Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (4): 641-645. doi: 10.19723/j.issn.1671-167X.2019.04.008
Previous Articles Next Articles
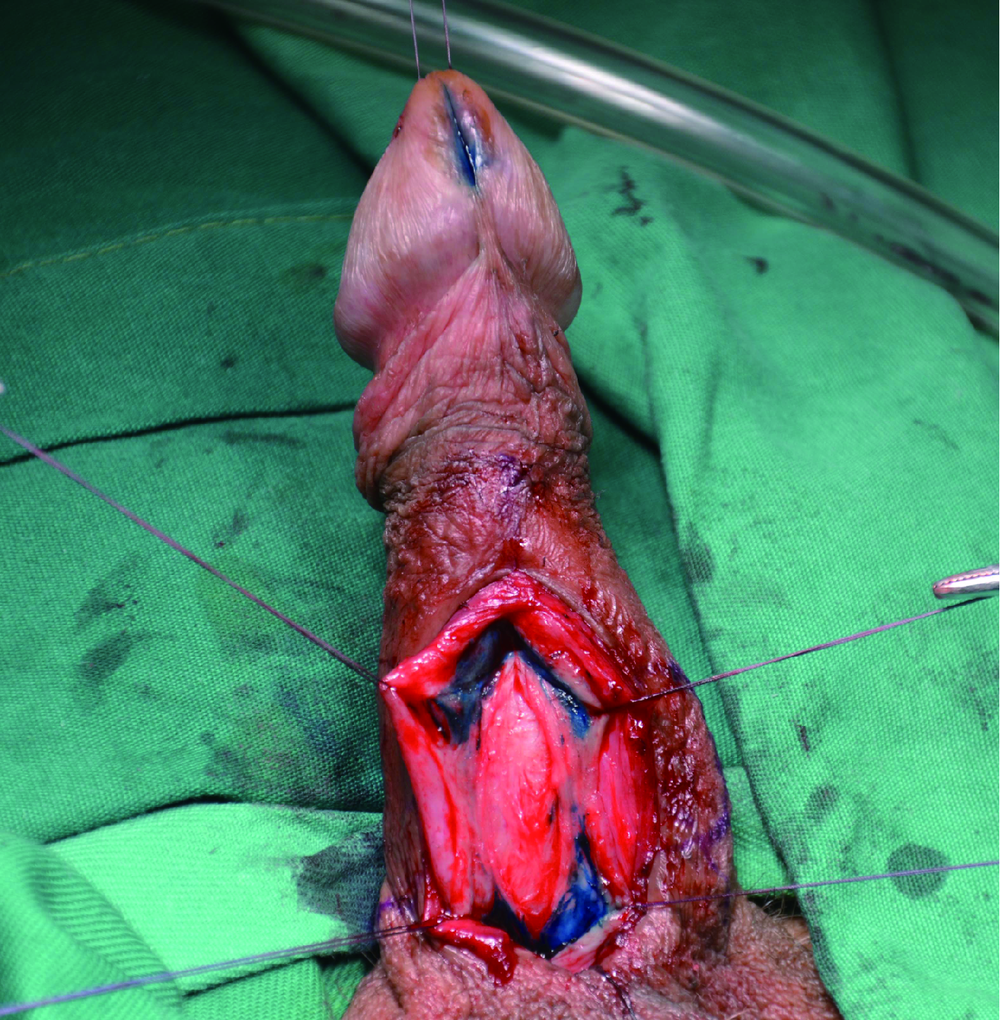
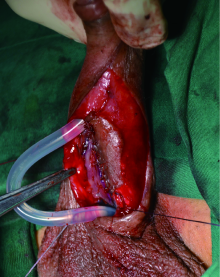
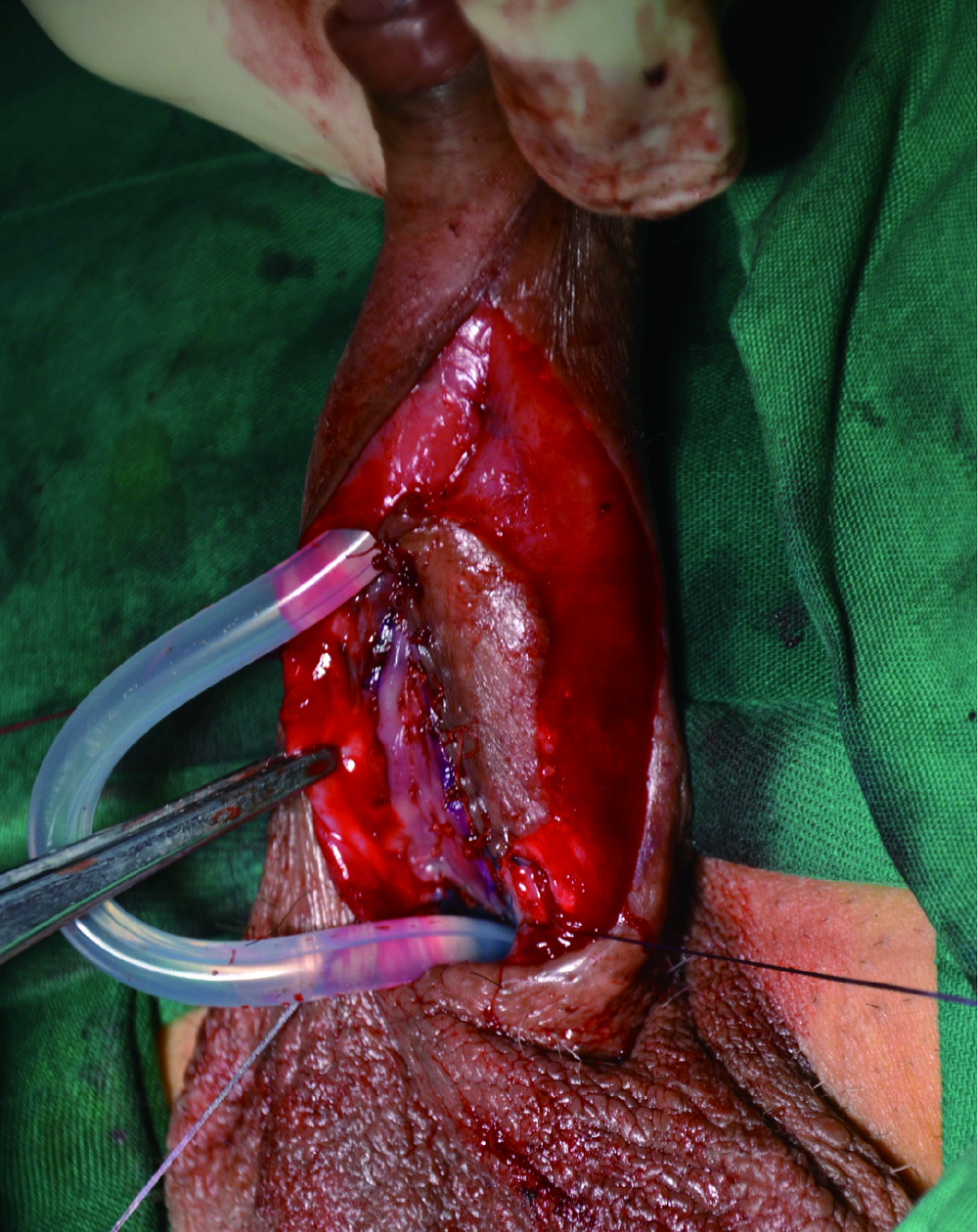
Single-stage repair of penile urethral stricture using combined dorsal onlay oral mucosa grafting with ventral onlay penile skin flap
Jian-wei WANG,Li-bo MAN( ),Guang-lin HUANG,Feng HE,Hai WANG,Hai-dong WANG,Xiao XU,Wei LI,Jian-po ZHAI,Zhen-hua LIU
),Guang-lin HUANG,Feng HE,Hai WANG,Hai-dong WANG,Xiao XU,Wei LI,Jian-po ZHAI,Zhen-hua LIU
- Department of Urology, Beijing Jishuitan Hospital, The Fourth Medical College of Peking University, Beijing 100096, China
CLC Number:
- R699
| [1] | McAninch JW, Morey AF . Penile circular fasciocutaneous skin flap in 1-stage reconstruction of complex anterior urethral strictures[J]. J Urol, 1998,159(4):1209-1213. |
| [2] | Morey AF . Urethral plate salvage with dorsal graft promotes successful penile flaponlay reconstruction of severe pendulous strictures[J]. J Urol, 2001,166(4):1376-1378. |
| [3] | Bayne DB, Gaither TW, Awad MA , et al. Guidelines of guidelines: a review of urethral stricture evaluation, management, and follow-up[J]. Transl Androl Urol, 2017,6(2):288-294. |
| [4] | Horiguchi A . Substitution urethroplasty using oral mucosa graft for male anterior urethral stricture disease: current topics and reviews[J]. Int J Urol, 2017,24(7):493-503. |
| [5] | Erickson BA, Breyer BN , McAninch JW. Single-stage segmental urethral replacement using combined ventral onlay fasciocutaneous flap with dorsal onlay buccal grafting for long segment strictures[J]. BJU Int, 2012,109(9):1392-1396. |
| [6] | Greenwell TJ, Venn AF, Mundy AR . Changing practice in anteriorurethroplasty[J]. BJU Int, 1999,83(6):631-635. |
| [7] | Wessells H, Angermeier KW, Elliott S , et al. Male urethral stricture: American Urological Association Guideline[J]. J Urol, 2017,197(1):182-190. |
| [8] | Gelman J, Sohn W . 1-stage repair of obliterative distal urethral strictures with buccal graft urethral plate reconstruction and simultaneous onlay penile skin flap[J]. J Urol, 2011,186(3):935-938. |
| [9] | Djordjevic ML, Majstorovic M, Stanojevic D , et al. Combined buccal mucosa graft and dorsal penile skin flap for repair of severe hypospadias[J]. Urology, 2008,71(5):821-825. |
| [10] | Soliman MG, Abo Farha MA, El Abd AS , et al. Dorsal onlay urethroplasty using buccal mucosa graft versus penile skin flap for management of long anterior urethral strictures: a prospective randomized study[J]. Scand J Urol, 2014,48(5):466-473. |
| [11] | 满立波, 王建伟 . 图解尿道成形术[M]. 北京: 人民卫生出版社, 2018: 52-59. |
| [1] | WANG Jian-wei,XU Xiao,BAO Zheng-qing,LIU Zhen-hua,HE Feng,HUANG Guang-lin,MAN Li-bo. Outcomes of partial pubectomy assisted anastomotic urethroplasty for male patients with pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 798-802. |
| [2] | Jian-wei WANG,Li-bo MAN,Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI. Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 646-650. |
| [3] | WANG Jian-wei, MAN Li-bo, HUANG Guang-lin, WANG Hai, Xu Xiao, ZHU Xiao-fei, LI Wei, LIU Zhen-hua. “3-step” strategy of transperineal anastomotic urethroplasty for the simple pelvic fracture urethral distraction defect in male patients [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 617-620. |
|
||