Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (6): 982-992. doi: 10.19723/j.issn.1671-167X.2023.06.005
Previous Articles Next Articles
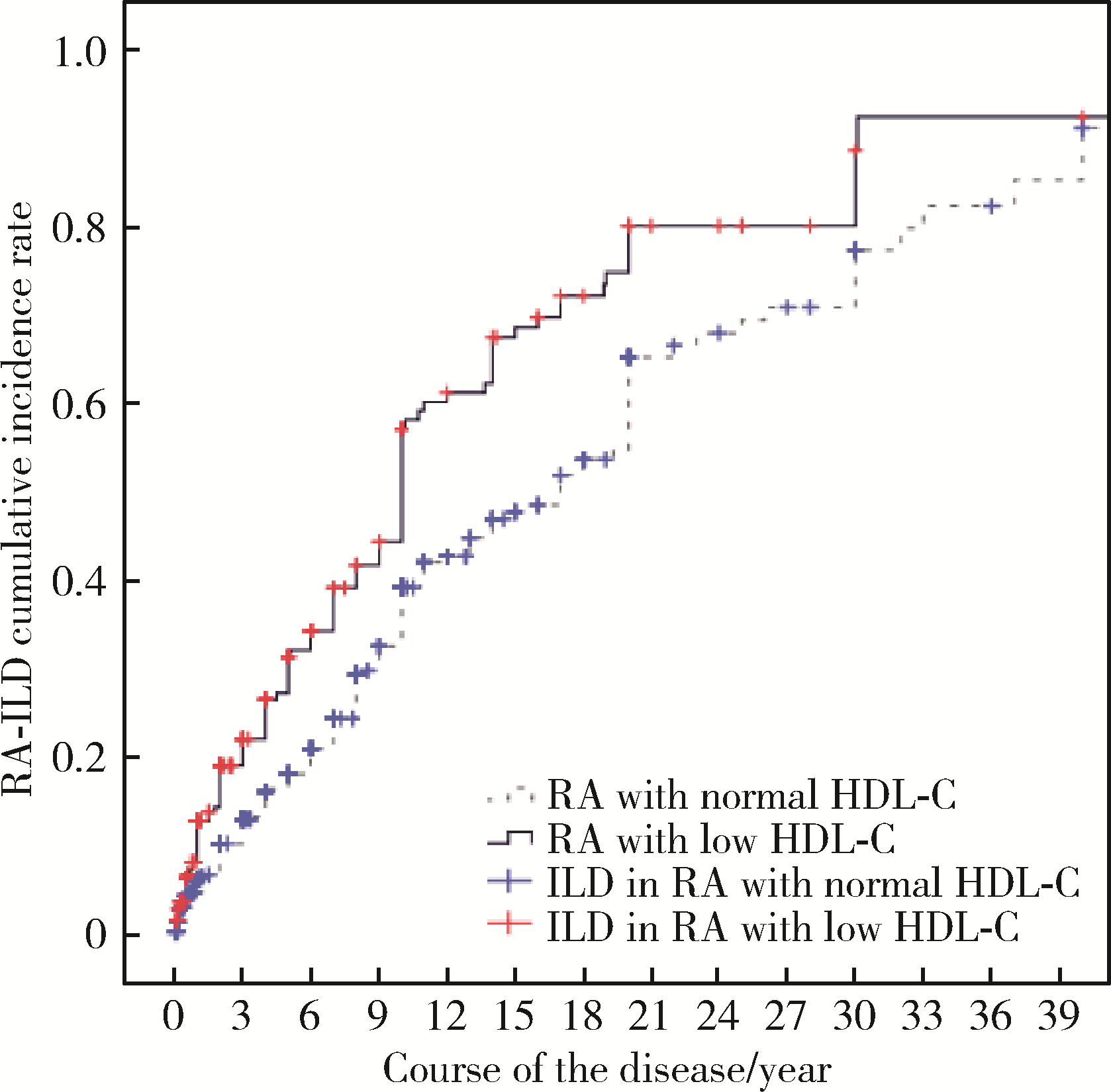
Correlation between dyslipidemia and rheumatoid arthritis associated interstitial lung disease
Qi WU1,2,Yue-ming CAI1,Juan HE1,Wen-di HUANG3,Qing-wen WANG1,*( )
)
- 1. Department of Rheumatism and Immunology, Peking University Shenzhen Hospital; Shenzhen Key Laboratory of Immunity and Inflammatory Diseases, Shenzhen 518000, Guangdong, China
2. Shantou University Medical College, Shantou 515000, Guangdong, China
3. Department of Pulmonary and Critical Care Medicine, Peking University Shenzhen Hospital Shenzhen, Shenzhen 518000, Guangdong, China
CLC Number:
- R593.2
| 1 |
Figus FA , Piga M , Azzolin I , et al. Rheumatoid arthritis: Extra-articular manifestations and comorbidities[J]. Autoimmun Rev, 2021, 20 (4): 102776.
doi: 10.1016/j.autrev.2021.102776 |
| 2 | Suda T . UP-to-date information on rheumatoid arthritis-associated interstitial lung disease[J]. Clin Med Insights Circ Respir Pulm Med, 2015, 9, 155- 162. |
| 3 |
Hyldgaard C , Hilberg O , Pedersen AB , et al. A population-based cohort study of rheumatoid arthritis-associated interstitial lung disease: Comorbidity and mortality[J]. Ann Rheum Dis, 2017, 76, 1700- 1706.
doi: 10.1136/annrheumdis-2017-211138 |
| 4 |
Fazeli M S , Khaychuk V , Wittstock K , et al. Rheumatoid arthritis-associated interstitial lung disease: Epidemiology, risk/prognostic factors, and treatment landscape[J]. Clin Exp Rheumatol, 2021, 39 (5): 1108- 1118.
doi: 10.55563/clinexprheumatol/h9tc57 |
| 5 | Uzma E , Tasnim A , Danish K . Lipid abnormalities in patients with rheumatoid arthritis[J]. Pak J Med SCI, 2017, 33 (1): 227- 230. |
| 6 | 陈哲. 血清脂蛋白异常与IPF关系及其临床意义[D]. 广西: 广西医科大学, 2018. |
| 7 |
Aletaha D , Neogi T , Silman AJ , et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative[J]. Arthritis Rheum, 2010, 62 (9): 2569- 2581.
doi: 10.1002/art.27584 |
| 8 |
Travis WD , Costabel U , Hansell DM , et al. An official American Thoracis Society/European Respiratory Society statement: Update of the international multisciplinary classification of the idiopathic interstitial pneumonias[J]. Am J Respir Crit Care Med, 2013, 188 (6): 733- 748.
doi: 10.1164/rccm.201308-1483ST |
| 9 | 中国成人血脂异常防治指南修订联合委员会. 中国成人血脂异常防治指南(2016年修订版)[J]. 中华全科医师杂志, 2017, 16 (1): 15- 35. |
| 10 |
Semb AG , Ikdahl E , Wibetoe G , et al. Atherosclerotic cardiovascular disease prevention in rheumatoid arthritis[J]. Nat Rev Rheumatol, 2020, 16 (7): 361- 379.
doi: 10.1038/s41584-020-0428-y |
| 11 |
Hollan I , Ronda N , Dessein P , et al. Lipd management in rheumatoid arthritis: A position paper of the Working Group on Cardiovascular Pharmacotherapy of the European Society of Cardiology[J]. Eur Heart J Cardiovasc Pharmacother, 2020, 6 (2): 104- 114.
doi: 10.1093/ehjcvp/pvz033 |
| 12 |
Charles-Schoeman C , Meriwether D , Lee YY , et al. High levels of oxidized fatty acids in HDL are associated with impaired HDL function in patients with active rheumatoid arthritis[J]. Clin Rheumatol, 2018, 37 (3): 615- 622.
doi: 10.1007/s10067-017-3896-y |
| 13 | Gordon EM , Figueroa DM , Barochia AV , et al. High-density lipoproteins and apolipoprotein A-I: Potential new players in the prevention and treatment of lung disease[J]. Front Pharmacol, 2016, 7, 323. |
| 14 |
Hee LE , Eun-Ju L , Jeong KH , et al. Overexpression of apolipoprotein A1 in the lung abrogates fibrosis in experimental silicosis[J]. PloS One, 2013, 8 (2): e55827.
doi: 10.1371/journal.pone.0055827 |
| 15 |
Belchamber K , Donnelly L E . Targeting defective pulmonary innate immunity: A new therapeutic option?[J]. Pharmacol Ther, 2020, 209, 107500.
doi: 10.1016/j.pharmthera.2020.107500 |
| 16 | Tall AR , Yvan-Charvet L . Cholesterol, inflammation and innate immunity[J]. Nat Rev Immunol, 2015, 15 (2): 104- 116. |
| 17 | Laurent YC , Fabrizia B , Renè GR , et al. Immunometabolic function of cholesterol in cardiovascular disease and beyond[J]. Cardiovasc Res, 2019, 115 (9): 1393- 1407. |
| 18 | Chistiakov DA , ORekhov AN , Bobryshev YV . ApoA1 and ApoA1-specific self-antibodies in cardiovascular disease[J]. Lab Invest, 2016, 96 (7): 708- 718. |
| 19 | Vuilleumier N , Bratt J , Alizadeh R , et al. Anti-apoA-1 IgG and oxidized LDL are raised in rheumatoid arthritis (RA): Potential associations with cardiovascular disease and RA disease activity[J]. Scand J Rheumatol, 2010, 39 (6): 447- 453. |
| 20 | Salaffi F , Carotti M , di Carlo M , et al. High-resolution computed tomography of the lung in patients with rheumatoid arthritis: Prevalence of interstitial lung disease involvement and determinants of abnormalities[J]. Medicine (Baltimore), 2019, 98 (38): e17088. |
| 21 | Kelly CA , Saravanan V , Nisar M , et al. Rheumatoid arthritis-related interstitial lung disease: associations, prognostic factors and physiological and radiological characteristics: A large multicentre UK study[J]. Rheumatology (Oxford), 2014, 53 (9): 1676- 1682. |
| 22 | Ito Y , Arita M , Kumagai S , et al. Radiological fibrosis score is strongly associated with worse survival in rheumatoid arthritis-related interstitial lung disease[J]. Mod Rheumatol, 2019, 29 (1): 98- 104. |
| [1] | Dongwu LIU, Jie CHEN, Mingli GAO, Jing YU. Rheumatoid arthritis with Castleman-like histopathology in lymph nodes: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 928-931. |
| [2] | Huina HUANG,Jing ZHAO,Xiangge ZHAO,Ziran BAI,Xia LI,Guan WANG. Regulatory effect of lactate on peripheral blood CD4+ T cell subsets in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 519-525. |
| [3] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [4] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [5] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [6] | Wen-gen LI,Xiao-dong GU,Rui-qiang WENG,Su-dong LIU,Chao CHEN. Expression and clinical significance of plasma exosomal miR-34-5p and miR-142-3p in systemic sclerosis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1022-1027. |
| [7] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Correlation analysis between body mass index and clinical characteristics of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 993-999. |
| [8] | Yin-ji JIN,Lin SUN,Jin-xia ZHAO,Xiang-yuan LIU. Significance of IgA isotype of anti-v-raf murine sarcoma viral oncogene homologue B1 antibody in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 631-635. |
| [9] | Wen-xin CAI,Shi-cheng LI,Yi-ming LIU,Ru-yu LIANG,Jing LI,Jian-ping GUO,Fan-lei HU,Xiao-lin SUN,Chun LI,Xu LIU,Hua YE,Li-zong DENG,Ru LI,Zhan-guo LI. A cross-sectional study on the clinical phenotypes of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1068-1073. |
| [10] | Fang CHENG,Shao-ying YANG,Xing-xing FANG,Xuan WANG,Fu-tao ZHAO. Role of the CCL28-CCR10 pathway in monocyte migration in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1074-1078. |
| [11] | Rui LIU,Jin-xia ZHAO,Liang YAN. Clinical characteristics of patients with rheumatoid arthritis complicated with venous thrombosis of lower extremities [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1079-1085. |
| [12] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1086-1093. |
| [13] | YAN Hui,PANG Lu,LI Xue-ying,YANG Wen-shuang,JIANG Shi-ju,LIU Ping,YAN Cun-ling. Incidence and cause of abnormal cholesterol in children aged 2-18 years in a single center [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 217-221. |
| [14] | GAO Chao,CHEN Li-hong,WANG Li,YAO Hong,HUANG Xiao-wei,JIA Yu-bo,LIU Tian. Validation of the Pollard’s classification criteria (2010) for rheumatoid arthritis patients with fibromyalgia [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 278-282. |
| [15] | LOU Xue,LIAO Li,LI Xing-jun,WANG Nan,LIU Shuang,CUI Ruo-mei,XU Jian. Methylation status and expression of TWEAK gene promoter region in peripheral blood of patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1020-1025. |
|
||