Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (4): 667-671. doi: 10.19723/j.issn.1671-167X.2020.04.013
Previous Articles Next Articles
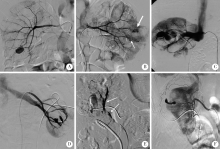
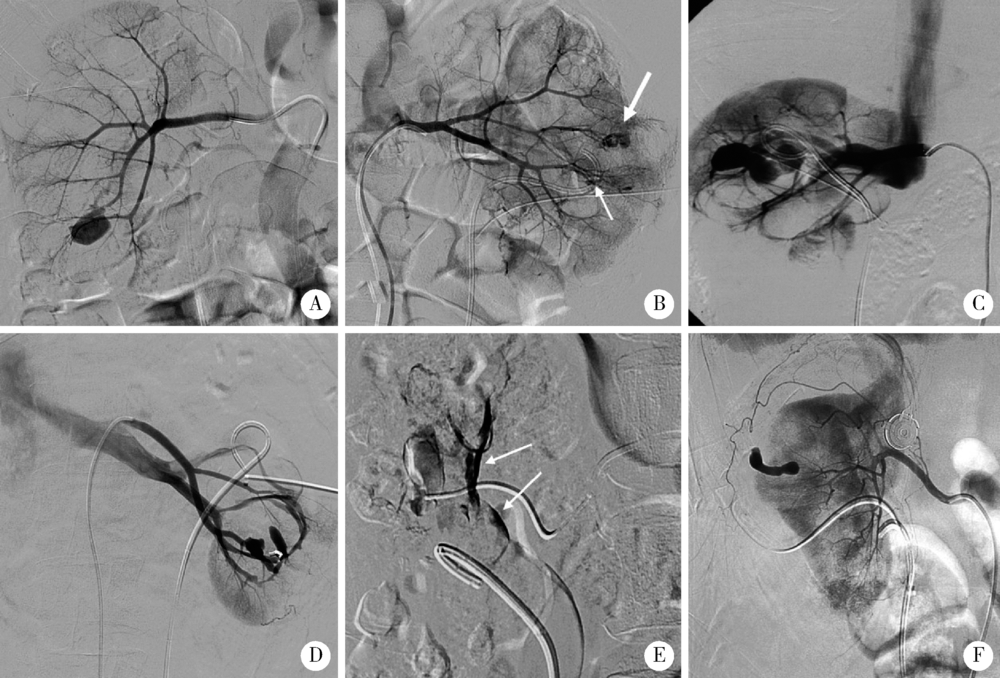
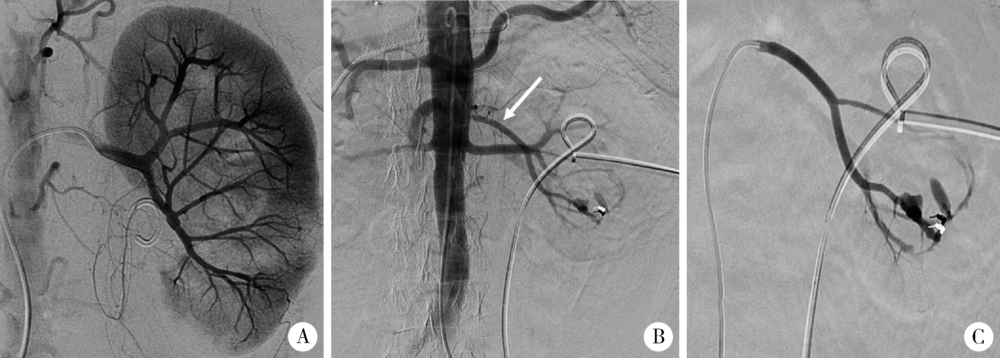
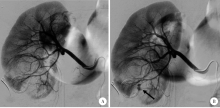
Interventional treatment of hemorrhage after percutaneous nephrolithotomy
Jian GAO1,△( ),Li-bao HU1,Chen CHEN1,Xin ZHI1,Tao XU2,△(
),Li-bao HU1,Chen CHEN1,Xin ZHI1,Tao XU2,△( )
)
- 1. Department of Radiology, Peking University People’s Hospital, Beijing 100044, China
2. Department of Urology, Peking University People’s Hospital, Beijing 100044, China
CLC Number:
- R814.47
| [1] | Un S, Cakir V, Kara C, et al. Risk factors for hemorrhage requiring embolization after percutaneous nephrolithotomy[J]. Can Urol Assoc J, 2015,9(9/10):594-598. |
| [2] | El Tayeb MM, Knoedler JJ, Krambeck AE, et al. Vascular complications after percutaneous nephrolithotomy: 10 years of expe-rience[J]. Urology, 2015,85(4):777-781. |
| [3] | El-Nahas AR, Shokeir AA, Mohsen T, et al. Functional and morphological effects of postpercutaneous nephrolithotomy superselective renal angiographic embolization[J]. Urology, 2008,71(3):408-412. |
| [4] | Kervancioglu S, Gelebek Yilmaz F, Erturhan S. Endovascular management of vascular complications after percutaneous nephrolithotomy[J]. Vasa, 2014,43(6):459-464. |
| [5] | Li L, Zhang Y, Chen Y, et al. A multicentre retrospective study of transcatheter angiographic embolization in the treatment of delayed haemorrhage after percutaneous nephrolithotomy[J]. Eur Radiol, 2015,25(4):1140-1147. |
| [6] | Wang HL, Xu CY, Wang HH, et al. Emergency transcatheter arterial embolization for acute renal hemorrhage[J]. Medicine, 2015,94(42):e1667. |
| [7] | Choi MJ, Kim PH, Shin JH, et al. Angiographic management of percutaneous renal procedure-related bleeding: A single-center experience[J]. Int J Urol, 2019,26(3):406-412. |
| [8] |
El-Nahas AR, Shokeir AA, El-Assmy AM, et al. Postpercuta-neous nephrolithotomy extensive hemorrhage: A study of risk factors[J]. J Urol, 2007,177(2):576-579.
pmid: 17222636 |
| [9] | 任医民, 伍筱梅, 温宇, 等. 经皮肾镜取石术后肾出血栓塞失败的原因分析[J]. 中华医学杂志, 2017,97(1):22-25. |
| [10] |
He ZH, Lei HQ, Lu XB, et al. Analysis of repeated renal arte-riography after percutaneous nephrolithotomy[J]. Urolithiasis, 2017,45(5):495-499.
pmid: 27837249 |
| [11] | Ding XB, Guan JJ, Tian JY, et al. Subcostal artery bleeding after percutaneous nephrolithotomy: A case report and literature review[J]. J Int Med Res, 2018,46(10):4350-4353. |
| [12] | Seetharama MK, Ananthashayana VH, Shivanand G, et al. Interventional radiology in the management of visceral artery pseudo-aneurysms: A review of techniques and embolic materials[J]. Korean J Radiol, 2016,17(3):351-363. |
| [13] | Ganpule AP, Shah DH, Desai MR. Postpercutaneous nephrolithotomy bleeding: Aetiology and management[J]. Curr Opin Urol, 2014,24(2):189-194. |
| [14] | 熊六林, 黄晓波, 叶雄俊, 等. 经皮肾镜术后肾脏严重出血特点及选择性介入栓塞的时机选择(附13例报告)[J]. 北京大学学报(医学版), 2010,42(4):465-468. |
| [1] | Wanyin HOU,Jie DONG. Acquired cystic kidney hemorrhage in peritoneal dialysis patients: A report of three cases [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 546-550. |
| [2] | Kewei CHEN,Shaohui DENG,Zhuo LIU,Hongxian ZHANG,Lulin MA,Shudong ZHANG. Discussion on the surgical timing of rupture and hemorrhage of renal angiomyolipoma [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 326-331. |
| [3] | Min FENG,Zhe CHEN,Yong-jing CHENG. A case of duodenal ulcer as prominent manifestation of IgG4-related disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1125-1129. |
| [4] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [5] | Su-huan XU,Bei-bei WANG,Qiu-ying PANG,Li-jun ZHONG,Yan-ming DING,Yan-bo HUANG,Xin-yan CHE. Effect of equal temperature bladder irrigation in patients with transurethral resection of prostate: A meta-analysis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 676-683. |
| [6] | Yun-peng CUI,Xue-dong SHI,Jia LIU,Chuan MI,Bing WANG,Yuan-xing PAN,Yun-fei LIN. Percutaneous pedicle screw fixation combined expandable tubular retractor in the treatment of spinal metastases [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 530-536. |
| [7] | Hui LI,Yang-xu GAO,Shu-lei WANG,Hong-xin YAO. Surgical complications of totally implantable venous access port in children with malignant tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1167-1171. |
| [8] | YUAN Chang-wei,WANG Ying-jin,ZHANG Shu-jie,SHEN Sheng-li,DUAN Hong-zhou. Clinical outcomes following microsurgery and endovascular embolization in the management of spinal dural arteriovenous fistula: A meta-analysis study [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 304-314. |
| [9] | LI Wei-hao,LI Wei,ZHANG Xue-min,LI Qing-le,JIAO Yang,ZHANG Tao,JIANG Jing-jun,ZHANG Xiao-ming. Comparison of the outcomes between open and hybrid approaches in the treatment of thoracoabdominal aortic aneurysms repair [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 177-181. |
| [10] | DAI Xiang,ZUO Mei-ni,ZHANG Xiao-peng,HU Hao,XU Tao. Comparison of long-term outcomes in different managements of diverticular neck in percutaneous nephrolithotomy for diverticular calculi [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 704-709. |
| [11] | ZHANG Lei,LI Guo-liang,DANG Zong-hui, ,A yong,WU Ling-jie,LIU Li-jun. Analysis of bleeding risk in percutaneous renal biopsy in Tibet [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 298-301. |
| [12] | Wen-min DONG,Ming-rui WANG,Hao HU,Qi WANG,Ke-xin XU,Tao XU. Initial clinical experience and follow-up outcomes of treatment for ureteroileal anastomotic stricture with Allium coated metal ureteral stent [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 637-641. |
| [13] | Ming-rui WANG,Qi WANG,Hao HU,Jin-hui LAI,Yong-xin HE,Jie XIONG,Xian-hui LIU,Shi-jun LIU,Ke-xin XU,Tao XU. Long-term analysis of safety and efficacy of standard percutaneous nephrolithotomy in patients with solitary kidneys [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 663-666. |
| [14] | Kai MA,Xing-ke QU,Qing-quan XU,Liu-lin XIONG,Xiong-jun YE,Li-zhe AN,Wei-nan CHEN,Xiao-bo HUANG. Endoscopic treatment for ureterovesical junction stenosis in patients with kidney transplantation: 13 cases report [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1155-1158. |
| [15] | Yu-hua WANG,Guo-hua ZHANG,Ling-ling ZHANG,Jun-li LUO,Lan GAO. Adrenal hemorrhage in a patient with systemic lupus erythematosus [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1178-1181. |