Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 1074-1081. doi: 10.19723/j.issn.1671-167X.2023.06.019
Previous Articles Next Articles
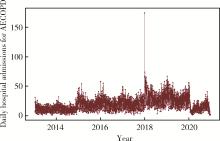
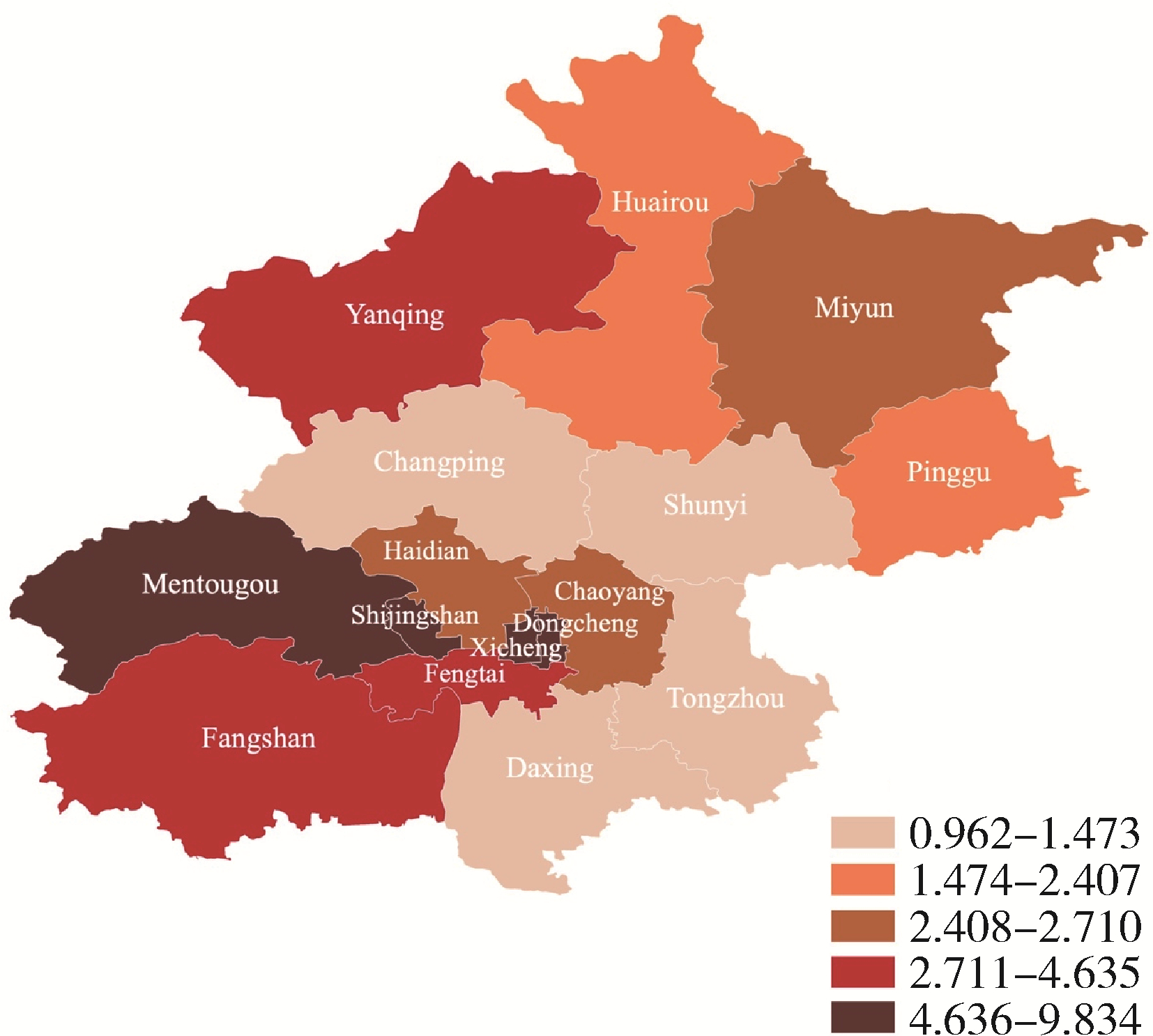
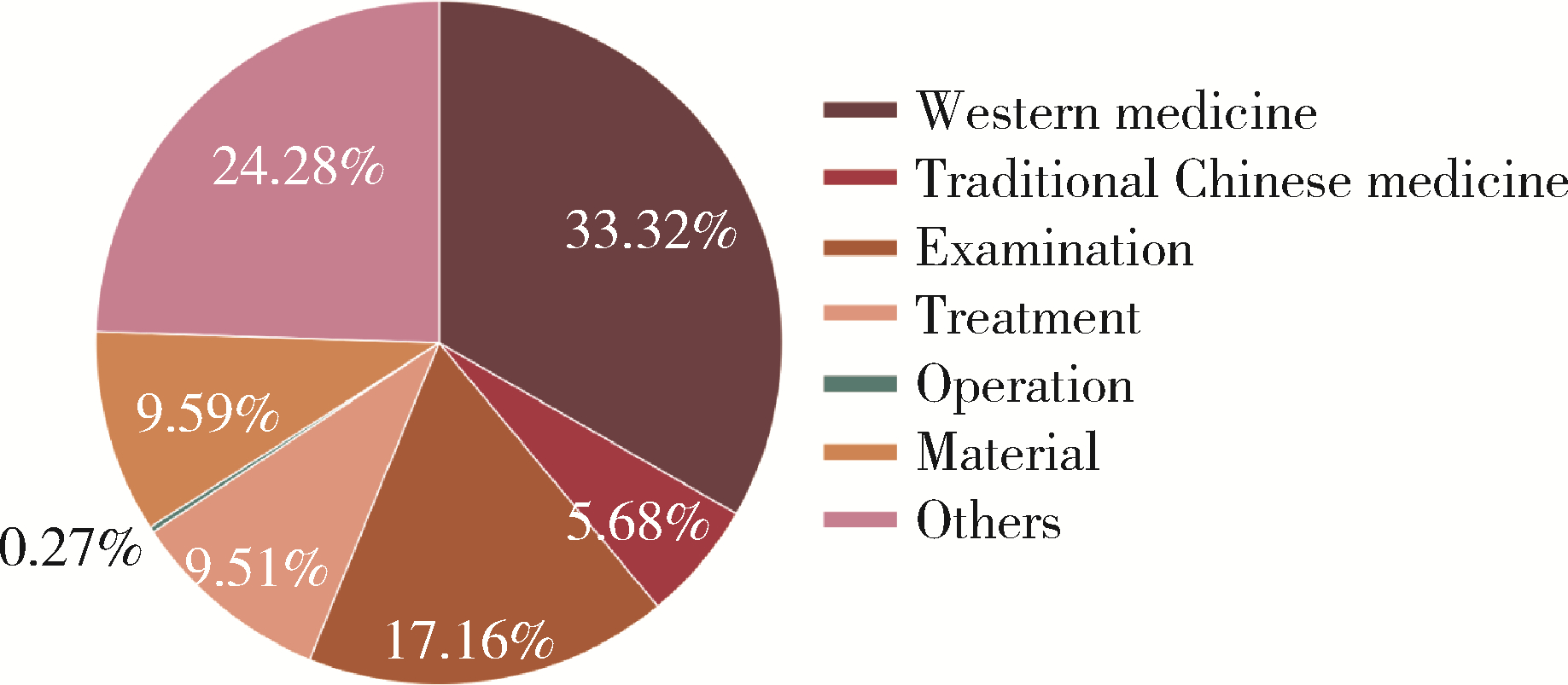
Epidemiology and hospitalization costs analysis of female inpatients with acute exacerbation of chronic obstructive pulmonary disease in Beijing from 2013 to 2020
Zi-kai WANG1,Jia-li MO2,Meng ZHANG1,Ji-ping LIAO1,*( )
)
- 1. Department of Respiratory and Critical Care Medicine, Peking University First Hospital, Beijing, 100034, China
2. Departmant of Pediatrics, Peking University First Hospital, Beijing, 100034, China
CLC Number:
- R563.9
| 1 |
Yin P , Wu J , Wang L , et al. The burden of COPD in China and its provinces: Findings from the global burden of disease study 2019[J]. Front Public Health, 2022, 10, 859499.
doi: 10.3389/fpubh.2022.859499 |
| 2 |
Cao Y , Xing Z , Long H , et al. Predictors of mortality in COPD exacerbation cases presenting to the respiratory intensive care unit[J]. Respir Res, 2021, 22 (1): 77.
doi: 10.1186/s12931-021-01657-4 |
| 3 |
Prediletto I , Giancotti G , Nava S . COPD exacerbation: Why it is important to avoid ICU admission[J]. J Clin Med, 2023, 12 (10): 3369.
doi: 10.3390/jcm12103369 |
| 4 |
Warwick M , Fernando SM , Aaron SD , et al. Outcomes and resource utilization among patients admitted to the intensive care unit following acute exacerbation of chronic obstructive pulmonary disease[J]. J Intensive Care Med, 2021, 36 (9): 1091- 1097.
doi: 10.1177/0885066620944865 |
| 5 |
Celli BR , Fabbri LM , Aaron SD , et al. Differential diagnosis of suspected chronic obstructive pulmonary disease exacerbations in the acute care setting: Best practice[J]. Am J Respir Crit Care Med, 2023, 207 (9): 1134- 1144.
doi: 10.1164/rccm.202209-1795CI |
| 6 |
Wu Y , Wang Z , Zheng Y , et al. Trends in Hospital admissions for chronic obstructive pulmonary diseases after comprehensive tobacco control policies in Beijing, China[J]. Nicotine Tob Res, 2022, 24 (12): 1978- 1984.
doi: 10.1093/ntr/ntac137 |
| 7 |
Scicluna V , Han M . COPD in women: future challenges[J]. Arch Bronconeumol, 2023, 59 (1): 3- 4.
doi: 10.1016/j.arbres.2022.06.008 |
| 8 |
Gao N , Li C , Ji J , et al. Short-term effects of ambient air pollution on chronic obstructive pulmonary disease admissions in Beijing, China (2013-2017)[J]. Int J Chron Obstruct Pulmon Dis, 2019, 14, 297- 309.
doi: 10.2147/COPD.S188900 |
| 9 | Zysman M , Raherison-Semjen C . Women's COPD[J]. Front Med, 2021, 8, 600107. |
| 10 |
Han MK , Postma D , Mannino DM , et al. Gender and chronic obstructive pulmonary disease: Why it matters[J]. Am J Respir Crit Care Med, 2007, 176 (12): 1179- 1184.
doi: 10.1164/rccm.200704-553CC |
| 11 |
Bhatt SP , Bodduluri S , Nakhmani A , et al. Sex differences in airways at chest CT: Results from the COPD gene cohort[J]. Radiology, 2022, 305 (3): 699- 708.
doi: 10.1148/radiol.212985 |
| 12 |
Cheng LL , Liu YY , Su ZQ , et al. Clinical characteristics of tobacco smoke-induced versus biomass fuel-induced chronic obstructive pulmonary disease[J]. J Transl Int Med, 2015, 3 (3): 126- 129.
doi: 10.1515/jtim-2015-0012 |
| 13 |
Kamal R , Srivastava AK , Kesavachandran CN , et al. Chronic obstructive pulmonary disease (COPD) in women due to indoor biomass burning: A meta analysis[J]. Int J Environ Health Res, 2022, 32 (6): 1403- 1417.
doi: 10.1080/09603123.2021.1887460 |
| 14 | Xu M , Ke P , Wang C , et al. Cooking with biomass fuels and mortality among Chinese elderly people: A prospective cohort study[J]. Indoor Air, 2022, 32 (1): e12954. |
| 15 |
Macdonald MI , Shafuddin E , King PT , et al. Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease[J]. Lancet Respir Med, 2016, 4 (2): 138- 148.
doi: 10.1016/S2213-2600(15)00509-3 |
| 16 |
Wang C , Xu J , Yang L , et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health[CPH] study): A national cross-sectional study[J]. Lancet, 2018, 391 (10131): 1706- 1717.
doi: 10.1016/S0140-6736(18)30841-9 |
| 17 |
Rogliani P , Lauro D , Di Daniele N , et al. Reduced risk of COVID-19 hospitalization in asthmatic and COPD patients: A benefit of inhaled corticosteroids[J]. Expert Rev Respir Med, 2021, 15 (4): 561- 568.
doi: 10.1080/17476348.2021.1850275 |
| 18 |
Wang Z , Zhou Y , Luo M , et al. Association of diurnal temperature range with daily hospitalization for exacerbation of chronic respiratory diseases in 21 cities, China[J]. Respir Res, 2020, 21 (1): 251.
doi: 10.1186/s12931-020-01517-7 |
| 19 |
Radicioni G , Ceppe A , Ford AA , et al. Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort[J]. Lancet Respir Med, 2021, 9 (11): 1241- 1254.
doi: 10.1016/S2213-2600(21)00079-5 |
| 20 |
Li M , Chen S , Zhao H , et al. The short-term associations of chronic obstructive pulmonary disease hospitalizations with meteorological factors and air pollutants in Southwest China: A time-series study[J]. Sci Rep, 2021, 11 (1): 12914.
doi: 10.1038/s41598-021-92380-z |
| 21 | Liu Y, Han X, Cui X, et al. Association between air pollutants and acute exacerbation of chronic obstructive pulmonary disease: A time stratified case-crossover design with a distributed lag nonlinear model[J]. Geohealth, 2022, 6(2): e2021GH000529. |
| 22 |
Zhang L , Zhao N , Zhang W , et al. Changes in long-term PM2.5 pollution in the urban and suburban areas of China's three largest urban agglomerations from 2000 to 2020[J]. Remote Sensing, 2022, 14 (7): 1716.
doi: 10.3390/rs14071716 |
| 23 | Jiang X , Xiao H , Segal R , et al. Trends in readmission rates, hospital charges, and mortality for patients with chronic obstructive pulmonary disease (COPD) in Florida from 2009 to 2014[J]. Clin Ther, 2018, 40 (4): 613 e1- 626 e1. |
| 24 | Kim J , Lee TJ , Kim S , et al. The economic burden of chronic obstructive pulmonary disease from 2004 to 2013[J]. J Med Econ, 2016, 19 (2): 103- 110. |
| 25 |
Chen YH , Yao WZ , Cai BQ , et al. Economic analysis in admitted patients with acute exacerbation of chronic obstructive pulmonary disease[J]. Chin Med J (Engl), 2008, 121 (7): 587- 591.
doi: 10.1097/00029330-200804010-00003 |
| 26 |
Schermer TR , Hendriks AJ , Chavannes NH , et al. Probability and determinants of relapse after discontinuation of inhaled corticosteroids in patients with COPD treated in general practice[J]. Prim Care Respir J, 2004, 13 (1): 48- 55.
doi: 10.1016/j.pcrj.2003.11.005 |
| [1] | Zhe WANG,Wei SUN,Xue YANG,Ying SONG,Ai-ping JI,Jie BAI. Clinical analysis of patients with oral and maxillofacial infections in oral emergency [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 543-547. |
| [2] | Xue-zhao JI,Shan LIU,Wan-zhou WANG,Ye-tong ZHAO,Lu-yi LI,Wen-lou ZHANG,Guo-feng SHEN,Fu-rong DENG,Xin-biao GUO. Associations between indoor volatile organic compounds and nocturnal heart rate variability of young female adults: A panel study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 488-494. |
| [3] | Xi-ya SUN,Yi-lu CHEN,Lin ZENG,Li-ying YAN,Jie QIAO,Rong LI,Xu ZHI. Correlation analysis of vitamin D level and anti-Müllerian hormone in infertile female and the role in predicting pregnancy outcome [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 167-173. |
| [4] | Si-wei DENG,Ze-yi CHEN,Zhi-ke LIU,Jian WANG,Lin ZHUO,Shuang-qing GAO,Jia-kuo YU,Si-yan ZHAN. Epidemiological study of bone and joint injury based on urban medical insurance database [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 527-534. |
| [5] | Li-jun ZHAO,Hong-tian LI,Ya-li ZHANG,Yu-bo ZHOU,Jian-meng LIU. Mobile terminal-based survey on the birth characteristics for Chinese newborns [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 813-818. |
| [6] | Wei-yu ZHANG,Qiu-xiang XIA,Hao HU,Jing-wen CHEN,Yi-ran SUN,Ke-xin XU,Xiao-peng ZHANG. Analysis of urodynamic study of female outpatients with lower urinary tract symptoms and follow-up of the patients with detrusor underactive [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 856-862. |
| [7] | Xin-yan CHE,Shi-liang WU,Yu-ke CHEN,Yan-bo HUANG,Yang YANG. A survey of risk factors and quality of life in female medical staff with urinary incontinence [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 706-710. |
| [8] | WANG Dan-dan, GAN Ye-hua, MA Xu-chen, MENG Juan-hong. Association between ADAMTS14 gene polymorphism and the temporomandibular joint osteoarthritis in Chinese Han females [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 279-283. |
| [9] | ZHANG Wei-yu, ZHANG Xiao-peng, CHEN Jing-wen, SUN Yi-ran, WANG Jia, HU Hao, XU Ke-xin. Effect of age on urodynamic parameters of women with urinary incontinence [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 825-829. |
| [10] | ZHOU Yu-Bo, LUO Shu-Sheng, LI Hong-Tian, GAO Yan-Qiu, LIU Jian-Meng. Secular trends of premarital medical examination in China during 1996 and 2013 [J]. Journal of Peking University(Health Sciences), 2015, 47(3): 437-442. |
| [11] | JIA Xiao-Jun, FANG Zhi-Wei, HU Hao, XU Ke-Xin, HUANG Xiao-Bo, WANG Xiao-Feng. Influence of tension-free midurethral sling surgery on sexual function in women with stress urinary incontinence [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 570-573. |
| [12] | HUANG Guang-Lin, MAN Li-Bo, WANG Hai, WANG Jian-Wei, DI Jian-Po, ZHU Xiao-Fei, ZHOU Ning, XU Xiao. Management of female urethral obliteration with the rotary excision appliance [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 574-577. |
| [13] | DENG Qiu-ju, PAN Ya-qi, WANG Chao-yi, LI Feng-lei, LV Shao-jiang, HU Shao-yong, NING Tao, GUO Chuan-hai, HE Zhong-hu, KE Yang. Prevalence and risk factors for hepatitis B in Hua County, Henan Province [J]. Journal of Peking University(Health Sciences), 2013, 45(6): 965-970. |
|
||