Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (3): 453-459. doi: 10.19723/j.issn.1671-167X.2021.03.003
Previous Articles Next Articles
Genetic study of cardiovascular disease subtypes defined by International Classification of Diseases
GUO Zi-ning,LIANG Zhi-sheng,ZHOU Yi,ZHANG Na,HUANG JieΔ( )
)
- Department of Global Health, School of Public Health, Peking University 100191, China
CLC Number:
- R54
| [1] |
Nabel EG. Cardiovascular disease[J]. N Engl J Med, 2003,349(1):60-72.
doi: 10.1056/NEJMra035098 |
| [2] |
Collaborators GBDCOD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the global burden of disease study 2017[J]. Lancet, 2018,392(10159):1736-1788.
doi: 10.1016/S0140-6736(18)32203-7 |
| [3] |
Bowry AD, Lewey J, Dugani SB, et al. The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management[J]. Can J Cardiol, 2015,31(9):1151-1159.
doi: 10.1016/j.cjca.2015.06.028 |
| [4] | Mccarthy MI, Abecasis GR, Cardon LR, et al. Genome-wide association studies for complex traits: consensus, uncertainty and challenges[J]. Nat Rev Genet, 2008,9(5):356-369. |
| [5] |
Aragam KG, Natarajan P. Polygenic scores to assess atheroscle-rotic cardiovascular disease risk: clinical perspectives and basic implications[J]. Circ Res, 2020,126(9):1159-1177.
doi: 10.1161/CIRCRESAHA.120.315928 |
| [6] |
Hirsch JA, Nicola G, Mcginty G, et al. ICD-10: history and context[J]. Am J Neuroradiol, 2016,37(4):596-599.
doi: 10.3174/ajnr.A4696 |
| [7] |
Bycroft C, Freeman C, Petkova D, et al. The UK Biobank resource with deep phenotyping and genomic data[J]. Nature, 2018,562(7726):203-209.
doi: 10.1038/s41586-018-0579-z pmid: 30305743 |
| [8] |
Purcell S, Neale B, Todd-Brown K, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses[J]. Am J Hum Genet, 2007,81(3):559-575.
pmid: 17701901 |
| [9] |
Pruim RJ, Welch RP, Sanna S, et al. LocusZoom: regional visualization of genome-wide association scan results[J]. Bioinformatics, 2010,26(18):2336-2337.
doi: 10.1093/bioinformatics/btq419 |
| [10] |
Bulik-Sullivan B, Finucane HK, Anttila V, et al. An atlas of genetic correlations across human diseases and traits[J]. Nat Genet, 2015,47(11):1236-1241.
doi: 10.1038/ng.3406 |
| [11] |
Zhu Z, Zheng Z, Zhang F, et al. Causal associations between risk factors and common diseases inferred from GWAS summary data[J]. Nat Commun, 2018,9(1):224.
doi: 10.1038/s41467-017-02317-2 |
| [12] |
Perdu B, de Freitas F, Frints SG, et al. Osteopathia striata with cranial sclerosis owing to WTX gene defect[J]. J Bone Miner Res, 2010,25(1):82-90.
doi: 10.1359/jbmr.090707 |
| [13] |
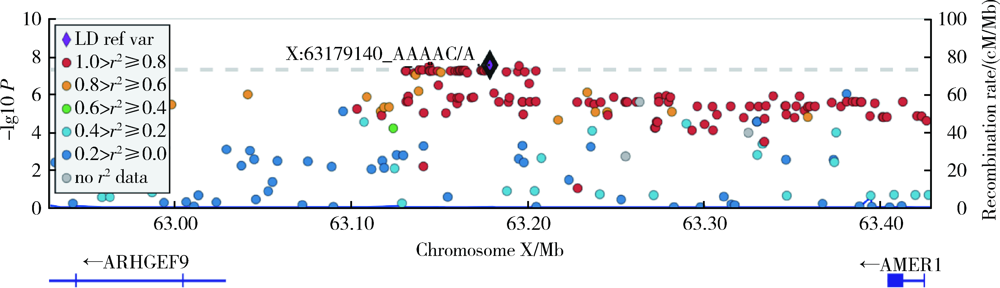
Sanz-Pamplona R, Lopez-Doriga A, Paré-Brunet L, et al. Exome sequencing reveals AMER1 as a frequently mutated gene in colorectal cancer[J]. Clin Cancer Res, 2015,21(20):4709-4718.
doi: 10.1158/1078-0432.CCR-15-0159 pmid: 26071483 |
| [14] |
Lloyd-Jones DM, Nam BH, D’agostino S, et al. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring[J]. JAMA, 2004,291(18):2204-2211.
pmid: 15138242 |
| [1] | Tianjing ZHOU,Qiuping LIU,Minglu ZHANG,Xiaofei LIU,Jiali KANG,Peng SHEN,Hongbo LIN,Xun TANG,Pei GAO. Comparison of initiation of antihypertensive therapy strategies for primary prevention of cardiovascular diseases in Chinese population: A decision-analytic Markov modelling study [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 441-447. |
| [2] | Ming-lu ZHANG,Qiu-ping LIU,Chao GONG,Jia-min WANG,Tian-jing ZHOU,Xiao-fei LIU,Peng SHEN,Hong-bo LIN,Xun TANG,Pei GAO. Comparison of aspirin treatment strategies for primary prevention of cardiovascular diseases: A decision-analytic Markov modelling study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 480-487. |
| [3] | Jia-min WANG,Qiu-ping LIU,Ming-lu ZHANG,Chao GONG,Shu-dan LIU,Wei-ye CHEN,Peng SHEN,Hong-bo LIN,Pei GAO,Xun TANG. Effectiveness of different screening strategies for type 2 diabete on preventing cardiovascular diseases in a community-based Chinese population using a decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 450-457. |
| [4] | Chao GONG,Qiu-ping LIU,Jia-min WANG,Xiao-fei LIU,Ming-lu ZHANG,Han YANG,Peng SHEN,Hong-bo LIN,Xun TANG,Pei GAO. Effectiveness of statin treatment strategies for primary prevention of cardiovascular diseases in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 443-449. |
| [5] | LIU Qiu-ping,CHEN Xi-jin,WANG Jia-min,LIU Xiao-fei,SI Ya-qin,LIANG Jing-yuan,SHEN Peng,LIN Hong-bo,TANG Xun,GAO Pei. Effectiveness of different screening strategies for cardiovascular diseases prevention in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 460-466. |
| [6] | Jia-li CHEN,Yue-bo JIN,Yi-fan WANG,Xiao-ying ZHANG,Jing LI,Hai-hong YAO,Jing HE,Chun LI. Clinical characteristics and risk factors of cardiovascular disease in patients with elderly-onset rheumatoid arthritis: A large cross-sectional clinical study [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1040-1047. |
| [7] | Meng-ying WANG,Wen-yong LI,Ren ZHOU,Si-yue WANG,Dong-jing LIU,Hong-chen ZHENG,Jing LI,Nan LI,Zhi-bo ZHOU,Hong-ping ZHU,Tao WU,Yong-hua HU. Evaluating the effect of WNT pathway genes considering interactions on the risk of non-syndromic oral clefts among Chinese populations [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 815-820. |
| [8] | YANG Chao, WANG Jin-wei, YANG Yao-zheng, BAI Kun-hao, GAO Bi-xia, ZHAO Ming-hui, ZHANG Lu-xia, WU Shou-ling, WANG Fang. Impact of anemia and chronic kidney disease on the risk of cardiovascular disease and all-cause mortality among diabetic patients [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 495-500. |
| [9] | SI Ya-qin, TANG Xun, ZHANG Du-dan, HE Liu, CAO Yang, WANG Jin-wei, LI Na, LIU Jian-jiang, GAO Pei, HU Yong-hua. Effectiveness of different screening strategies for primary prevention of cardiovascular diseases in a rural northern Chinese population [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 443-449. |
| [10] | TANG Xun1, ZHANG Du-dan, HE Liu, CAO Yang, WANG Jin-wei, LI Na, HUANG Shao-ping, DOU Hui-dong, GAO Pei, HU Yong-hua. Application of the China-PAR risk prediction model for atherosclerotic cardiovascular disease in a rural northern Chinese population [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 439-445. |
| [11] | GAO Ying, ZHU Cheng-gang, WU Na-qiong, GUO Yuan-lin, LIU Geng, DONG Qian, LI Jian-jun. Study on the reliability of CardioChek PA for measuring lipid profile [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 523-528. |
| [12] | YU Yang, SHENG Qin-Hui, ZHANG Bao-Wei, DING Wen-Hui. Left atrial size predicts adverse cardiac events in patients with non-obstruction hypertrophic cardiomyopathy [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 207-210. |
|
||