Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1190-1195. doi: 10.19723/j.issn.1671-167X.2022.06.022
Previous Articles Next Articles
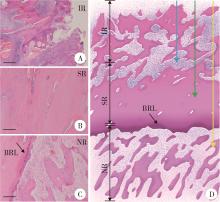
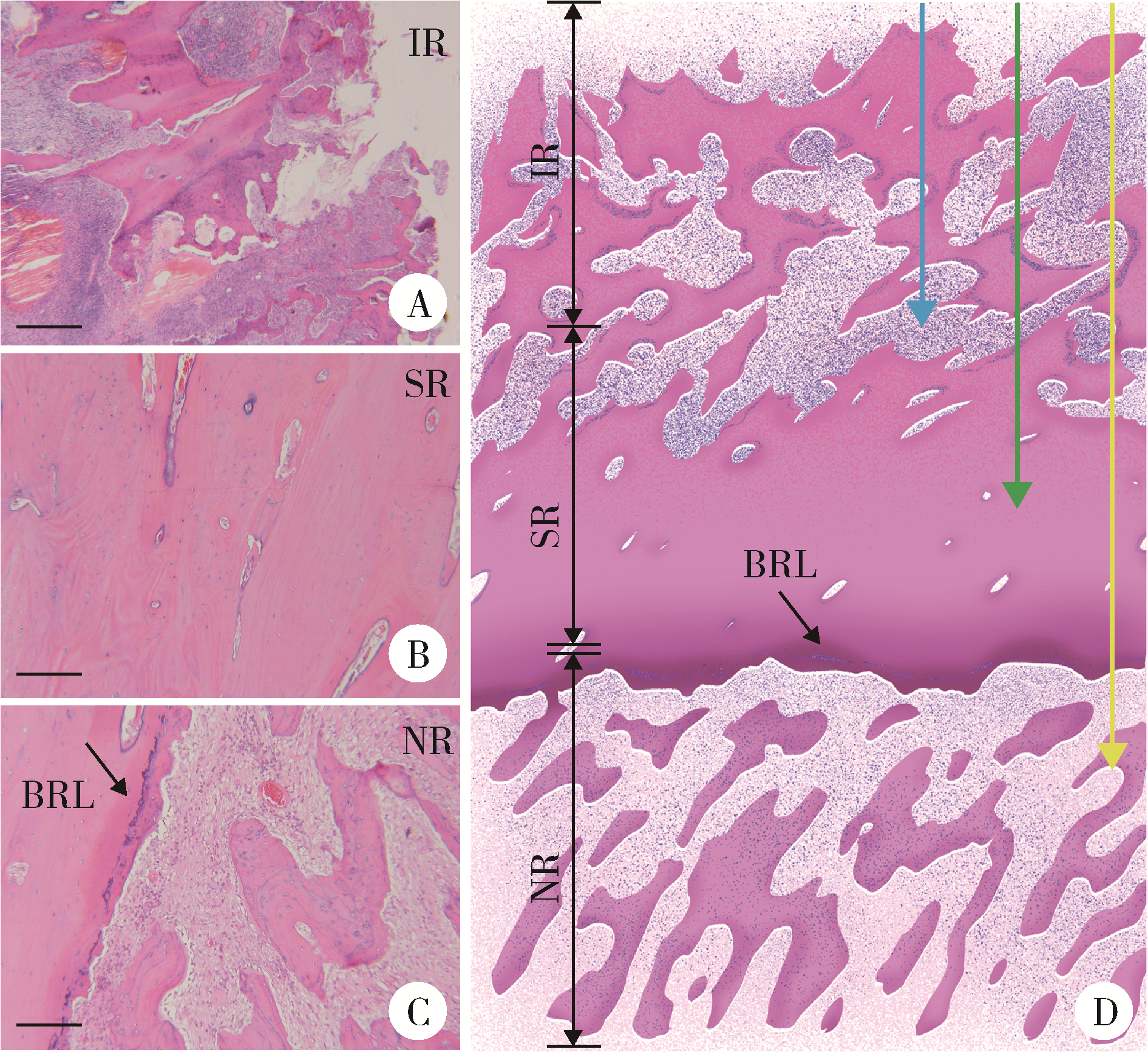
Analysis of pathological characteristics of medication-related osteonecrosis of the jaw and discussion of clinical treatment strategies based on the pathological analysis results
Yu-xing GUO1,Jian-yun ZHANG2,Dian-can WANG1,Chuan-bin GUO1,*( )
)
- 1. Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
2. Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R782.4
| 1 | Sacco R , Sacco N , Hamid U , et al. Microsurgical reconstruction of the jaws using vascularised free flap technique in patients with medication-related osteonecrosis: A systematic review[J]. Biomed Res Int, 2018, 2018, 9858921. |
| 2 |
Rupel K , Ottaviani G , Gobbo M , et al. A systematic review of therapeutical approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ)[J]. Oral Oncol, 2014, 50 (11): 1049- 1057.
doi: 10.1016/j.oraloncology.2014.08.016 |
| 3 |
郭玉兴, 王佃灿, 王洋, 等. 二膦酸盐药物治疗乳腺癌骨转移发生颌骨坏死的临床特点[J]. 北京大学学报(医学版), 2016, 48 (1): 80- 83.
doi: 10.3969/j.issn.1671-167X.2016.01.014 |
| 4 |
Hayashida S , Soutome S , Yanamoto S , et al. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: A multicenter retrospective study with propensity score matching analysis[J]. J Bone Miner Res, 2017, 32 (10): 2022- 2029.
doi: 10.1002/jbmr.3191 |
| 5 |
Ruggiero SL , Dodson TB , Fantasia J , et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw: 2014 update[J]. J Oral Maxillofac Surg, 2014, 72 (10): 1938- 1956.
doi: 10.1016/j.joms.2014.04.031 |
| 6 |
Basi DL , Hughes PJ , Thumbigere-Math V , et al. Matrix metalloproteinase-9 expression in alveolar extraction sockets of Zoledronic acid-treated rats[J]. J Oral Maxillofac Surg, 2011, 69 (11): 2698- 2707.
doi: 10.1016/j.joms.2011.02.065 |
| 7 |
Yamashita J , Koi K , Yang DY , et al. Effect of zoledronate on oral wound healing in rats[J]. Clin Cancer Res, 2011, 17 (6): 1405- 1414.
doi: 10.1158/1078-0432.CCR-10-1614 |
| 8 |
Marx RE . Pamidronate (aredia) and zoledronate (zometa) induced avascular necrosis of the jaws: A growing epidemic[J]. J Oral Maxillofac Surg, 2003, 61 (9): 1115- 1117.
doi: 10.1016/S0278-2391(03)00720-1 |
| 9 |
Ruggiero SL , Mehrotra B , Rosenberg TJ , et al. Osteonecrosis of the jaws associated with the use of bisphosphonates: A review of 63 cases[J]. J Oral Maxillofac Surg, 2004, 62 (5): 527- 534.
doi: 10.1016/j.joms.2004.02.004 |
| 10 |
Lin JT , Lane JM . Bisphosphonates[J]. J Am Acad Orthop Surg, 2003, 11 (1): 1- 4.
doi: 10.5435/00124635-200301000-00001 |
| 11 | Di Fede O , Panzarella V , Mauceri R , et al. The dental management of patients at risk of medication-related osteonecrosis of the jaw: new paradigm of primary prevention[J]. Biomed Res Int, 2018, 2018, 2684924. |
| 12 |
Shintani T , Hayashido Y , Mukasa H , et al. Comparison of the prognosis of bisphosphonate-related osteonecrosis of the jaw caused by oral and intravenous bisphosphonates[J]. Int J Oral Maxillofac Surg, 2015, 44 (7): 840- 844.
doi: 10.1016/j.ijom.2015.03.013 |
| 13 |
Nicolatou-Galitis O , Papadopoulou E , Vardas E , et al. Alveolar bone histological necrosis observed prior to extractions in patients, who received bone-targeting agents[J]. Oral Dis, 2020, 26 (5): 955- 966.
doi: 10.1111/odi.13294 |
| 14 |
Guo Y , Guo C . Enhancement of bone perfusion through cortical perforations to improve healing of medication-related osteonecrosis of the jaw: A retrospective study[J]. Int J Oral Maxillofac Surg, 2021, 50 (6): 740- 745.
doi: 10.1016/j.ijom.2020.07.036 |
| 15 |
郭玉兴, 王佃灿, 刘筱菁, 等. 翻瓣联合骨管技术拔牙方案在药物相关性颌骨坏死潜在风险患者中的应用初探[J]. 中华口腔医学杂志, 2021, 56 (5): 452- 457.
doi: 10.3760/cma.j.cn112144-20210104-00003 |
| [1] | Ying ZHOU,Ning ZHAO,Hongyuan HUANG,Qingxiang LI,Chuanbin GUO,Yuxing GUO. Application of double-layer soft tissue suture closure technique in the surgical treatment of patients with mandible medication-related osteonecrosis of the jaw of early and medium stages [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 51-56. |
| [2] | DING Ting-ting,ZENG Chu-xiong,HU Li-na,YU Ming-hua. Establishment of a prediction model for colorectal cancer immune cell infiltration based on the cancer genome atlas (TCGA) database [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 203-208. |
| [3] | WANG Ying-chun,HUANG Yong-hui,CHANG Hong,YAO Wei,YAN Xiu-e,LI Ke,ZHANG Yao-peng,ZHENG Wei. Characteristics of benign and malignant lesions of ampullary polyps and the accuracy of forceps biopsy [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 204-209. |
| [4] | Xiao-peng ZHANG,Zi-xiong HUANG,Lu-ping YU,Xiao-wei ZHANG,Qing LI,Shi-jun LIU,Tao XU. Clinical and pathological analysis of small renal cell carcinoma [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 623-627. |
|
||