Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 850-856. doi: 10.19723/j.issn.1671-167X.2021.05.007
Previous Articles Next Articles
Management algorithm for septic arthritis after anterior cruciate ligament reconstruction
WANG Cheng1,MENG Ling-yu2,CHEN Na-yun1,LI Dai1,WANG Jian-quan1,AO Ying-fang1,△( )
)
- 1. Department of Sports Medicine, Peking University Third Hospital, Institute of Sports Medicine of Peking University, Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
2. Peking University School of Basic Medical Sciences, Beijing 100191, China
CLC Number:
- R687
| [1] |
Murawski CD, Wolf MR, Araki D, et al. Anatomic anterior cruciate ligament reconstruction: current concepts and future perspective [J]. Cartilage, 2013, 4(3):27S-37S.
doi: 10.1177/1947603513486557 |
| [2] |
Williams RJ, Laurencin CT, Warren RF, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction. Diagnosis and management [J]. Am J Sports Med, 1997, 25(2):261-267.
doi: 10.1177/036354659702500222 |
| [3] |
McAllister DR, Parker RD, Cooper AE, et al. Outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. Am J Sports Med, 1999, 27(5):562-570.
doi: 10.1177/03635465990270050301 |
| [4] |
Viola R, Marzano N, Vianello R. An unusual epidemic of Staphylococcus-negative infections involving anterior cruciate ligament reconstruction with salvage of the graft and function [J]. Arthroscopy, 2000, 16(2):173-177.
pmid: 10705329 |
| [5] |
Indelli PF, Dillingham M, Fanton G, et al. Septic arthritis in postoperative anterior cruciate ligament reconstruction [J]. Clin Orthop Relat Res, 2002, 398:182-188.
doi: 10.1097/00003086-200205000-00026 |
| [6] |
Schollin-Borg M, Michaёlsson K, Rahme H. Presentation, outcome, and cause of septic arthritis after anterior cruciate ligament reconstruction: a case control study [J]. Arthroscopy, 2003, 19(9):941-947.
pmid: 14608312 |
| [7] |
Burks RT, Friederichs MG, Fink B, et al. Treatment of post-operative anterior cruciate ligament infections with graft removal and early reimplantation [J]. Am J Sports Med, 2003, 31(3):414-418.
doi: 10.1177/03635465030310031501 |
| [8] |
Fong SY, Tan JL. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction [J]. Ann Acad Med Singap, 2004, 33(2):228-234.
pmid: 15098639 |
| [9] |
Musso AD, McCormack RG. Infection after ACL reconstruction: what happens when cultures are negative [J]. Clin J Sport Med, 2005, 15(5):381-384.
pmid: 16162999 |
| [10] |
Zalavras CG, Patzakis MJ, Tibone J, et al. Treatment of persistent infection after anterior cruciate ligament surgery [J]. Clin Orthop Relat Res, 2005, 439:52-55.
doi: 10.1097/01.blo.0000181499.49740.e5 |
| [11] |
Judd D, Bottoni C, Kim D, et al. Infections following arthroscopic anterior cruciate ligament reconstruction [J]. Arthroscopy, 2006, 22(4):375-384.
doi: 10.1016/j.arthro.2005.12.002 |
| [12] |
Binnet MS, Basarir K. Risk and outcome of infection after different arthroscopic anterior cruciate ligament reconstruction techniques [J]. Arthroscopy, 2007, 23(8):862-868.
doi: 10.1016/j.arthro.2007.02.008 |
| [13] |
Van Tongel A, Stuyck J, Bellemans J, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, management and outcome [J]. Am J Sports Med, 2007, 35(7):1059-1063.
doi: 10.1177/0363546507299443 |
| [14] |
Schulz AP, Götze S, Schmidt HG, et al. Septic arthritis of the knee after anterior cruciate ligament surgery: a stage-adapted treatment regimen [J]. Am J Sports Med, 2007, 35(7):1064-1069.
doi: 10.1177/0363546507299744 |
| [15] |
Katz LM, Battaglia TC, Patino P, et al. A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft [J]. Arthroscopy, 2008, 24(12):1330-1335.
doi: 10.1016/j.arthro.2008.07.015 |
| [16] |
Iorio R, Vadalà A, Di VI, et al. Tunnel enlargement after anterior cruciate ligament reconstruction in patients with post-operative septic arthritis [J]. Knee Surg Sports Traumatol Arthrosc, 2008, 16(10):921-927.
doi: 10.1007/s00167-008-0575-1 |
| [17] |
Wang C, Ao Y, Wang J, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause [J]. Arthroscopy, 2009, 25(3):243-249.
doi: 10.1016/j.arthro.2008.10.002 |
| [18] | Sajovic M, NiCAGL , Dernovš EMZ. Septic arthritis of the knee following anterior cruciate ligament reconstruction [J]. Orthop Rev (Pavia), 2009, 1(1):e3. |
| [19] |
Nag HL, Neogi DS, Nataraj AR, et al. Tubercular infection after arthroscopic anterior cruciate ligament reconstruction [J]. Arthroscopy, 2009, 25(2):131-136.
doi: 10.1016/j.arthro.2008.09.009 |
| [20] |
Monaco E, Maestri B, Labianca L, et al. Clinical and radiological outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. J Orthop Sci, 2010, 15(2):198-203.
doi: 10.1007/s00776-009-1447-3 |
| [21] |
Barker JU, Drakos MC, Maak TG, et al. Effect of graft selection on the incidence of postoperative infection in anterior cruciate ligament reconstruction [J]. Am J Sports Med, 2010, 38(2):281-286.
doi: 10.1177/0363546509346414 |
| [22] |
Benner RW, Shelbourne KD, Freeman H. Infections and patellar tendon ruptures after anterior cruciate ligament reconstruction: a comparison of ipsilateral and contralateral patellar tendon autografts [J]. Am J Sports Med, 2011, 39(3):519-525.
doi: 10.1177/0363546510388163 |
| [23] |
Sonnery-Cottet B, Archbold P, Zayni R, et al. Prevalence of septic arthritis after anterior cruciate ligament reconstruction among professional athletes [J]. Am J Sports Med, 2011, 39(11):2371-2376.
doi: 10.1177/0363546511417567 pmid: 21856928 |
| [24] |
Vertullo CJ, Quick M, Jones A, et al. A surgical technique using presoaked vancomycin hamstring grafts to decrease the risk of infection after anterior cruciate ligament reconstruction [J]. Arthroscopy, 2012, 28(3):337-342.
doi: 10.1016/j.arthro.2011.08.301 |
| [25] |
Schub DL, Schmitz LM, Sakamoto FA, et al. Long-term outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction [J]. Am J Sports Med, 2012, 40(12):2764-2770.
doi: 10.1177/0363546512461903 |
| [26] |
Torres-Claramunt R, Pelfort X, Erquicia J, et al. Knee joint infection after ACL reconstruction: prevalence, management and functional outcomes [J]. Knee Surg Sports Traumatol Arthrosc, 2013, 21(12):2844-2849.
doi: 10.1007/s00167-012-2264-3 |
| [27] |
RisticV , Maljanovic M, Harhaji V, et al. Infections after reconstructions of anterior cruciate ligament [J]. Med Pregl, 2014, 67(1/2):11-15.
doi: 10.2298/MPNS1402011R |
| [28] |
Abdel-Aziz A, Radwan YA, Rizk A. Multiple arthroscopic debridement and graft retention in septic knee arthritis after ACL reconstruction: a prospective case-control study [J]. Int Orthop, 2014, 38(1):73-82.
doi: 10.1007/s00264-013-2123-y pmid: 24100920 |
| [29] |
Boström WH, Mikkelsen C, Forssblad M, et al. Postoperative septic arthritis after anterior cruciate ligament reconstruction: does it affect the outcome? a retrospective controlled study [J]. Arthroscopy, 2014, 30(9):1100-1109.
doi: 10.1016/j.arthro.2014.03.019 |
| [30] |
Calvo R, Figueroa D, Anastasiadis Z, et al. Septic arthritis in ACL reconstruction surgery with hamstring autografts. eleven years of experience [J]. Knee, 2014, 21(3):717-720.
doi: 10.1016/j.knee.2014.01.007 |
| [31] |
Schuster P, Schulz M, Immendoerfer M, et al. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: evaluation of an arthroscopic graft-retaining treatment protocol [J]. Am J Sports Med, 2015, 43(12):3005-3012.
doi: 10.1177/0363546515603054 pmid: 26403209 |
| [32] |
Pérez-Prieto D, Trampuz A, Torres-Claramunt R, et al. Infections after anterior cruciate ligament reconstruction: which antibiotic after arthroscopic debridement? [J]. J Knee Surg, 2017, 30(4):309-313.
doi: 10.1055/s-0036-1584559 pmid: 27367205 |
| [33] |
Hantes ME, Raoulis VA, Doxariotis N, et al. Management of septic arthritis after arthroscopic anterior cruciate ligament reconstruction using a standard surgical protocol [J]. Knee, 2017, 24(3):588-593.
doi: 10.1016/j.knee.2017.02.007 |
| [34] |
Torres-Claramunt R, Gelber P, Pelfort X, et al. Managing septic arthritis after knee ligament reconstruction [J]. Int Orthop, 2016, 40(3):607-614.
doi: 10.1007/s00264-015-2884-6 pmid: 26239533 |
| [35] |
Wang C, Lee YH, Siebold R. Recommendations for the management of septic arthritis after ACL reconstruction [J]. Knee Surg Sports Traumatol Arthrosc, 2014, 22(9):2136-2144.
doi: 10.1007/s00167-013-2648-z |
| [36] |
Muscolo DL, Carbo L, Aponte-Tinao LA, et al. Massive bone loss from fungal infection after anterior cruciate ligament arthroscopic reconstruction [J]. Clin Orthop Relat Res, 2009, 467(9):2420-2425.
doi: 10.1007/s11999-009-0714-0 |
| [37] |
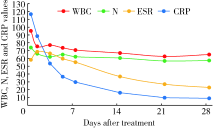
Wang C, Ao Y, Fan X, et al. C-reactive protein and erythrocyte sedimentation rate changes after arthroscopic anterior cruciate ligament reconstruction: guideline to diagnose and monitor postoperative infection [J]. Arthroscopy, 2014, 30(9):1110-1115.
doi: 10.1016/j.arthro.2014.03.025 |
| [38] |
Paci JM, Schweizer SK, Wilbur DM, et al. Results of laboratory evaluation of acute knee effusion after anterior cruciate ligament reconstruction: what is found in patients with a noninfected, painful postoperative knee [J]. Am J Sports Med, 2010, 38(11):2267-2272.
doi: 10.1177/0363546510374573 |
| [1] | Shuang REN, Huijuan SHI, Zixuan LIANG, Si ZHANG, Xiaoqing HU, Hongshi HUANG, Yingfang AO. Biomechanics during cutting movement in individuals after anterior cruciate ligament reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 868-873. |
| [2] | Li WAN, Zhoucang ZHANG, Jiaxiang DING, Mei WANG. Venous air embolism following removal of central venous catheters: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 938-941. |
| [3] | Jiangjing WANG,Shunyi WEI,Yingfang AO,Yuping YANG. Comparison of the early analgesic efficacy of three different drugs after anterior cruciate ligament reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 293-298. |
| [4] | Jiayun DONG,Xuefen LI,Ruifang LU,Wenjie HU,Huanxin MENG. Histopathological characteristics of peri-implant soft tissue in reconstructed jaws with vascularized bone flaps [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 25-31. |
| [5] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [6] | Xin-ling ZHANG,Zhi-yu LIN,Yu-jie CHEN,Wen-fang DONG,Xin YANG. Plastic and reconstruction surgery for non-healing wound after posterior spinal surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 910-914. |
| [7] | Hai-xia XING,Lin WANG,Di QIAO,Chang LIU,Jie PAN. Clinical features of oral management to oral complications of Sjögren's syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 929-933. |
| [8] | Su-huan XU,Bei-bei WANG,Qiu-ying PANG,Li-jun ZHONG,Yan-ming DING,Yan-bo HUANG,Xin-yan CHE. Effect of equal temperature bladder irrigation in patients with transurethral resection of prostate: A meta-analysis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 676-683. |
| [9] | Hui LI,Yang-xu GAO,Shu-lei WANG,Hong-xin YAO. Surgical complications of totally implantable venous access port in children with malignant tumors [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1167-1171. |
| [10] | Bo YU,Yang-yu ZHAO,Zhe ZHANG,Yong-qing WANG. Infective endocarditis in pregnancy: A case report [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 578-580. |
| [11] | WU Jun-hui,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,QIN Xue-ying,WANG Meng-ying,WANG Xiao-wen,WANG Jia-ting,HU Yong-hua. Incidence and risk factors of ischemic stroke in patients with type 2 diabetes among urban workers in Beijing, China [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 249-254. |
| [12] | CAI Tian-yi,ZHANG Wen-bo,YU Yao,WANG Yang,MAO Chi,GUO Chuan-bin,YU Guang-yan,PENG Xin. Clinical analysis of selective tracheostomy necessary for patients undergoing head and neck surgery with free flap reconstruction [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 363-368. |
| [13] | LI Wei-hao,LI Wei,ZHANG Xue-min,LI Qing-le,JIAO Yang,ZHANG Tao,JIANG Jing-jun,ZHANG Xiao-ming. Comparison of the outcomes between open and hybrid approaches in the treatment of thoracoabdominal aortic aneurysms repair [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 177-181. |
| [14] | Yan-fang JIANG,Jian WANG,Yong-jian WANG,Jia LIU,Yin PEI,Xiao-peng LIU,Ying-fang AO,Yong MA. Mid-to-long term clinical outcomes and predictors after anterior cruciate ligament revision [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 857-863. |
| [15] | Shuang REN,Hui-juan SHI,Jia-hao ZHANG,Zhen-long LIU,Jia-yi SHAO,Jing-xian ZHU,Xiao-qing HU,Hong-shi HUANG,Ying-fang AO. Finite element analysis of the graft stresses after anterior cruciate ligament reconstruction [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 865-870. |
|
||