Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (6): 1067-1073. doi: 10.19723/j.issn.1671-167X.2025.06.008
Previous Articles Next Articles
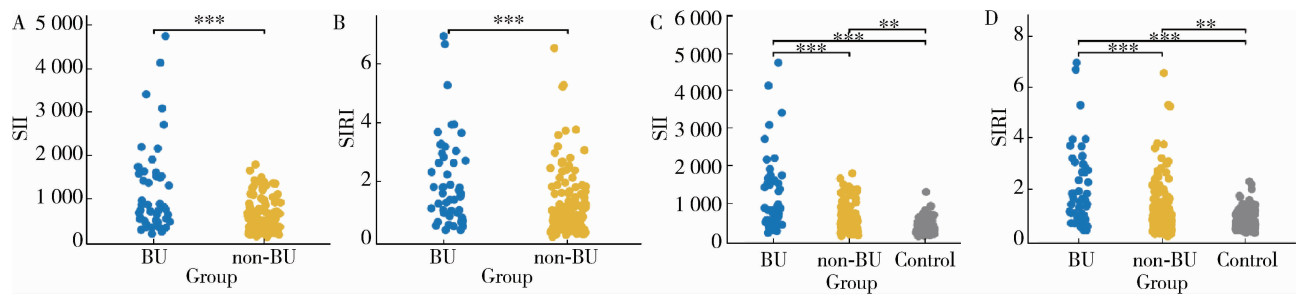
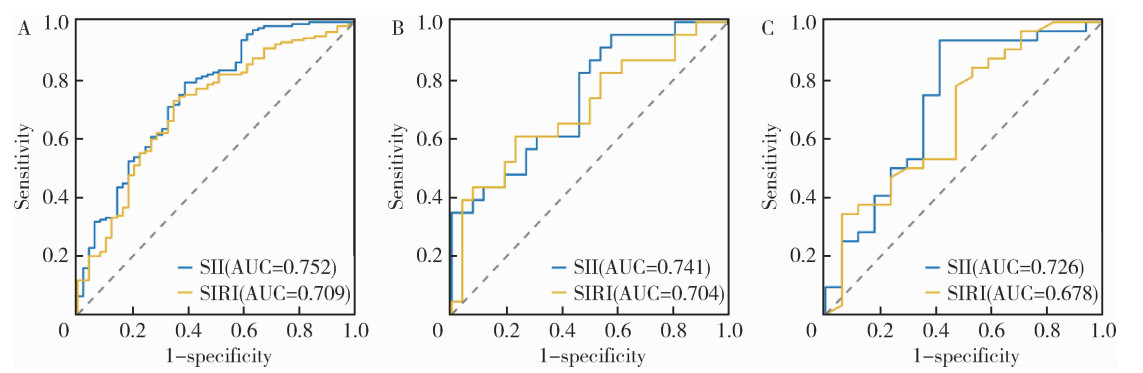
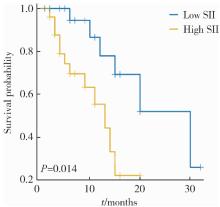
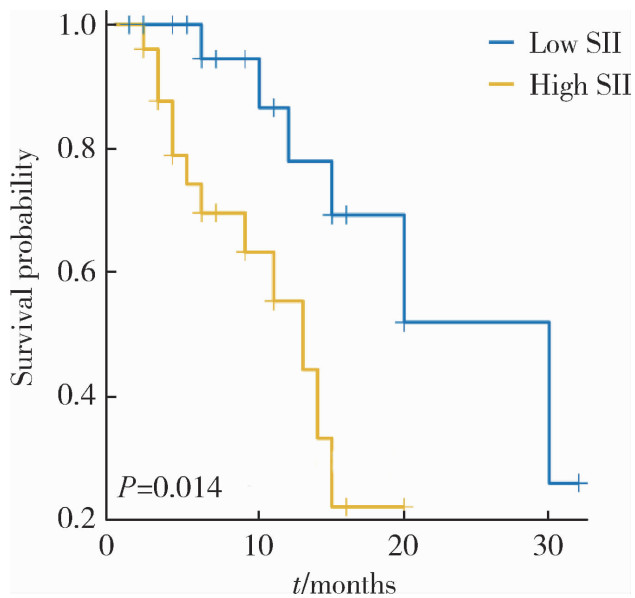
Role of the SII and SIRI in risk prediction, disease activity assessment, and prog-nostic evaluation of Behçet disease uveitis
Yajing GAO1,2,3, Zhengfang LI1,3, Mengsi MA1,2,3, Lijun WU1,3,*( )
)
- 1. Department of Rheumatology and Immunology, People's Hospital of Xinjiang Uygur Autonomous Region, Uygur 830000, China
2. Xinjiang Medical University, Uygur 830000, China
3. Xinjiang Clinical Research Center for Rheumatoid Arthritis, Uygur 830000, China
CLC Number:
- R593.22
| 1 |
|
| 2 |
doi: 10.1002/art.41998 |
| 3 |
doi: 10.1007/s10067-020-05026-2 |
| 4 |
doi: 10.1016/j.preteyeres.2023.101216 |
| 5 |
doi: 10.4103/tjem.tjem_198_23 |
| 6 |
doi: 10.3389/fimmu.2025.1530534 |
| 7 |
doi: 10.3389/fnut.2024.1353964 |
| 8 |
doi: 10.1111/jdv.12107 |
| 9 |
doi: 10.1093/rheumatology/38.8.728 |
| 10 |
doi: 10.1080/25785826.2020.1800244 |
| 11 |
|
| 12 |
doi: 10.1002/advs.202411524 |
| 13 |
|
| 14 |
|
| 15 |
|
| 16 |
doi: 10.1007/s12026-021-09194-4 |
| [1] | Tao WU, Jianzi LIN, Yafeng ZHU, Jianda MA, Peiwen JIA, Lijuan YANG, jie PAN, Yaowei ZOU, Ying YANG, Ye LU, Lie DAI. Serum inter-alpha-trypsin inhibitor heavy chain H3 is identified as a potential biomarker for myopenia in patients with rheumatoid arthritis using proteomic profiling [J]. Journal of Peking University (Health Sciences), 2025, 57(6): 1024-1031. |
| [2] | Xuebing LYU, Xuanhua YU, Weizhen ZHANG, Changquan LIU, Huhan LIN, Shanting ZENG, Huijuan HUANG, Yueping WU. Rheumatoid arthritis complicated with necrotizing fasciitis: A case report [J]. Journal of Peking University (Health Sciences), 2025, 57(6): 1198-1202. |
| [3] | Ju YANG, Jing XU, Juhua DAI, Lianjie SHI. Expression of lumican protein in serum of patients with rheumatoid arthritis and its correlation with disease and immune activities [J]. Journal of Peking University (Health Sciences), 2025, 57(5): 911-918. |
| [4] | Lianghua FENG, Lirong HONG, Yujia CHEN, Xueming CAI. Role and mechanism of ubiquitin-specific protease 35 in ferroptosis of rheumatoid arthritis-fibroblast like synoviocytes [J]. Journal of Peking University (Health Sciences), 2025, 57(5): 919-925. |
| [5] | Yijun HAN, Xiaoli CHEN, Changhong LI, Jinxia ZHAO. Application status of methotrexate in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 994-1000. |
| [6] | Peiwen JIA, Ying YANG, Yaowei ZOU, Zhiming OUYANG, Jianzi LIN, Jianda MA, Kuimin YANG, Lie DAI. Clinical characteristics of overlapping syndromes of low muscle mass in patients with rheumatoid arthritis and their impact on physical function [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1009-1016. |
| [7] | Doudou MA, Zhemin LU, Qian GUO, Sha ZHU, Jin GU, Yan DING, Lianjie SHI. Successful treatment of rheumatoid arthritis complicated with myasthenia gravis with low-dose rituximab: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1110-1114. |
| [8] | Rui YAN, Dan KE, Yan ZHANG, Li LI, Huanran SU, Wei CHEN, Mingxia SUN, Xiaomin LIU, Liang LUO. Diagnostic significance of serum chemokine CXCL-10 and Krebs von den lungen-6 level in patients with rheumatoid arthritis associated interstitial lung disease [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 956-962. |
| [9] | Zhengfang LI,Cainan LUO,Lijun WU,Xue WU,Xinyan MENG,Xiaomei CHEN,Yamei SHI,Yan ZHONG. Application value of anti-carbamylated protein antibody in the diagnosis of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 729-734. |
| [10] | Huina HUANG,Jing ZHAO,Xiangge ZHAO,Ziran BAI,Xia LI,Guan WANG. Regulatory effect of lactate on peripheral blood CD4+ T cell subsets in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 519-525. |
| [11] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [12] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [13] | Yin-ji JIN,Lin SUN,Jin-xia ZHAO,Xiang-yuan LIU. Significance of IgA isotype of anti-v-raf murine sarcoma viral oncogene homologue B1 antibody in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 631-635. |
| [14] | Wen-xin CAI,Shi-cheng LI,Yi-ming LIU,Ru-yu LIANG,Jing LI,Jian-ping GUO,Fan-lei HU,Xiao-lin SUN,Chun LI,Xu LIU,Hua YE,Li-zong DENG,Ru LI,Zhan-guo LI. A cross-sectional study on the clinical phenotypes of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1068-1073. |
| [15] | Fang CHENG,Shao-ying YANG,Xing-xing FANG,Xuan WANG,Fu-tao ZHAO. Role of the CCL28-CCR10 pathway in monocyte migration in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1074-1078. |
|
||