Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (6): 1075-1082. doi: 10.19723/j.issn.1671-167X.2024.06.021
Previous Articles Next Articles
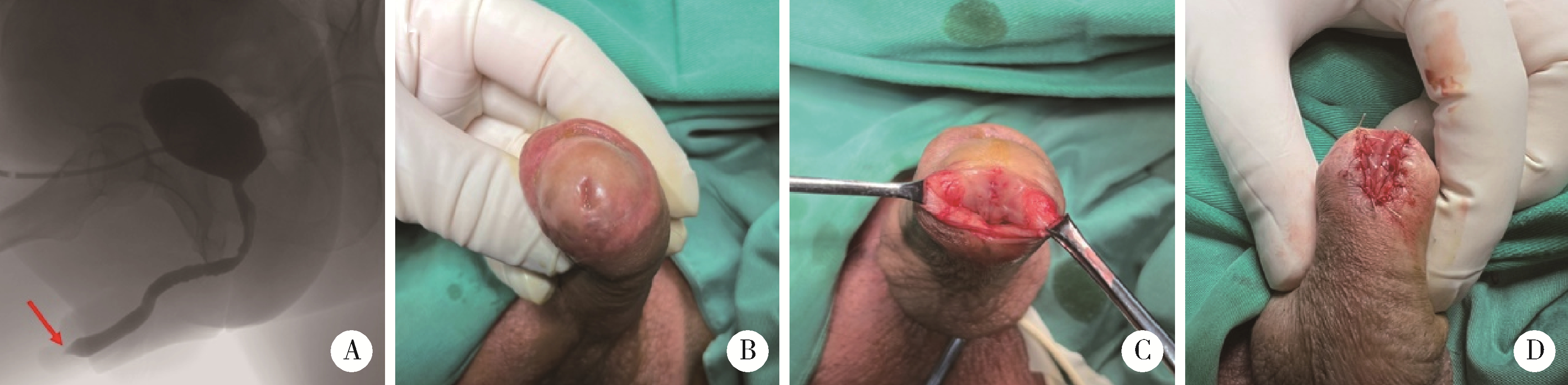
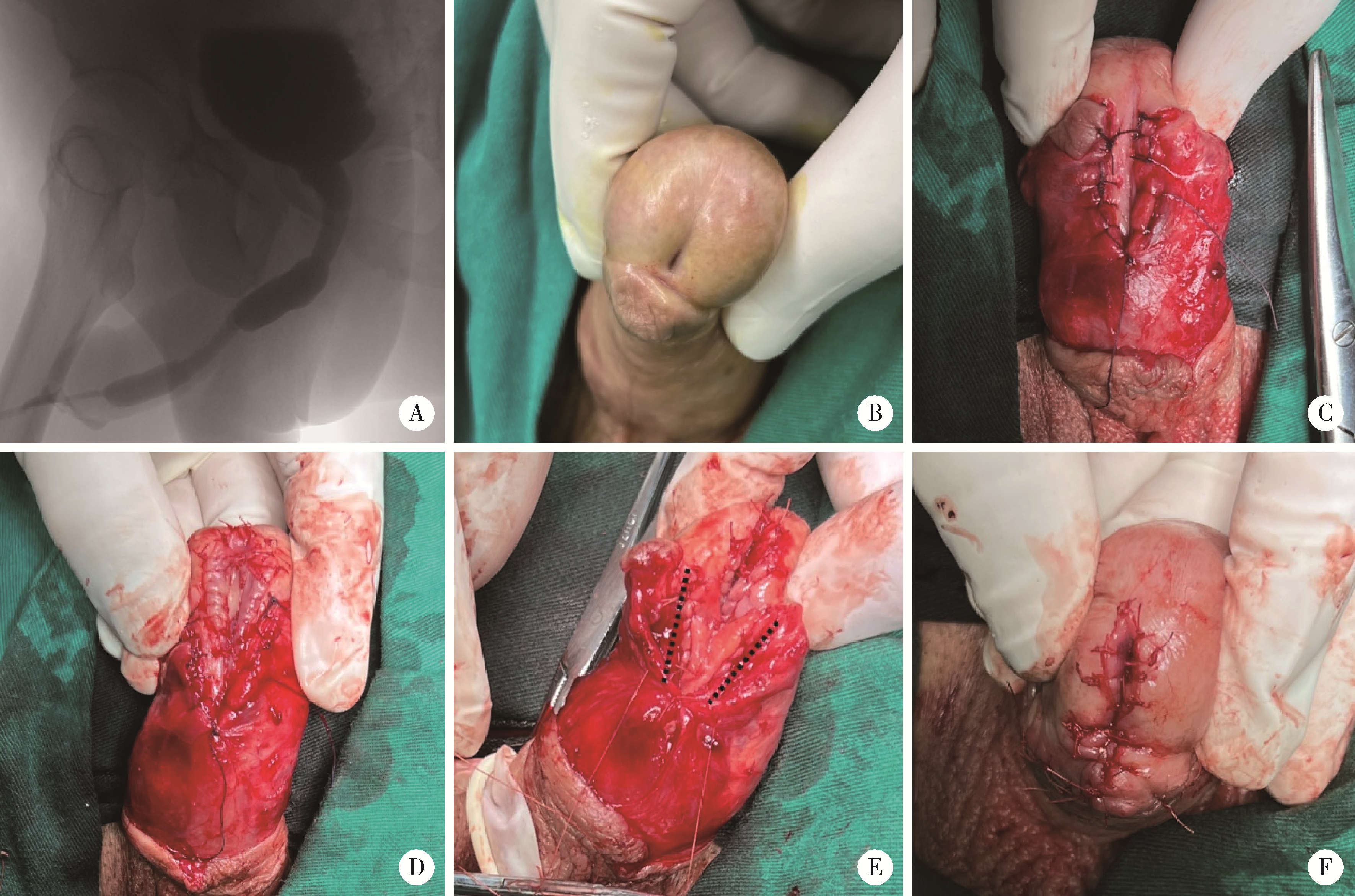
Surgical management of the distal urethral stricture diseases
Jie WANG, Jianwei WANG, Haizhui XIA, Xiao XU, Jianpo ZHAI, Feng HE, Guanglin HUANG*( ), Guizhong LI
), Guizhong LI
- Department of Urology, Beijing Jishuitan Hospital, Capital Medical Universitay, Beijing 100035, China
CLC Number:
- R697.1
| 1 |
Fenton AS , Morey AF , Aviles R , et al.Anterior urethral strictures: Etiology and characteristics[J].Urology,2005,65(6):1055-1058.
doi: 10.1016/j.urology.2004.12.018 |
| 2 |
Abbasi B , Shaw NM , Lui JL , et al.Comparative review of the guidelines for anterior urethral stricture[J].World J Urol,2022,40(8):1971-1980.
doi: 10.1007/s00345-022-03988-3 |
| 3 |
Meeks JJ , Barbagli G , Mehdiratta N , et al.Distal urethroplasty for isolated fossa navicularis and meatal strictures[J].BJU Int,2012,109(4):616-619.
doi: 10.1111/j.1464-410X.2011.10248.x |
| 4 | Dielubanza EJ , Han JS , Gonzalez CM .Distal urethroplasty for fossa navicularis and meatal strictures[J].Transl Androl Urol,2014,3(2):163-169. |
| 5 |
Vetterlein MW , Fisch MM , Zumstein V .Update on the management of penile and meatal strictures[J].Curr Opin Urol,2021,31(5):493-497.
doi: 10.1097/MOU.0000000000000910 |
| 6 | 黄晓东, 吕军, 张小明, 等.MGLSc并发阴茎头部尿道狭窄手术治疗的临床研究[J].中国男科学杂志,2014,(5):3-6. |
| 7 |
Virasoro R , Eltahawy EA , Jordan GH .Long-term follow-up for reconstruction of strictures of the fossa navicularis with a single technique[J].BJU Int,2007,100(5):1143-1145.
doi: 10.1111/j.1464-410X.2007.07078.x |
| 8 | 冯超, 张炯, 谢弘, 等.带蒂岛状转位筋膜皮瓣治疗尿道外口及舟状窝狭窄的临床研究[J].中华泌尿外科杂志,2019,40(6):408-411. |
| 9 | 张楷乐, 傅强.尿道狭窄治疗中的误区[J].中华泌尿外科杂志,2018,39(11):867-869. |
| 10 | 赵亚伟, 刘园园, 马龙, 等.超声在尿道狭窄诊治中的诊断价值[J].中国超声医学杂志,2018,34(12):1126-1128. |
| 11 | 张林琳.评估分析男性尿道狭窄的术前诊断手段: 尿道造影、超声尿道成像和磁共振尿道成像, 谁是诊断的金标准?[J].现代泌尿外科杂志,2022,27(2):166. |
| 12 |
Mikolaj F , Karolina M , Oliwia K , et al.Retrograde urethrography, sonouretrography and magnetic resonance urethrography in evaluation of male urethral strictures. Should the novel methods become the new standard in radiological diagnosis of urethral stricture disease?[J].Int Urol Nephrol,2021,53(12):2423-2435.
doi: 10.1007/s11255-021-02994-5 |
| 13 | 刘启宇, 李养群, 杨喆, 等.V形瓣法在尿道外口和阴茎头成形术中的应用[J].中华整形外科杂志,2016,32(1):49-51. |
| 14 |
Campos-Juanatey F , Osman NI , Greenwell T , et al.European Association of Urology Guidelines on urethral stricture disease (Part 2): Diagnosis, perioperative management, and follow-up in males[J].Eur Urol,2021,80(2):201-212.
doi: 10.1016/j.eururo.2021.05.032 |
| 15 | 张伟, 张志明, 焦点, 等.经尿道口腔黏膜尿道成形术修复尿道外口和舟状窝狭窄的安全性和疗效[J].中华泌尿外科杂志,2023,44(8):581-585. |
| 16 |
Daneshvar M , Simhan J , Blakely S , et al.Transurethral ventral buccal mucosa graft inlay for treatment of distal urethral strictures: International multi-institutional experience[J].World J Urol,2020,38(10):2601-2607.
doi: 10.1007/s00345-019-03061-6 |
| [1] | WANG Jian-wei,XU Xiao,BAO Zheng-qing,LIU Zhen-hua,HE Feng,HUANG Guang-lin,MAN Li-bo. Outcomes of partial pubectomy assisted anastomotic urethroplasty for male patients with pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 798-802. |
| [2] | Jian-wei WANG,Li-bo MAN,Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI. Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 646-650. |
| [3] | Jian-wei WANG,Li-bo MAN,Guang-lin HUANG,Feng HE,Hai WANG,Hai-dong WANG,Xiao XU,Wei LI,Jian-po ZHAI,Zhen-hua LIU. Single-stage repair of penile urethral stricture using combined dorsal onlay oral mucosa grafting with ventral onlay penile skin flap [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 641-645. |
| [4] | WANG Jian-wei, MAN Li-bo, HUANG Guang-lin, WANG Hai, Xu Xiao, ZHU Xiao-fei, LI Wei, LIU Zhen-hua. “3-step” strategy of transperineal anastomotic urethroplasty for the simple pelvic fracture urethral distraction defect in male patients [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 617-620. |
|
||