Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (5): 925-930. doi: 10.19723/j.issn.1671-167X.2019.05.022
Previous Articles Next Articles
Sinus floor elevation and simultaneous dental implantation: A long term retrospective study of sinus bone gain
Qian WANG1,Dan LI2,Zhi-hui TANG2,△( )
)
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Second Clinical Division, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.1
| [1] | 耿建平 . 上颌窦种植外科学[M]. 江苏: 江苏科学技术出版社, 2010: 1-2. |
| [2] | Boyne PJ, James RA . Grafting of the maxillary sinus floor with autogenous marrow and bone[J]. J Oral Surg, 1980,38(8):613-616. |
| [3] | Tatum H . Maxillary and sinus implant reconstructions[J]. Dent Clin North Am, 1986,30(2):207-229. |
| [4] | Summers RB . A new concept in maxillary implant surgery: the osteotome technique[J]. Compendium, 1994,15(2):152-162. |
| [5] | 范倩倩, 柳忠豪 . 上颌窦黏膜具有成骨潜能的研究进展[J]. 口腔医学研究, 2014,30(5):475-478. |
| [6] | Srouji S, Ben-David D, Lotan R , et al. The innate osteogenic potential of the maxillary sinus (Schneiderian) membrane: an ecto-pic tissue transplant model simulating sinus lifting[J]. Int J Oral Maxillofac Surg, 2010,39(8):793-801. |
| [7] | Lai HC, Zhuang LF, Lv XF , et al. Osteotome sinus floor elevation with or without grafting: a preliminary clinical trial[J]. Clin Oral Impl Res, 2010,21(5):520-526. |
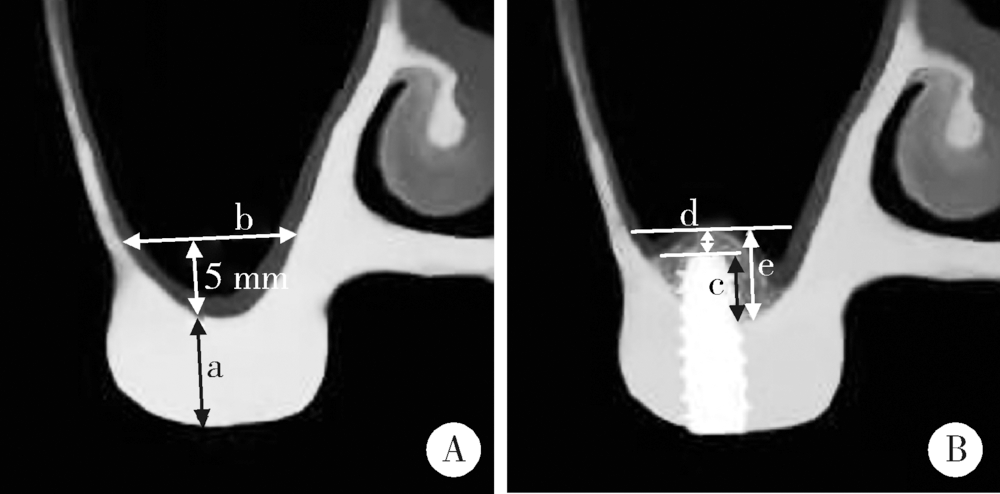
| [8] | Zheng X, Teng M, Zhou F , et al. Influence of maxillary sinus width on transcrestal sinus augmentation outcomes: radiographic evaluation based on cone beam CT[J]. Clin Implant Dent Relat Res, 2016,18(2):292-300. |
| [9] | Nunes LS, Bornstein MM, Sendi P , et al. Anatomical characteristics and dimensions of edentulous sites in the posterior maxillae of patients referred for implant therapy[J]. Int J Periodontics Restorative Dent, 2013,33(3):337-345. |
| [10] | 山道信之, 系濑正通 . 上颌窦底提升术:依据锥形束牙科CT影像诊断的高成功率植牙手术[M]. 张怡泓, 译.北京: 人民军医出版社, 2012: 6-7. |
| [11] | Brizuela A, Martín N, Fernández-Gonzalez FJ , et al. Osteotome sinus floor elevation without grafting material: results of a 2-year prospective study[J]. J Clin Exp Dent, 2014,6(5):e479-e484. |
| [12] | Jeong SM, Choi BH, Li J , et al. A retrospective study of the effects of sinus membrane elevation on bone formation around implants placed in the maxillary sinus cavity[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009,107(3):364-368. |
| [13] | Nedir R, Nurdin N, Abi Najm S , et al. Short implants placed with or without grafting into atrophic sinuses: the 5-year results of a prospective randomized controlled study[J]. Clin Oral Impl Res, 2017,28(7):877-886. |
| [14] | Si MS, Shou YW, Shi YT , et al. Long-term outcomes of osteotome sinus floor elevation without bone grafts: a clinical retrospective study of 4-9 years[J]. Clin Oral Impl Res, 2016,27(11):1392-1400. |
| [15] | Spinelli D, DE Vico G, Condò R , et al. Transcrestal guided sinus lift without grafting materials: a 36 months clinical prospective study[J]. Oral Implantol (Rome), 2016,8(2/3):74-86. |
| [16] | Viña-Almunia J, Maestre-Ferrín L, Alegre-Domingo T , et al. Survival of implants placed with the osteotome technique: an update[J]. Med Oral Patol Oral Cir Bucal, 2012,17(5):e765-e768. |
| [17] | Rammelsberg P, Mahabadi J, Eiffler C , et al. Radiographic monitoring of changes in bone height after implant placement in combination with an internal sinus lift without graft material[J]. Clinical Implant Dentistry and Related Research, 2015,17(1):e267-e274. |
| [18] | 林国芬, 谭包生, 单志钢 , 等. 冲压式上颌窦底提升术同期种植临床分析[J]. 中国口腔颌面外科杂志, 2012,10(3):231-235. |
| [19] | Borges FL, Dias R, Piattelli A , et al. Simultaneous sinus membrane elevation and dental implant placement without bone graft: a 6-month follow-up study[J]. J Periodontol, 2011,82(3):403-412. |
| [20] | Nedir R, Bischof M, Vazquez L , et al. Osteotome sinus floor elevation without grafting material: a 1-year prospective pilot study with ITI implants[J]. Clin Oral Implants Res, 2006,17(6):679-686. |
| [21] | Zill A, Precht C, Beck-Broichsitter B , et al. Implants inserted with graftless osteotome sinus floor elevation: a 5-year post-loading retrospective study[J]. Eur J Oral Implantol, 2016,9(3):277-289. |
| [22] | Chen HH, Lin YC, Lee SY , et al. Influence of sinus floor configuration on grafted bone remodeling after osteotome sinus floor elevation[J]. J Periodontol, 2017,88(1):10-16. |
| [23] | Qin L, Lin SX, Guo ZZ , et al. Influences of schneiderian membrane conditions on the early outcomes of osteotome sinus floor elevation technique: a prospective cohort study in the healing period[J]. Clin Oral Implants Res, 2017,28(9):1074-1081. |
| [24] | Proussaefs P, Lozada J, Kim J , et al. Repair of the perforated sinus membrane with a resorbable collagen membrane: a human study[J]. Int J Oral Maxillofac Implants, 2004,19(3):413-420. |
| [1] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [2] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [3] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [4] | LI Yi,YU Hua-jie,QIU Li-xin. Clinical classification and treatment decision of implant fracture [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 126-133. |
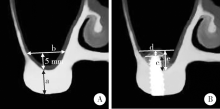
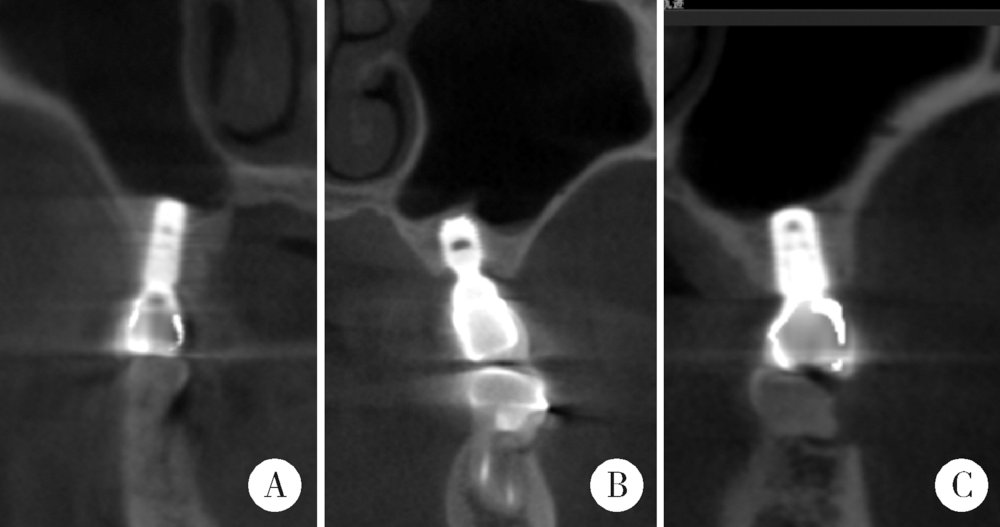
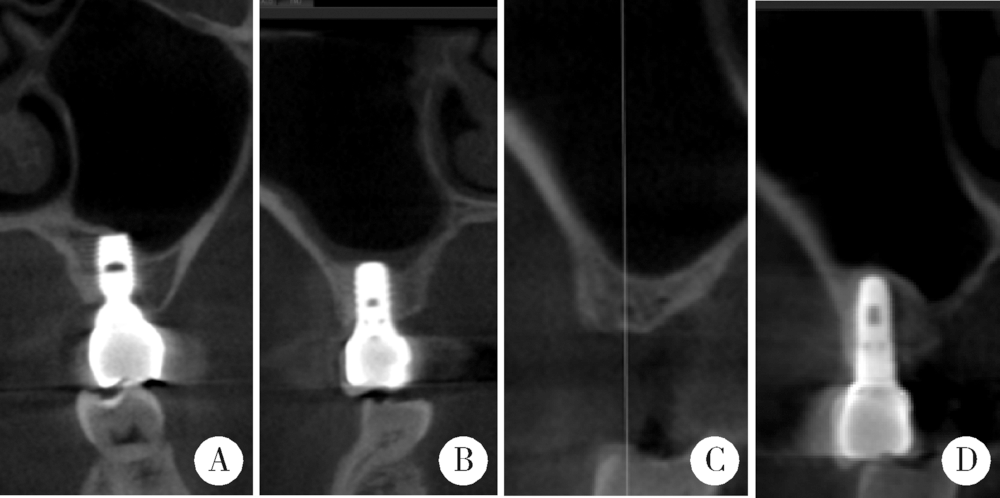
| [5] | LI Peng,PIAO Mu-zi,HU Hong-cheng,WANG Yong,ZHAO Yi-jiao,SHEN Xiao-jing. Radiography study on osteotome sinus floor elevation with placed implant simultaneously with no graft augmentation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 95-101. |
| [6] | Zhong ZHANG,Huan-xin MENG,Jie HAN,Li ZHANG,Dong SHI. Effect of vertical soft tissue thickness on clinical manifestation of peri-implant tissue in patients with periodontitis [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 332-338. |
| [7] | Chun-ping LIN,Song-he LU,Jun-xin ZHU,Hong-cheng HU,Zhao-guo YUE,Zhi-hui TANG. Influence of thread shapes of custom-made root-analogue implants on stress distribution of peri-implant bone: A three-dimensional finite element analysis [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1130-1137. |
| [8] | Xiao-qian LIU,Qiu-wen CHEN,Hai-lan FENG,Bing WANG,Jian QU,Zhen SUN,Mo-di HENG,Shao-xia PAN. Oral hygiene maintenance of locator attachments implant overdentures in edentulous population: A longitudinal study [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 136-144. |
| [9] | Zhi-yong△ ZHANG,Tian MENG,Quan CHEN,Wen-shu LIU,Yu-huan CHEN. Retrospective analysis of early dental implant failure [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1088-1091. |
| [10] | LIU Jing-yin, CHEN Fei, GE Yan-jun, WEI Ling, PAN Shao-xia, FENG Hai-lan. Influence of implants prepared by selective laser melting on early bone healing [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 117-122. |
| [11] | LIANG Nai-wen, SHI Lei,HUANG Ying,DENG Xu-liang. Role of different scale structures of titanium implant in the biological behaviors of human umbilical vein endothelial cells [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 43-048. |
| [12] | LI Bei-bei, LIN Ye, CUI Hong-yan, HAO Qiang, XU Jia-bin, DI Ping. Clinical evaluation of “All-on-Four” provisional prostheses reinforced with carbon fibers [J]. Journal of Peking University(Health Sciences), 2016, 48(1): 133-137. |
| [13] | CUI Hong-Yan, DI Ping, LI Jian-Hui, LIN Ye, LIU Rong-Rong. Application of spark erosion technology in manufacture of implant prosthesis [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 336-339. |
| [14] | HAN Jie, CHEN Zhi-Bin, LI Wei, MENG Huan-Xin. Determination of bone metabolic marker levels in perio-implant crevicular fluid and analysis of dental implants stability by resonance frequency in the early stage of healing [J]. Journal of Peking University(Health Sciences), 2015, 47(1): 37-41. |
| [15] | WU Min-Jie, ZHANG Xiang-Hao, ZOU Li-Dong, LIANG Feng. Clinical observation of the reliability of gingival contour by using temporary crown after loading 1 year [J]. Journal of Peking University(Health Sciences), 2014, 46(6): 954-957. |
|
||