Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (4): 762-770. doi: 10.19723/j.issn.1671-167X.2020.04.031
Previous Articles Next Articles
Evaluation of clinical efficacy of a kind of digital complete denture
Ling WEI1,Dong ZOU2,Hu CHEN1,Shao-xia PAN1,△( ),Yu-chun SUN1,△(
),Yu-chun SUN1,△( ),Yong-sheng ZHOU1
),Yong-sheng ZHOU1
- 1. Department of Prosthodontics, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Centre of Stomatology, China-Japan Friendship Hospital, Beijing 100029, China
CLC Number:
- R783.2
| [1] | Feine JS, Carlsson GE, Awad MA, et al. The McGill consensus statement on overdentures[J]. Int J Prosthodont, 2002,15(4):413-414. |
| [2] | Heydecke G, Locker D, Awad MA, et al. Oral and general health-related quality of life with conventional and implant dentures[J]. Community Dent Oral Epidemiol, 2003,31(3):161-168. |
| [3] | Awad MA, Lund JP, Dufresne E, et al. Comparing the efficacy of mandibular implant-retained overdentures and conventional dentures among middle-aged edentulous patients: satisfaction and functional assessment[J]. Int J Prosthodont, 2003,16(2):117-122. |
| [4] | Emami E, Heydecke G, Rompre PH, et al. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials[J]. Clin Oral Imp, 2009,20(6):533-544. |
| [5] |
Andreiotelli M, Att W, Strub JR. Prosthodontic complications with implant overdentures: a systematic literature review[J]. Int J Prosthodont, 2010,23(3):195-203.
pmid: 20552083 |
| [6] |
Bozini T, Petridis H, Garefis K, et al. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years[J]. Int J Oral Maxillofac Implants, 2011,26(2):304-318.
pmid: 21483883 |
| [7] | Bidra AS, Farrell K. Prospective cohort pilot study of 2-visit CAD/CAM monolithic complete dentures and implant-retained overdentures: clinical and patient-centered outcomes[J]. J Prosthet Dent, 2016,115(5):578-586. |
| [8] |
Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020[J]. J Prosthet Dent, 2002,87(1):5-8.
pmid: 11807476 |
| [9] |
Miyazaki T, Hotta Y, Kunii J, et al. A review of dental CAD/CAM: current status and future perspectives from 20 years of experience[J]. Dent Mater J, 2009,28(1):44-56.
pmid: 19280967 |
| [10] |
Wimmer T, Gallus K, Eichberger M, et al. Complete denture fabrication supported by CAD/CAM[J]. J Prosthet Dent, 2016,115(5):541-546.
pmid: 26774323 |
| [11] | Matsuda T, Goto T, Yagi K, Kashiwabara T, et al. Part-digitizing system of impression and interocclusal record for complete denture fabrication[J]. J Prosthodont, 2016,25(6):503-509. |
| [12] | Goodacre CJ, Garbacea A, Naylor WP, et al. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data[J]. Prosthet Dent, 2012,107(1):34-46. |
| [13] |
Inokoshi M, Kanazawa M, Minakuchi S. Evaluation of a complete denture trial method applying rapid prototyping[J]. Dent Mater J, 2012,31(1):40-46.
doi: 10.4012/dmj.2011-113 |
| [14] |
Zhang YD, Jiang JG, Liang T, et al. Kinematics modeling and experimentation of the multi-manipulator tooth-arrangement robot for full denture manufacturing[J]. J Med Syst, 2011,35(6):1421-1429.
pmid: 20703775 |
| [15] |
Kanazawa M, Inokoshi M, Minakuchi S, et al. Trial of a CAD/CAM system for fabricating complete dentures[J]. Dent Mater J, 2011,30(1):93-96.
doi: 10.4012/dmj.2010-112 |
| [16] |
Bidra AS, Taylor TD. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives[J]. J Prosthet Dent, 2013,109(6):361-366.
doi: 10.1016/S0022-3913(13)60318-2 pmid: 23763779 |
| [17] | 孙玉春, 吕培军, 王勇. 参数化定位全口义齿人工牙三维图形数据库的研究[J]. 口腔颌面修复学杂志, 2007,8(4):257-260. |
| [18] | 王勇, 吕培军, 赵占芳. 用于全口义齿的人工牙三维坐标系的建立[J]. 实用口腔医学杂志, 2005,21(5):653-655. |
| [19] | 孙玉春, 吕培军, 王勇. 计算机辅助设计与快速成形技术辅助制作全口义齿的探讨[J]. 中华口腔医学杂志, 2007,42(6):324-329. |
| [20] | 孙玉春, 吕培军, 王勇. 用于全口义齿计算机辅助设计的虚拟半可调牙合架[J]. 北京大学学报(医学版), 2008,40(1):92-96. |
| [21] | Sun YC, Lv PJ, Wang Y. Study on CAD & RP for removable complete denture[J]. Comput Meth Prog Bio, 2009,93(93):266-272. |
| [22] |
Chen H, Wang H, Lv PJ. Quantitative evaluation of tissue surface adaption of CAD-designed and 3D printed wax pattern of maxillary complete denture[J]. Biomed Res Int, 2015,2015:453968.
pmid: 26583108 |
| [23] |
Chen H, Yang X, Chen L, et al. Application of FDM three-dimensional printing technology in the digital manufacture of custom dentulous mandible trays[J]. Sci Rep, 2016,6:19207.
doi: 10.1038/srep19207 pmid: 26763620 |
| [24] | Yuan FS, Lv PJ, Wang PF, et al. Custom fabrication of try-inwax complete denture[J]. Rapid Prototyp J, 2016,22(3):539-543. |
| [25] |
Critchlow SB, Ellis JS. Prognostic indications for conventional complete denture therapy: a review of the literature[J]. J Dent, 2010,38(1):2-9.
doi: 10.1016/j.jdent.2009.08.004 pmid: 19695302 |
| [26] | 冯海兰, 徐军. 口腔修复学[M]. 2版. 北京: 北京大学医学出版社, 2015: 294. |
| [27] |
Reeve PE. The role of personality in the management of complete denture patients[J]. Br Dent J, 1984,156(10):356-362.
doi: 10.1038/sj.bdj.4805366 pmid: 6587876 |
| [28] |
Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile[J]. Community Dent Health, 1994,11(1):3-11.
pmid: 8193981 |
| [29] |
Awad MA, Lund JP, Shapiro SH, et al. Oral health status and treatment satisfaction with mandibular implant overdentures and conventional dentures: a randomized clinical trial in a senior population[J]. Int J Prosthodont, 2003,16(4):390-396.
pmid: 12956494 |
| [30] |
Bolender CL. The Cornell Medical Index as prognostic aid for complete denture patients[J]. J Prosthet Dent, 1969,22(1):20-29.
doi: 10.1016/0022-3913(69)90268-6 pmid: 5254404 |
| [31] |
Vervoorn JM, Duinkerke AS, Luteijn F, et al. Assessment of denture satisfaction[J]. Community Dent Oral Epidemiol, 1988,16(6):364-367.
doi: 10.1111/j.1600-0528.1988.tb00583.x pmid: 3060310 |
| [32] |
Bear ML. The use of the psychological measures in predicting patient satisfaction with complete dentures[J]. Int J Prosthodont, 1992,5(3):221-226.
pmid: 1524644 |
| [33] |
Kalk W, Baat C. Patients’ complaints and satisfaction 5 years after complete denture treatment[J]. Community Dent Oral Epidemiol, 1990,18(1):27-31.
pmid: 2404654 |
| [1] | Tuan-feng ZHOU,Xue YANG,Rui-jie WANG,Ming-xuan CHENG,Hua ZHANG,Jin-qi WEI. A clinical application study of digital manufacturing simple intraoral Gothic arch-tracing device in determining the centric relation of complete dentures [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 101-107. |
| [2] | Hao LUO,Fu-cong TIAN,Xiao-yan WANG. Surface roughness, gloss and sequential polishing times of various chairside computer aided design/manufacturing restorative materials [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 565-571. |
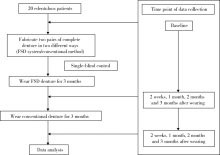
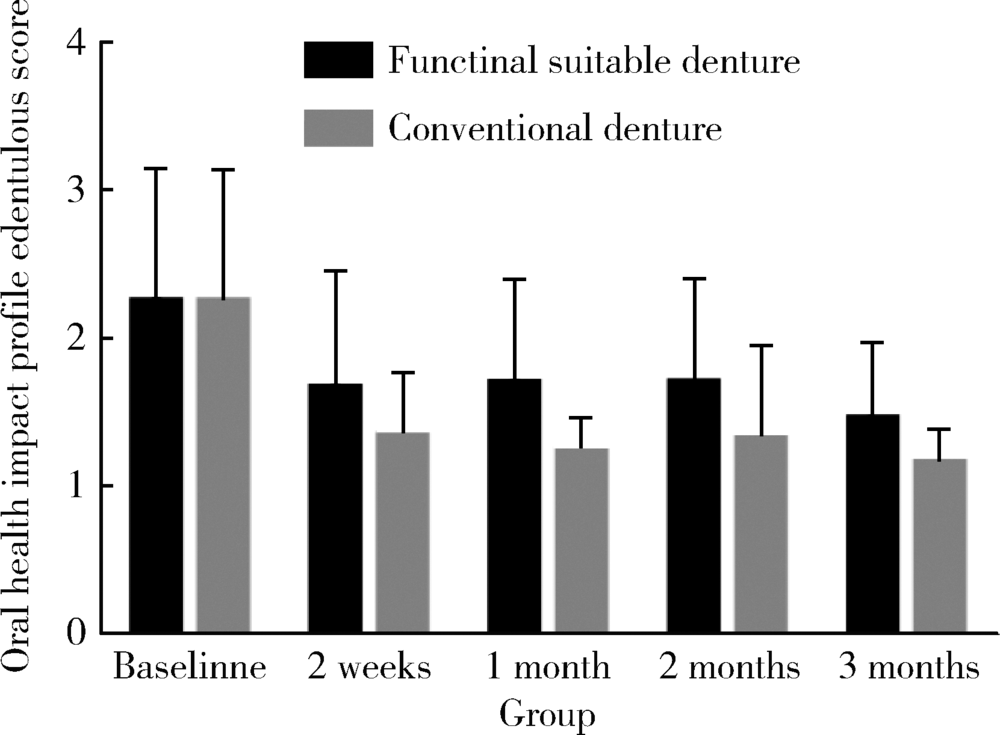
| [3] | Yu-chun SUN,Yong WANG,Ke-hui DENG,Hu CHEN,Wei-wei LI,Yi-jiao ZHAO,Shao-xia PAN,Hong-qiang YE,Yong-sheng ZHOU. Independent innovation research of functionally suitable denture digital system [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 390-394. |
|
||