Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (4): 721-726. doi: 10.19723/j.issn.1671-167X.2025.04.015
Previous Articles Next Articles
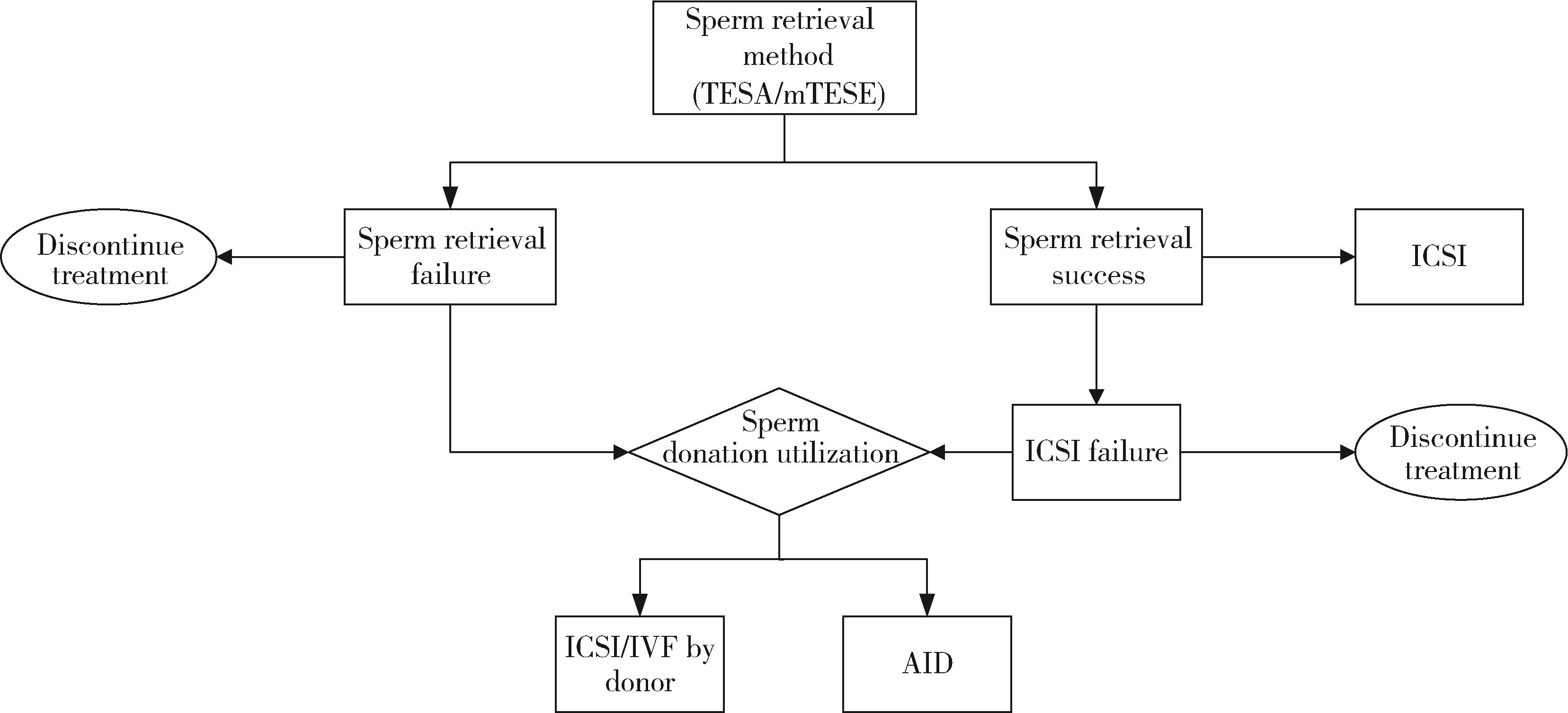
Sperm donation utilization rates in nonobstructive azoospermia patients under different testicular sperm retrieval methods during assisted reproductive technology cycles
Qianxi CHEN1,2, Yan CHEN1,2, Zhongjie ZHENG1,2, Wenhao TANG1,2, Zhen LIU1,2, Kai HONG1,2,*( ), Haocheng LIN1,2,*(
), Haocheng LIN1,2,*( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Center for Reproductive Medicine, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R698.2
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
洪伟, 王莹, 朱琳, 等. 显微镜下睾丸切开取精术在非梗阻性无精子症助孕治疗中的应用[J]. 陆军军医大学学报, 2023, 45 (3): 251- 256.
|
| 8 |
|
| 9 |
|
| 10 |
|
| 11 |
|
| 12 |
|
| 13 |
|
| [1] | MAO Jia-ming, LIU De-feng,ZHAO Lian-ming,HONG Kai, ZHANG Li, MA Lu-lin, JIANG Hui, QIAO Jie. Effect of testicular puncture biopsy on the success rate of microdissection testicular sperm extraction for idiopathic non-obstructive azoospermia [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 613-616. |
|
||