Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (2): 303-308. doi: 10.19723/j.issn.1671-167X.2025.02.013
Previous Articles Next Articles
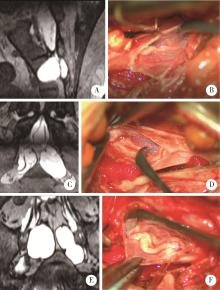
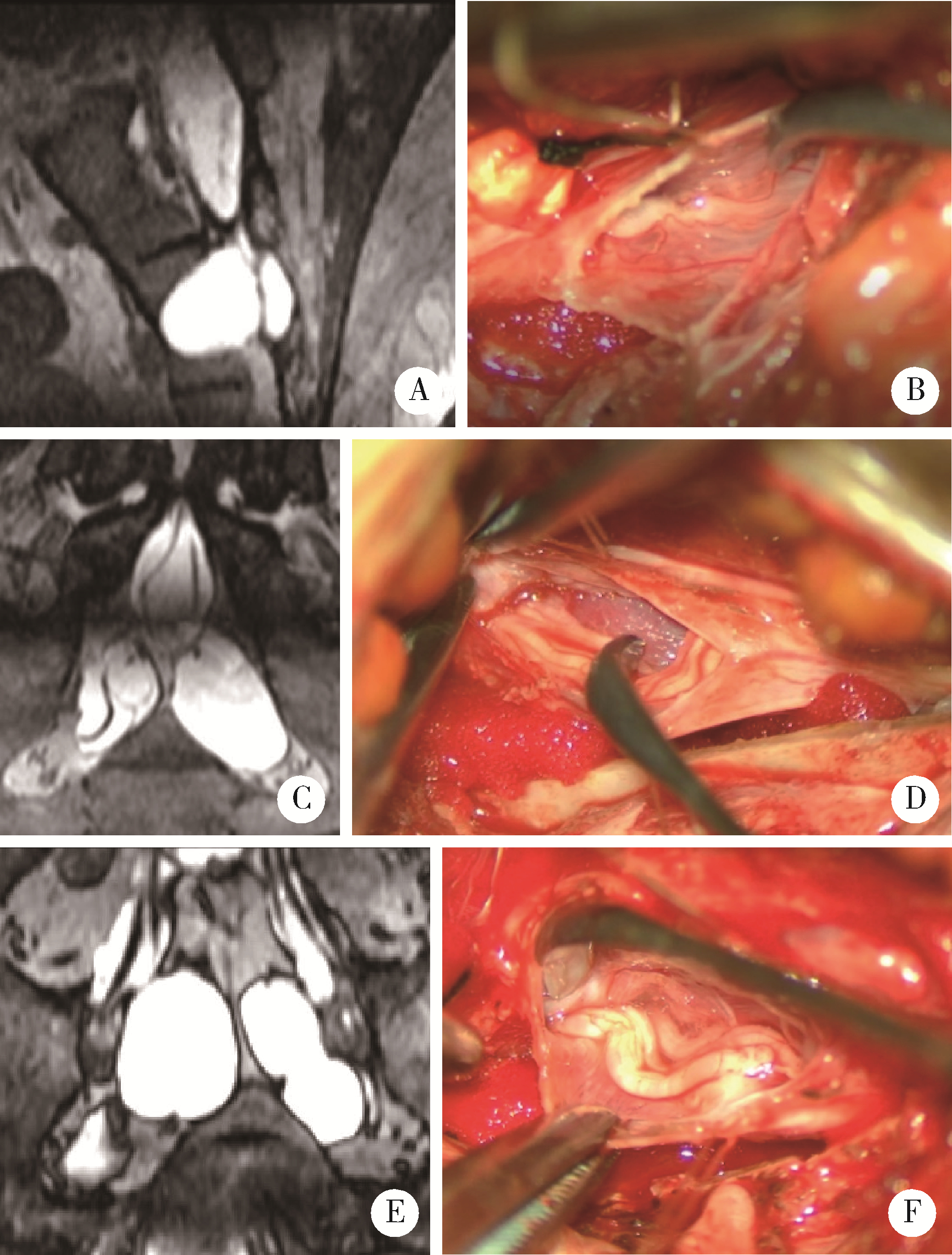
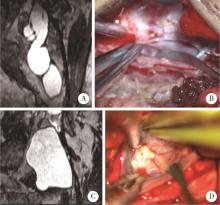
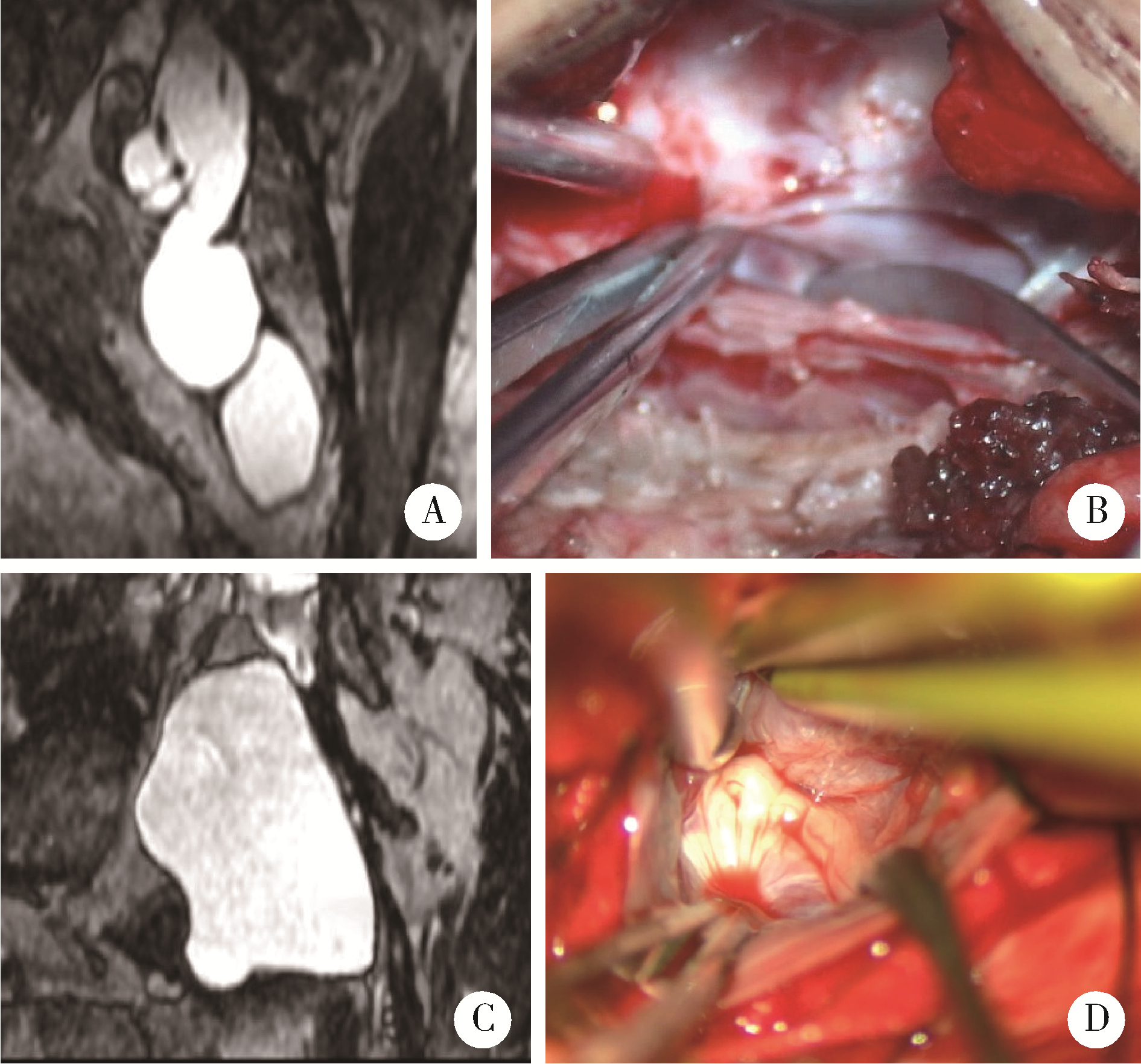
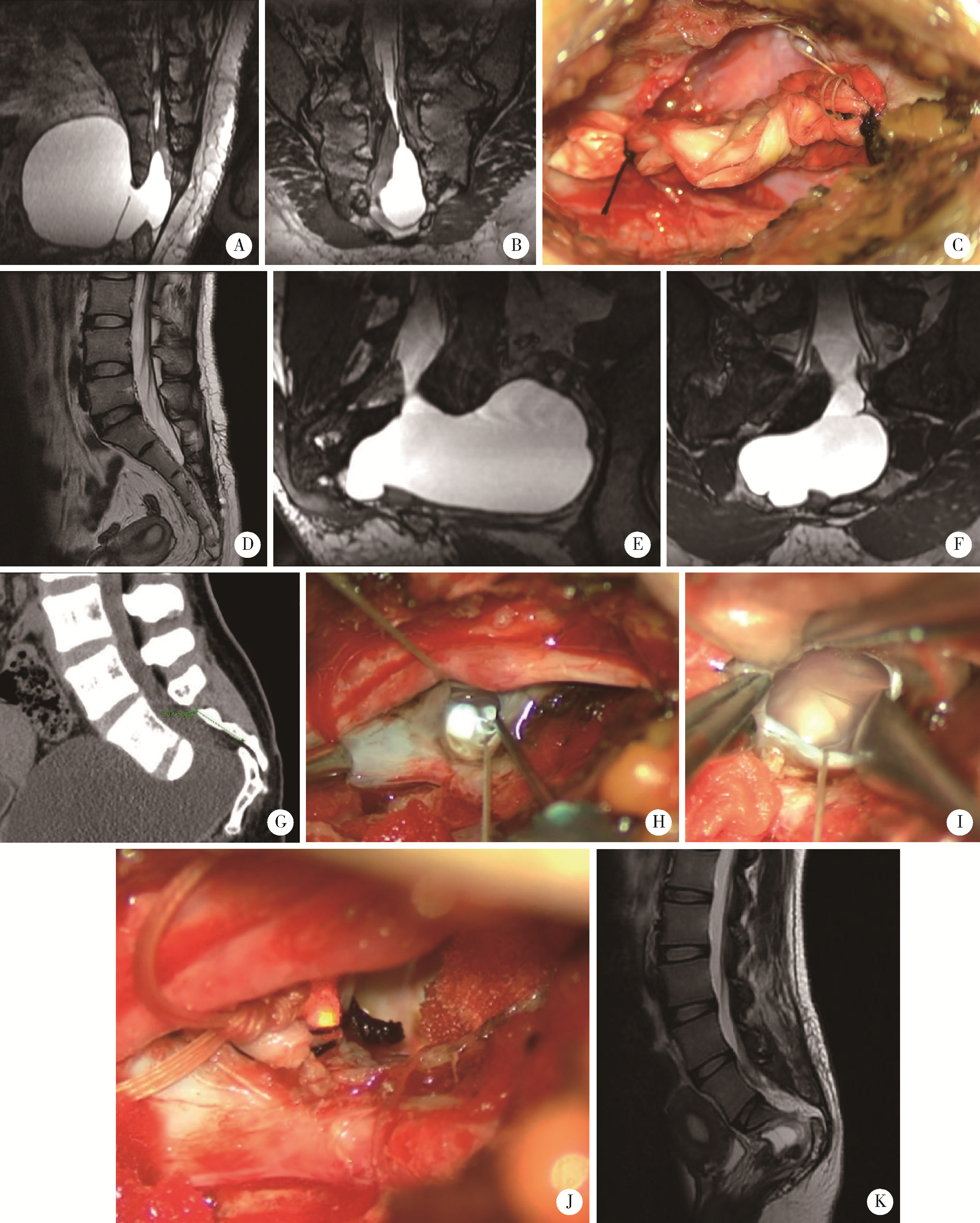
Significance of precise classification of sacral meningeal cysts by multiple dimensions radiographic reconstruction MRI in guiding operative strategy and rehabilitation
Jianjun SUN1,2,*( ), Qianquan MA1, Xiaoliang YIN1, Chenlong YANG1, Jia ZHANG1, Suhua CHEN1, Chao WU1, Jingcheng XIE1, Yunfeng HAN1, Guozhong LIN1, Yu SI1, Jun YANG1, Haibo WU3, Qiang ZHAO3
), Qianquan MA1, Xiaoliang YIN1, Chenlong YANG1, Jia ZHANG1, Suhua CHEN1, Chao WU1, Jingcheng XIE1, Yunfeng HAN1, Guozhong LIN1, Yu SI1, Jun YANG1, Haibo WU3, Qiang ZHAO3
- 1. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
2. Department of Neurosurgery, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
3. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R739.42
| 1 |
Sun JJ , Wang ZY , Li ZD , et al. Reconstruction of nerve root sheaths for sacral extradural spinal meningeal cysts with spinal nerve root fibers[J]. Sci China Life Sci, 2013, 56 (11): 1007- 1013.
doi: 10.1007/s11427-013-4536-7 |
| 2 |
Sun JJ , Wang ZY , Teo M , et al. Comparative outcomes of the two types of sacral extradural spinal meningeal cysts using different operation methods: A prospective clinical study[J]. PLoS One, 2013, 8 (12): e83964.
doi: 10.1371/journal.pone.0083964 |
| 3 |
Sun JJ , Wang ZY , Liu B , et al. Neck transfixion for sacral extradural spinal meningeal cysts without spinal nerve root fibers[J]. Eur Spine J, 2016, 25 (6): 1945- 1952.
doi: 10.1007/s00586-014-3471-z |
| 4 | 谢京城, 王振宇, 陈晓东. 骶管终丝脊膜囊肿合并脊髓拴系综合征的诊断和治疗[J]. 中国临床神经外科杂志, 2015, 20 (11): 651- 653. |
| 5 |
Weigel R , Polemikos M , Uksul N , et al. Tarlov cysts: Long-term follow-up after microsurgical inverted plication and sacroplasty[J]. Eur Spine J, 2016, 25 (11): 3403- 3410.
doi: 10.1007/s00586-016-4744-5 |
| 6 | Hulens M , Bruyninckx F , Dankaerts W , et al. Electromyographic abnormalities associated with symptomatic sacral Tarlov cysts[J]. Pain Pract, 2016, 16 (5): E81- E88. |
| 7 |
Hulens M , Rasschaert R , Bruyninckx F , et al. Symptomatic Tarlov cysts are often overlooked: Ten reasons why: A narrative review[J]. Eur Spine J, 2019, 28 (10): 2237- 2248.
doi: 10.1007/s00586-019-05996-1 |
| 8 |
Fletcher SA , Mirza S , Burström G , et al. Management of perineural (Tarlov) cysts: A population-based cohort study and algorithm for the selection of surgical candidates[J]. Acta Neurochir (Wien), 2019, 161 (9): 1909- 1915.
doi: 10.1007/s00701-019-04000-5 |
| 9 |
Yang AI , Rinehart CD , McShane BJ , et al. Growth of lumbosacral perineural (Tarlov) cysts: A natural history analysis[J]. Neurosurgery, 2020, 86 (1): 88- 92.
doi: 10.1093/neuros/nyy586 |
| 10 |
Hulens M , Bruyninckx F , Dankaerts W , et al. High prevalence of perineural cysts in patients with fibromyalgia and chronic fatigue syndrome[J]. Pain Med, 2021, 22 (4): 883- 890.
doi: 10.1093/pm/pnaa410 |
| 11 |
Dowsett LE , Clement F , Coward S , et al. Effectiveness of surgical treatment for Tarlov cysts: A systematic review of published literature[J]. Clin Spine Surg, 2018, 31 (9): 377- 384.
doi: 10.1097/BSD.0000000000000582 |
| 12 | Telfeian AE , Doberstein C , Oyelese AA , et al. Transforaminal endoscopic approach for treatment of a lumbar perineural cyst: Technical note[J]. World Neurosurg, 2019, 127 (7): 85- 91. |
| 13 |
Wang Z , Jian F , Chen Z , et al. Percutaneous spinal endoscopic treatment of symptomatic sacral Tarlov cysts[J]. World Neurosurg, 2022, 158, e598- e604.
doi: 10.1016/j.wneu.2021.11.019 |
| 14 |
Ma QQ , Zhang J , Yang CL , et al. Arachnoidal diverticula of sacral extradural meningeal cyst: A novel definition and case series[J]. World Neurosurg, 2022, 163, e106- e112.
doi: 10.1016/j.wneu.2022.03.052 |
| 15 |
Tsuchimochi K , Morioka T , Murakami N , et al. Huge multiple spinal extradural meningeal cysts in infancy[J]. Childs Nerv Syst, 2019, 35 (3): 535- 540.
doi: 10.1007/s00381-018-4009-1 |
| 16 | 王奥楠, 邬海博, 孙建军. 三维快速稳态采集成像序列术前评估神经根型骶管囊肿的价值[J]. 实用放射学杂志, 2021, 37 (10): 15- 17. |
| [1] | Yuxuan TIAN,Mingjian RUAN,Yi LIU,Derun LI,Jingyun WU,Qi SHEN,Yu FAN,Jie JIN. Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 567-574. |
| [2] | Yi LIU,Chang-wei YUAN,Jing-yun WU,Qi SHEN,Jiang-xi XIAO,Zheng ZHAO,Xiao-ying WANG,Xue-song LI,Zhi-song HE,Li-qun ZHOU. Diagnostic efficacy of prostate cancer using targeted biopsy with 6-core systematic biopsy for patients with PI-RADS 5 [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 812-817. |
| [3] | Chang-wei YUAN,De-run LI,Zhi-hua LI,Yi LIU,Gang-zhi SHAN,Xue-song LI,Li-qun ZHOU. Application of dynamic contrast enhanced status in multiparametric magnetic resonance imaging for prostatic cancer with PI-RADS 4 lesion [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 838-842. |
| [4] | Ying LIU,Ran HUO,Hui-min XU,Zheng WANG,Tao WANG,Hui-shu YUAN. Correlations between plaque characteristics and cerebral blood flow in patients with moderate to severe carotid stenosis using magnetic resonance vessel wall imaging [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 646-651. |
| [5] | Qiang FU,Guan-ying GAO,Yan XU,Zhuo-hua LIN,You-jing SUN,Li-gang CUI. Comparative study of ultrasound and magnetic resonance imaging in the diagnosis of asymptomatic anterosuperior acetabular labrum tears [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 665-669. |
| [6] | Shan YE,Ping-ping JIN,Nan ZHANG,Hai-bo WU,Lin SHI,Qiang ZHAO,Kun YANG,Hui-shu YUAN,Dong-sheng FAN. Cortical thickness and cognitive impairment in patients with amyotrophic lateral sclerosis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1158-1162. |
| [7] | Ying CAI,Qiao-qin WAN,Xian-jie CAI,Ya-juan GAO,Hong-bin HAN. Epidural photobiomodulation accelerates the drainage of brain interstitial fluid and its mechanism [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1000-1005. |
| [8] | WANG Shu-lei,GAO Yang-xu,ZHANG Hong-wu,YANG Hai-bo,LI Hui,LI Yu,SHEN Li-xue,YAO Hong-xin. Clinical analysis of 30 cases of basal ganglia germinoma in children [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 222-226. |
| [9] | ZHANG Fan,CHEN Qu,HAO Yi-chang,YAN Ye,LIU Cheng,HUANG Yi,MA Lu-lin. Relationship between recovery of urinary continence after laparoscopic radical prostatectomy and preoperative/postoperative membranous urethral length [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 299-303. |
| [10] | Yi-fan WU,Xiao-yuan ZHANG,Shuang REN,Ying-xiang YU,Cui-qing CHANG. Measurement and evaluation of the quadriceps muscle mass in young men based on magnetic resonance imaging [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 843-849. |
| [11] | Hui SHENG,Lei LIANG,Tong-liang ZHOU,Yan-xing JIA,Tong WANG,Lan YUAN,Hong-bin HAN. Improved synthesis process of optical-magnetic bimodal probe of Gd-[4,7-Bis-carboxymethyl-10-(2-fluoresceinthioureaethyl)-1,4,7,10-tetraaza-cyclododec-1-yl]-acetic acid complexes [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 959-963. |
| [12] | Shi-ming ZHAO,Tie-jun YANG,Chun-miao XU,Xiao-feng GUO,Yong-kang MA,Xue-jun CHEN,Xiang LI,Chao-hong HE. Bladder cancer local staging about muscle invasion: 3.0T MRI performance following transurethral resection [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 701-704. |
| [13] | Meng-meng ZHENG,Guang-pu DING,Wei-jie ZHU,Kun-lin YANG,Shu-bo FAN,Bao GUAN,Xin-fei LI,Yu-kun CAI,Jin-sheng ZHANG,Xue-song LI,Li-qun ZHOU. Application of preoperative three-dimensional image reconstruction in the treatment of ureteropelvic junction obstruction [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 705-710. |
| [14] | Yu SONG,Hong-bin HAN,Jun YANG,Ai-bo WANG,Qing-yuan HE,Yuan-yuan LI,Guo-mei ZHAO,Ya-juan GAO,Rui WANG,Yi-xing HAN,Ai-lian LIU,Qing-wei SONG. Effect of convection enhanced delivery on the microstructure of brain extracellular space in aged rats [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 362-367. |
| [15] | Li XU,Ming-jie HU,Yu-yu LI,Hong-dang QU,Wei-dong QIAN,Xiao-lin LIU. Superficial siderosis of the central nervous system caused by myxopapillary ependymoma of conus medullaris and cauda equine: a case report and literature review [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 769-774. |
|
||