Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (5): 991-999. doi: 10.19723/j.issn.1671-167X.2022.05.028
Previous Articles Next Articles
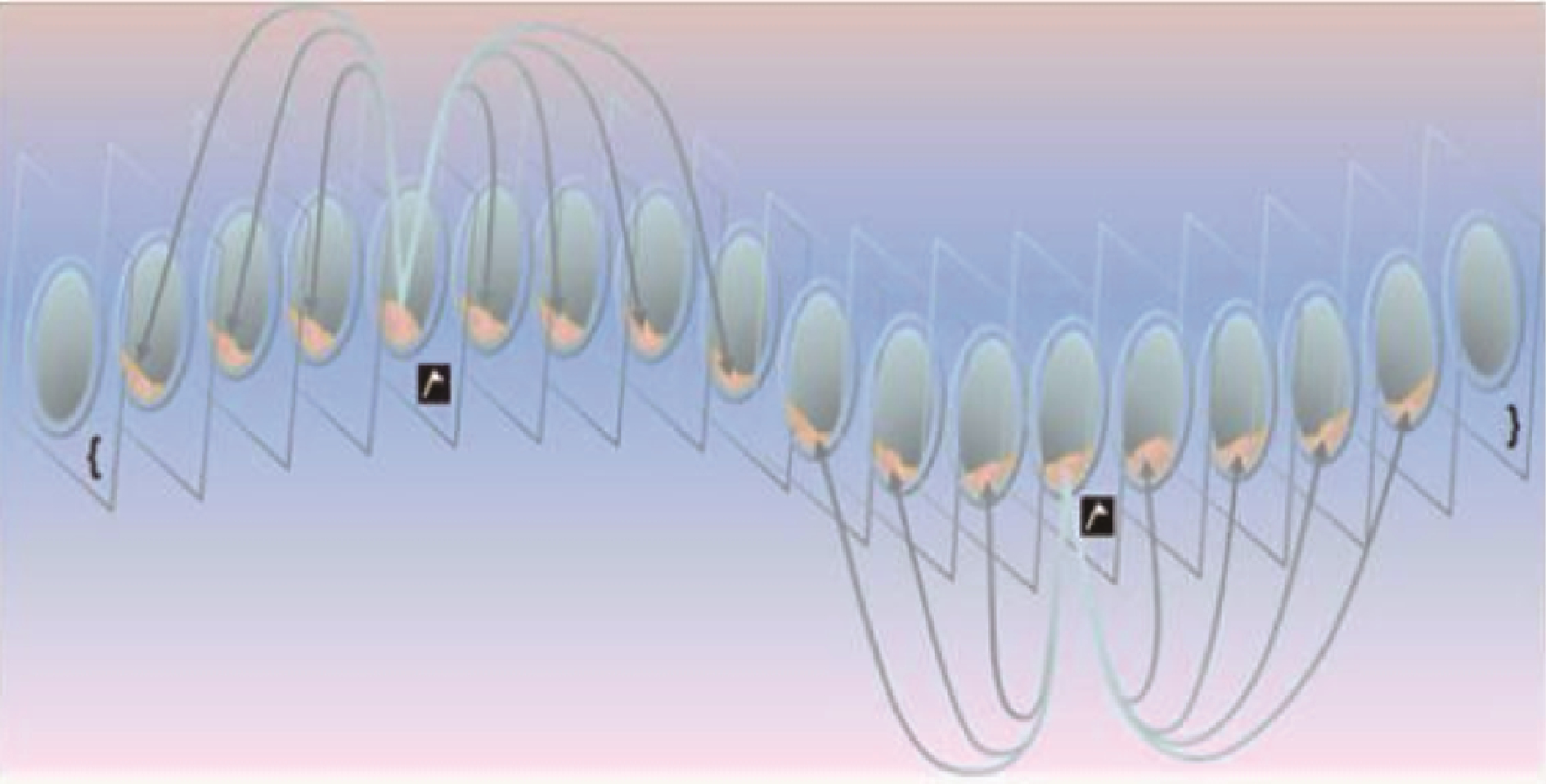
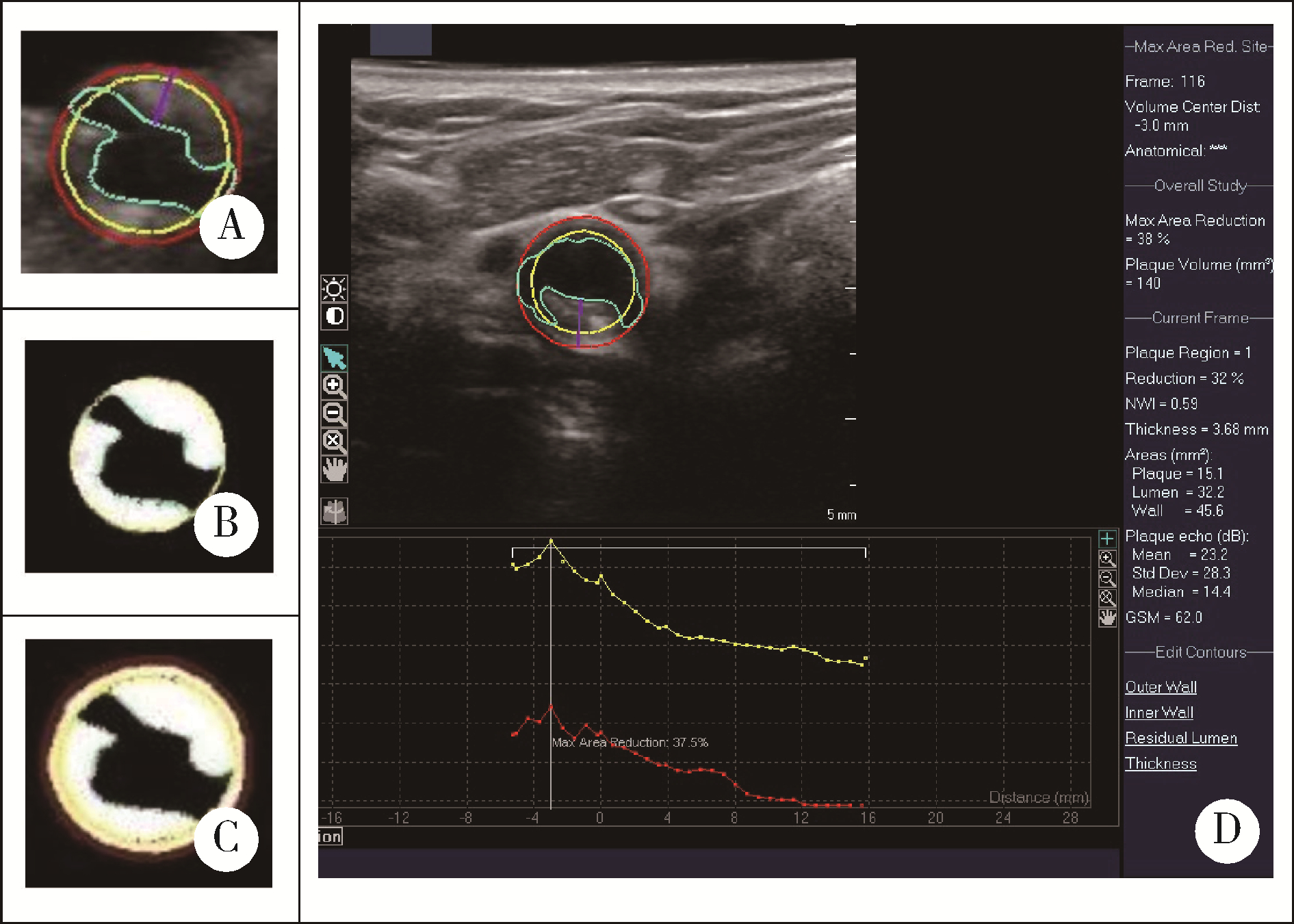
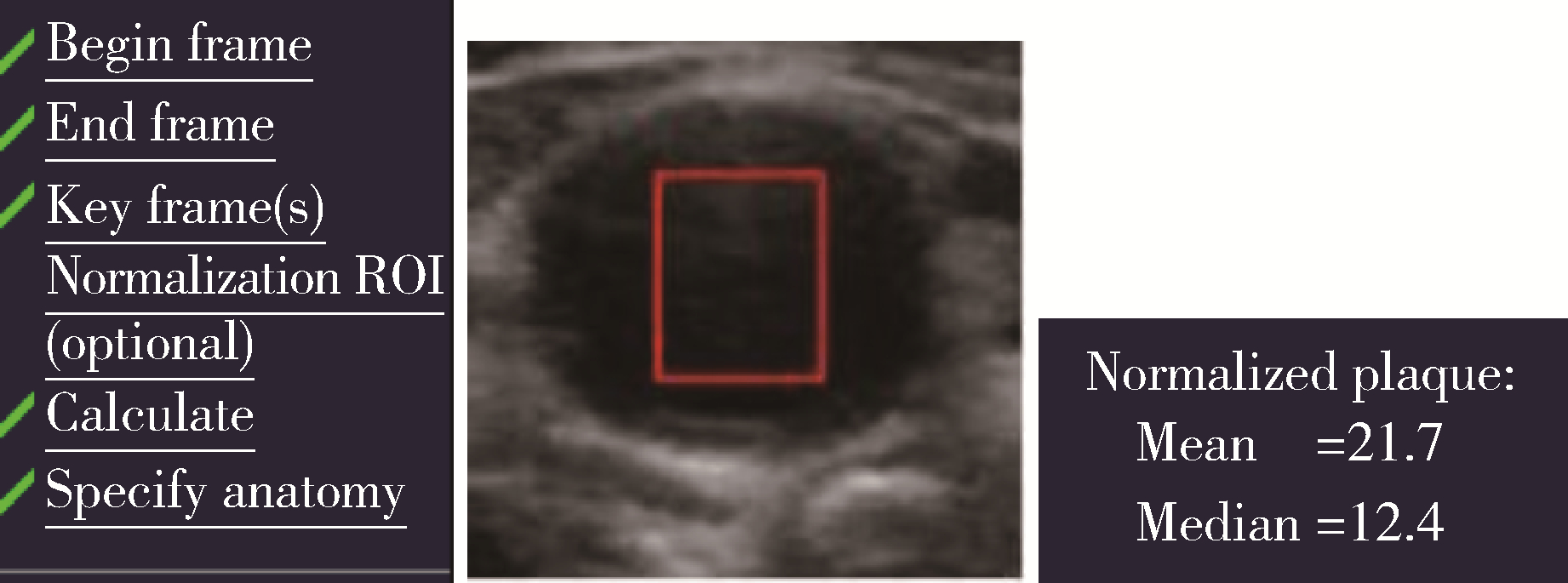
Evaluation of carotid atherosclerotic plaques by vascular plaque quantification (VPQ) technology of three-dimensional ultrasonography
Hai-ying XING1,2,Yu-hui CHEN3,Ke XU1,2,Dian-dian HUANG1,2,Qing PENG1,2,Ran LIU1,2,Wei SUN1,2,Yi-ning HUANG1,2,*( )
)
- 1. Department of Neurology, Peking University First Hospital, Beijing 100034, China
2. Department of Neurology, Beijing Key Laboratory of Neurovascular Disease Discovery, Beijing, China
3. Department of Neurology, Beijing Hospital, Beijing 100730, China
CLC Number:
- R543.4
| 1 |
Lal BK , Hobson RW , Pappas PJ , et al. Pixel distribution analysis of B-mode ultrasound scan images predicts histologic features of atherosclerotic carotid plaques[J]. J Vasc Surg, 2002, 35 (6): 1210- 1217.
doi: 10.1067/mva.2002.122888 |
| 2 |
Herr JE , Hetu MF , Li TY , et al. Presence of calcium-like tissue composition in carotid plaque is indicative of significant coronary artery disease in high-risk patients[J]. J Am Soc Echocardiogr, 2019, 32 (5): 633- 642.
doi: 10.1016/j.echo.2019.01.001 |
| 3 |
Mujaj B , Bos D , Selwaness M , et al. Statin use is associated with carotid plaque composition: The Rotterdam study[J]. Int J Cardiol, 2018, 260, 213- 218.
doi: 10.1016/j.ijcard.2018.02.111 |
| 4 |
Vergallo R , Crea F . Atherosclerotic plaque healing[J]. N Engl J Med, 2020, 383 (9): 846- 857.
doi: 10.1056/NEJMra2000317 |
| 5 |
Touboul PJ , Hennerici MG , Meairs S , et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011[J]. Cerebrovasc Dis, 2012, 34 (4): 290- 296.
doi: 10.1159/000343145 |
| 6 |
中国成人血脂异常防治指南修订联合委员会. 中国成人血脂异常防治指南(2016年修订版)[J]. 中华心血管病杂志, 2016, 44 (10): 833- 853.
doi: 10.3760/cma.j.issn.0253-3758.2016.10.005 |
| 7 | Geroulakos G , Ramaswami G , Nicolaides A , et al. Characterization of symptomatic and asymptomatic carotid plaques using high-resolution real-time ultrasonography[J]. Br J Surg, 1993, 80 (10): 1274- 1277. |
| 8 |
Johri AM , Herr JE , Li TY , et al. Novel ultrasound methods to investigate carotid artery plaque vulnerability[J]. J Am Soc Echocardiogr, 2017, 30 (2): 139- 148.
doi: 10.1016/j.echo.2016.11.003 |
| 9 |
el-Barghouty N , Geroulakos G , Nicolaides A , et al. Computer-assisted carotid plaque characterisation[J]. Eur J Vasc Endovasc Surg, 1995, 9 (4): 389- 393.
doi: 10.1016/S1078-5884(05)80005-X |
| 10 |
Spanos K , Tzorbatzoglou I , Lazari P , et al. Carotid artery plaque echomorphology and its association with histopathologic characteristics[J]. J Vasc Surg, 2018, 68 (6): 1772- 1780.
doi: 10.1016/j.jvs.2018.01.068 |
| 11 |
Mathiesen EB , Bonaa KH , Joakimsen O . Echolucent plaques are associated with high risk of ischemic cerebrovascular events in carotid stenosis: The tromso study[J]. Circulation, 2001, 103 (17): 2171- 2175.
doi: 10.1161/01.CIR.103.17.2171 |
| 12 |
Hashimoto H , Tagaya M , Niki H , et al. Computer-assisted analysis of heterogeneity on B-mode imaging predicts instability of asymptomatic carotid plaque[J]. Cerebrovasc Dis, 2009, 28 (4): 357- 364.
doi: 10.1159/000229554 |
| 13 |
Huibers A , de Borst GJ , Bulbulia R , et al. Plaque echolucency and the risk of ischaemic stroke in patients with asymptomatic carotid stenosis within the first asymptomatic carotid surgery trial (ACST-1)[J]. Eur J Vasc Endovasc Surg, 2016, 51 (5): 616- 621.
doi: 10.1016/j.ejvs.2015.11.013 |
| 14 |
Zhang M , Zhao Q , Gao Y , et al. Prediction for rupture risk of carotid artery plaques: A comparative study of 3D-GSM and CAS system[J]. Eur J Radiol, 2016, 85 (9): 1659- 1665.
doi: 10.1016/j.ejrad.2016.05.013 |
| 15 |
王秀玲, 张敏郁, 丁桂春, 等. 三维超声灰阶中位数定量评价颈动脉斑块的易损性[J]. 中华医学超声杂志: 电子版, 2017, 14 (1): 23- 28.
doi: 10.3877/cma.j.issn.1672-6448.2017.01.008 |
| 16 |
Urbak L , Sandholt BV , Graebe M , et al. Patients with unstable atherosclerosis have more echolucent carotid plaques compared with stable atherosclerotic patients: A 3-D ultrasound study[J]. Ultrasound Med Biol, 2020, 46 (9): 2164- 2172.
doi: 10.1016/j.ultrasmedbio.2020.04.002 |
| 17 |
Nicolaides AN , Kakkos SK , Kyriacou E , et al. Asymptomatic internal carotid artery stenosis and cerebrovascular risk stratification[J]. J Vasc Surg, 2010, 52 (6): 1486- 1496.
doi: 10.1016/j.jvs.2010.07.021 |
| 18 |
Ruiz-Ares G , Fuentes B , Martinez-Sanchez P , et al. A prediction model for unstable carotid atheromatous plaque in acute ischemic stroke patients: Proposal and internal validation[J]. Ultrasound Med Biol, 2014, 40 (9): 1958- 1965.
doi: 10.1016/j.ultrasmedbio.2014.04.015 |
| 19 |
Biasi GM , Froio A , Diethrich EB , et al. Carotid plaque echolucency increases the risk of stroke in carotid stenting: The imaging in carotid angioplasty and risk of stroke (ICAROS) study[J]. Circulation, 2004, 110 (6): 756- 762.
doi: 10.1161/01.CIR.0000138103.91187.E3 |
| 20 |
Ariyoshi K , Okuya S , Kunitsugu I , et al. Ultrasound analysis of gray-scale median value of carotid plaques is a useful reference index for cerebro-cardiovascular events in patients with type 2 diabetes[J]. J Diabetes Investig, 2015, 6 (1): 91- 97.
doi: 10.1111/jdi.12242 |
| 21 |
国家卫生健康委员会脑卒中防治专家委员会血管超声专业委员会, 中国超声医学工程学会浅表器官及外周血管超声专业委员会, 中国超声医学工程学会颅脑及颈部血管超声专业委员会, 中国超声医学工程学会颅脑及颈部血管超声专业委员会. 头颈部血管超声若干问题的专家共识(颈动脉部分)[J]. 中国脑血管病杂志, 2020, 17 (6): 346- 352.
doi: 10.3969/j.issn.1672-5921.2020.06.013 |
| 22 |
Kadoglou NP , Gerasimidis T , Moumtzouoglou A , et al. Intensive lipid-lowering therapy ameliorates novel calcification markers and GSM score in patients with carotid stenosis[J]. Eur J Vasc Endovasc Surg, 2008, 35 (6): 661- 668.
doi: 10.1016/j.ejvs.2007.12.011 |
| 23 |
Yamaguchi M , Sasaki M , Ohba H , et al. Quantitative assessment of changes in carotid plaques during cilostazol administration using three-dimensional ultrasonography and non-gated magnetic resonance plaque imaging[J]. Neuroradiology, 2012, 54 (9): 939- 945.
doi: 10.1007/s00234-012-1011-2 |
| [1] | Chao GONG,Qiu-ping LIU,Jia-min WANG,Xiao-fei LIU,Ming-lu ZHANG,Han YANG,Peng SHEN,Hong-bo LIN,Xun TANG,Pei GAO. Effectiveness of statin treatment strategies for primary prevention of cardiovascular diseases in a community-based Chinese population: A decision-analytic Markov model [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 443-449. |
| [2] | LIU Huan, WANG Hong-yu, LIU Jin-bo, ZHAO Hong-wei, ZHOU Ying-yan, LI Li-hong. Relationship between large artery elasticity function and coronary heart disease, lower extremity arterial disease in patients with carotid plaque [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1027-1033. |
| [3] | JIA Li-jing, YI Liang, YANG Zhi-xu, WANG Shu-peng, LI Gang, ZHU Xi. Preventive effects of ulinastatin on acute respiratory distress syndrome [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 672-679. |
| [4] | ZHANG Jing, REN Jing-yi, CHEN Hong, HAN Guan-ping. Statins decreases expression of five inflammation-associated microRNAs in the plasma of patients with unstable angina [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 761-768. |
| [5] | 欧Meng-恩 , ZHANG Xiao, LIU Yun-Song, GE Yan-Jun, ZHOU Yong-Sheng. Ectopic osteogenesis of stromal cell-derived factor 1 combined with simvastatin loaded collagen scaffold in vivo [J]. Journal of Peking University(Health Sciences), 2015, 47(1): 47-51. |
| [6] | XU Lu, WANG Chao, SHEN Wen-Wen, QI Rong. Effects of simvastatin nano-liposomes on osteogenic differentiation of bone marrow stromal cells [J]. Journal of Peking University(Health Sciences), 2014, 46(6): 883-888. |
| [7] | GUAN Jing-Lin, JIANG Wen- , WANG Huai-Yu, ZENG Hui, ZHANG Su-Min, WANG Guang, MAO Jie-Ming. Multiple effect of simvastatin on vascular endothelium of hypercholesterolemia patients [J]. Journal of Peking University(Health Sciences), 2014, 46(5): 703-706. |
| [8] | XIA Jing-Gang, QU Yang, Hu-Shao-Dong, XU Ji, YIN Chun-Lin, XU Dong. Cardioprotective effect and mechanism of intensive lipid modulation on patients with coronary artery disease undergoing noncardiac surgery [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 601-605. |
|
||