Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (6): 1145-1152. doi: 10.19723/j.issn.1671-167X.2025.06.019
Previous Articles Next Articles
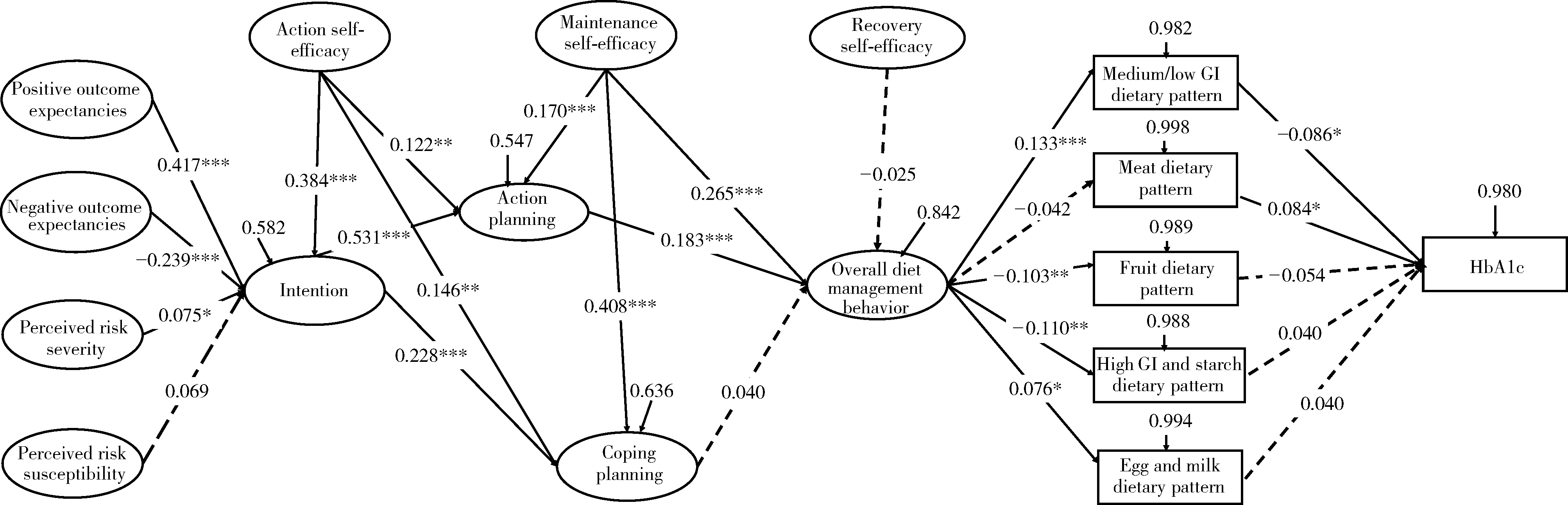
Analyzing the influential factors of dietary patterns and blood glucose control in type 2 diabetes patients based on the model of health action process approach model
Hewei MIN1, Yibo WU1, Yuhui SHI1, Mingzi LI2, Xinying SUN1,*( )
)
- 1. Department of Social Medicine and Health Education, Peking University School of Public Health, Beijing 100191, China
2. Peking University School of Nursing, Beijing 100191, China
CLC Number:
- R193.3
| 1 |
|
| 2 |
doi: 10.1016/j.ajcnut.2023.08.022 |
| 3 |
Schwarzer R, Sniehotta FF, Lippke S, et al. On the assessment and analysis of variables in the health action process approach conducting an investigation[EB/OL]. (2013-11-01)[2024-05-20]. https://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=3FFB18BA8EEC17A6CFA2C9065A98F60Fdoi=10.1.1.388.1394&rep=rep1&type=pdf.
|
| 4 |
doi: 10.1093/heapro/daad095 |
| 5 |
|
| 6 |
doi: 10.1080/08870446.2018.1458983 |
| 7 |
doi: 10.2196/13363 |
| 8 |
doi: 10.1111/aphw.12190 |
| 9 |
doi: 10.1016/j.pcd.2019.08.009 |
| 10 |
陈雪莹. 社区2型糖尿病患者饮食教具干预的效果评价研究[D]. 北京: 北京大学, 2021.
|
| 11 |
doi: 10.2337/diacare.23.7.943 |
| 12 |
doi: 10.1016/0749-5978(91)90020-T |
| 13 |
doi: 10.1037/0278-6133.19.5.487 |
| 14 |
温鑫. 基于HAPA理论慢性肾病健康饮食认知信念问卷的编制及应用研究[D]. 长春: 吉林大学, 2020.
|
| 15 |
doi: 10.2196/40420 |
| 16 |
doi: 10.1038/ejcn.2017.41 |
| 17 |
王雨, 李桂丽, 李颖. 糖尿病患者的膳食模式与伴发心脑血管疾病的关系研究[J]. 营养学报, 2021, 43 (2): 144- 149.
|
| 18 |
doi: 10.1016/j.jacc.2016.06.011 |
| 19 |
doi: 10.3390/nu13010116 |
| 20 |
doi: 10.1186/s12937-017-0303-0 |
| 21 |
doi: 10.1017/S1368980020004930 |
| 22 |
doi: 10.1007/s10654-017-0246-y |
| 23 |
doi: 10.3390/nu14030706 |
| 24 |
|
| 25 |
doi: 10.1016/S0140-6736(14)60613-9 |
| 26 |
doi: 10.1093/ajcn/nqz035 |
| 27 |
doi: 10.1111/obr.12172 |
| 28 |
doi: 10.1093/eurheartj/ehad336 |
| 29 |
doi: 10.1037/a0030182 |
| 30 |
doi: 10.19082/6647 |
| 31 |
doi: 10.1016/j.appet.2013.06.097 |
| 32 |
doi: 10.1111/aphw.12050 |
| 33 |
doi: 10.1111/bjhp.12144 |
| 34 |
曹佃省, 谢光荣. 从行为意向到健康行为: 健康行为程式模型(HAPA)概述[J]. 中国临床心理学杂志, 2010, 18 (6): 809- 812.
|
| 35 |
张持晨, 郑晓, 赵慧宁, 等. 基于健康行为过程取向的大学生膳食行为干预[J]. 卫生研究, 2017, 46 (5): 755- 760.
|
| 36 |
张向京, 岳建华, 林锐. 健康行为HAPA模型为指导提高老年高血压患者自我效能、心理健康和服药依从性的影响[J]. 中国健康心理学杂志, 2021, 29 (8): 1199- 1204.
|
| 37 |
doi: 10.1186/s13098-021-00773-x |
| 38 |
|
| 39 |
赵静, 赵秋利, 王丽敏, 等. 2型糖尿病患者饮食行为改变特征的研究[J]. 中华护理杂志, 2018, 53 (2): 139- 143.
|
| 40 |
郭怡, 孙信, 黎泽明, 等. 基于健康行动过程取向理论模型分析2型糖尿病患者锻炼行为现状[J]. 中华疾病控制杂志, 2022, 26 (1): 56-60, 98.
|
| 41 |
朱金凤, 蔡卫新, 陶子荣, 等. 中青年出血性脑卒中患者康复运动依从性现状及其影响因素分析[J]. 中华护理杂志, 2023, 58 (5): 580- 586.
|
| 42 |
doi: 10.4103/jehp.jehp_175_20 |
| [1] | Ziyan CHEN, Xiaoyue ZHANG, Yiwu GU, Chun CHANG. Type 2 diabetes patients use E-health to manage disease willingness and influence mechanisms [J]. Journal of Peking University (Health Sciences), 2025, 57(3): 522-528. |
| [2] | Lei BAO,Xia-xia CAI,Ming-yuan ZHANG,Lei-lei REN. Effect of vitamin D3 on mild cognitive impairment in type 2 diabetic mice and its possible mechanism [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 587-592. |
| [3] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [4] | Xiao-yue ZHANG,Yu-xin LIN,Ying JIANG,Lan-chao ZHANG,Mang-yan DONG,Hai-yi CHI,Hao-yu DONG,Li-jun MA,Zhi-jing LI,Chun CHANG. Mediating effect of self-efficacy on self-management ability and self-management behavior in patients with type 2 diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 450-455. |
| [5] | CHEN Ping,LI Ze-ming,GUO Yi,SUN Xin-ying,Edwin B. FISHER. To explore medication adherence of patients with type 2 diabetes mellitus using the latent profile analysis based on the Big Five personality theory [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 530-535. |
| [6] | Ze-ming LI,Min GAO,Xue-ying CHEN,Xin-ying SUN. Relationship between the five-factor model of personality traits and self-management attitude of patients with type 2 diabetes [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 506-513. |
| [7] | Jiang XIE,Fei LI. Association of sleep overlap syndrome with type 2 diabetes in a cross-sectional study [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 252-255. |
|
||