e1. |
| [7] |
Girardi LN, Ohmes LB, Lau C, et al. Open repair of descending thoracic and thoracoabdominal aortic aneurysms in patients with preoperative renal failure[J]. Eur J Cardiothorac Surg, 2017, 51(5):971-977.
doi: 10.1093/ejcts/ezx007 |
| [8] |
Cina CS, Clase CM. Coagulation disorders and blood product use in patients undergoing thoracoabdominal aortic aneurysm repair[J]. Transfus Med Rev, 2005, 19(2):143-154.
doi: 10.1016/j.tmrv.2004.11.003 |
| [9] | 闫兵, 张雷, 黄骏咏, 等. 去分支技术治疗胸腹主动脉瘤[J]. 中华外科杂志, 2014, 52(7):536-538. |
| [10] |
Moulakakis KG, Mylonas SN, Avgerinos ED, et al. Hybrid open endovascular technique for aortic thoracoabdominal pathologies[J]. Circulation, 2011, 124(24):2670-2680.
doi: 10.1161/CIRCULATIONAHA.111.041582 |
| [11] | 张宏鹏, 郭伟, 刘小平, 等. 杂交技术治疗胸腹主动脉瘤[J]. 中华外科杂志, 2009, 47(9):657-660. |
| [1] | Wenjing LI,Baozhou ZHANG,Heng LI,Liangpeng LAI,Hui DU,Ning SUN,Xiaofeng GONG,Ying LI,Yan WANG,Yong WU. Tibiotalocalcaneal arthrodesis for end-stage ankle and hindfoot arthropathy: Short- and mid-term clinical outcomes [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 299-306. |
| [2] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [3] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [4] | Su-huan XU,Bei-bei WANG,Qiu-ying PANG,Li-jun ZHONG,Yan-ming DING,Yan-bo HUANG,Xin-yan CHE. Effect of equal temperature bladder irrigation in patients with transurethral resection of prostate: A meta-analysis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 676-683. |
| [5] | Lei WANG,Tian-dong HAN,Wei-xing JIANG,Jun LI,Dao-xin ZHANG,Ye TIAN. Comparison of safety and effectiveness of active migration technique and in situ lithotripsy technique in the treatment of 1-2 cm upper ureteral calculi by flexible ure-teroscopy [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 553-557. |
| [6] | Hui LI,Yang-xu GAO,Shu-lei WANG,Hong-xin YAO. Surgical complications of totally implantable venous access port in children with malignant tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1167-1171. |
| [7] | ZHUANG Jin-man,LI Tian-run,LI Xuan,LUAN Jing-yuan,WANG Chang-ming,FENG Qi-chen,HAN Jin-tao. Application of Rotarex mechanical thrombectomy system in acute lower limb ische-mia [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1159-1162. |
| [8] | Yan-fang JIANG,Jian WANG,Yong-jian WANG,Jia LIU,Yin PEI,Xiao-peng LIU,Ying-fang AO,Yong MA. Mid-to-long term clinical outcomes and predictors after anterior cruciate ligament revision [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 857-863. |
| [9] | Zheng-da ZHU,Yan GAO,Wen-xiu HE,Xin FANG,Yang LIU,Pan WEI,Zhi-min YAN,Hong HUA. Efficacy and safety of Nocardia rubra cell wall skeleton for the treatment of erosive oral lichen planus [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 964-969. |
| [10] | Wen-min DONG,Ming-rui WANG,Hao HU,Qi WANG,Ke-xin XU,Tao XU. Initial clinical experience and follow-up outcomes of treatment for ureteroileal anastomotic stricture with Allium coated metal ureteral stent [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 637-641. |
| [11] | Jian GAO,Li-bao HU,Chen CHEN,Xin ZHI,Tao XU. Interventional treatment of hemorrhage after percutaneous nephrolithotomy [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 667-671. |
| [12] | Xiao LI,Jia-zeng SU,Yan-yan ZHANG,Li-qi ZHANG,Ya-qiong ZHANG,Deng-gao LIU,Guang-yan YU. Inflammation grading and sialoendoscopic treatment of131I radioiodine-induced sialadenitis [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 586-590. |
| [13] | Kai MA,Xing-ke QU,Qing-quan XU,Liu-lin XIONG,Xiong-jun YE,Li-zhe AN,Wei-nan CHEN,Xiao-bo HUANG. Endoscopic treatment for ureterovesical junction stenosis in patients with kidney transplantation: 13 cases report [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1155-1158. |
| [14] | Ying ZHAN,Yi-tian DU,Zhen-zhen YANG,Chun-li ZHANG,Xian-rong QI. Preparation and characterization of paclitaxel microspheres in situ gel and its antitumor efficacy by local injection [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 477-486. |
| [15] | Chen LIANG,Wei-yu ZHANG,Hao HU,Qi WANG,Zhi-wei FANG,Ke-xin XU. Comparison of effectiveness and complications between two different methods of augmentation cystoplasty [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 293-297. |
|
||