Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (2): 299-306. doi: 10.19723/j.issn.1671-167X.2024.02.015
Previous Articles Next Articles
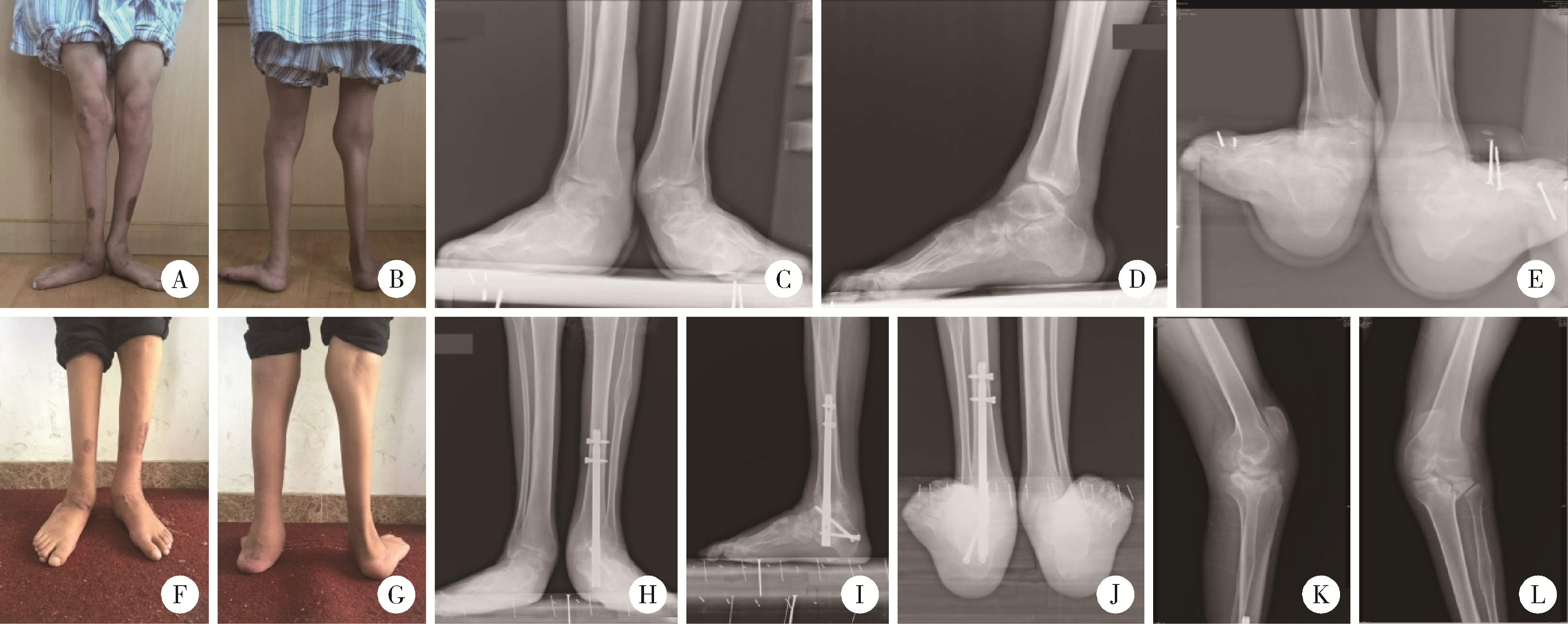
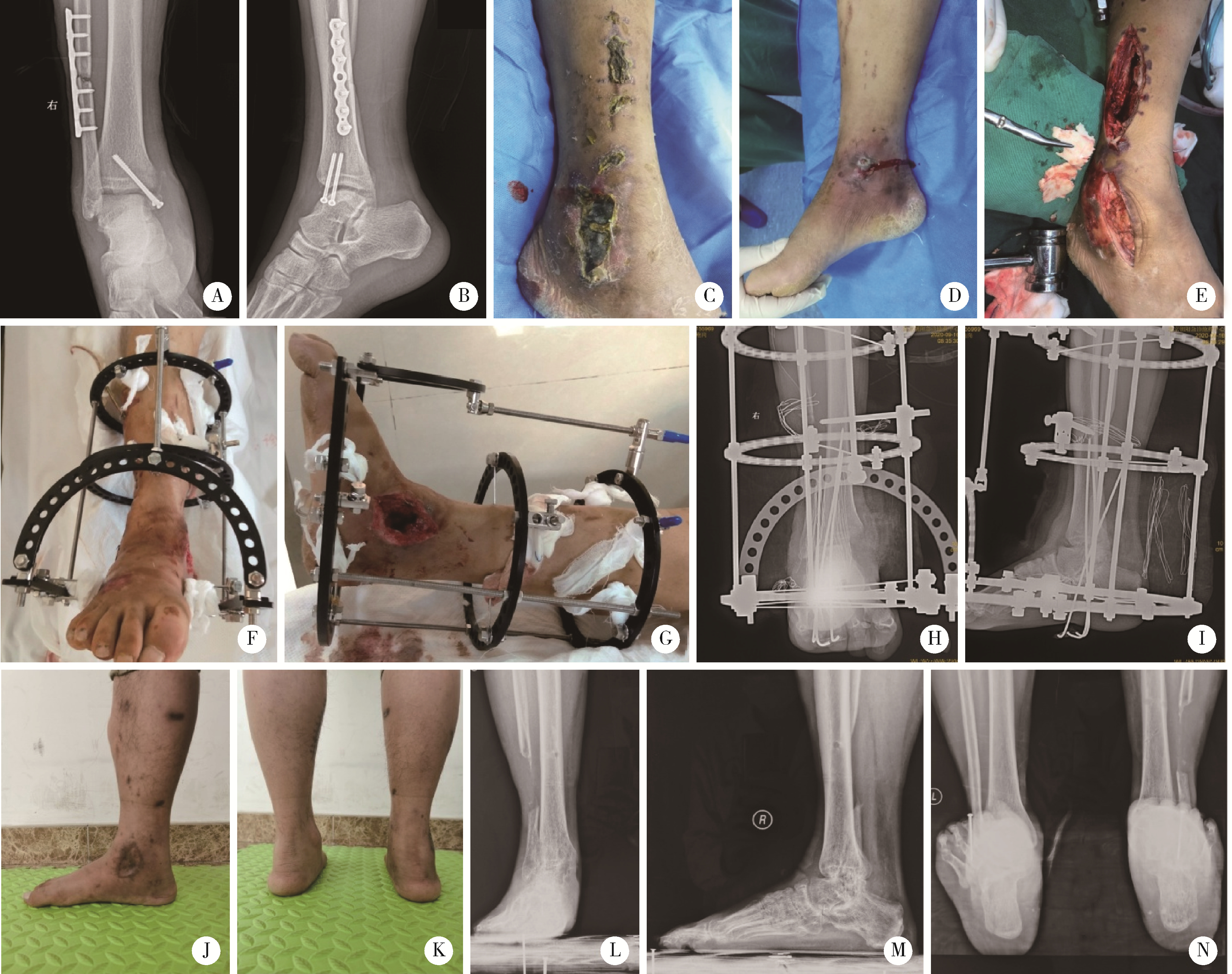
Tibiotalocalcaneal arthrodesis for end-stage ankle and hindfoot arthropathy: Short- and mid-term clinical outcomes
Wenjing LI,Baozhou ZHANG,Heng LI,Liangpeng LAI,Hui DU,Ning SUN,Xiaofeng GONG,Ying LI*( ),Yan WANG,Yong WU
),Yan WANG,Yong WU
- Department of Foot and Ankle Surgery, Beijing Jishuitan Hospital, Capital Medical University, Beijing 100035, China
CLC Number:
- R687.4
| 1 |
Brage ME , Mathews CS . Ankle and tibiotalocalcaneal fusion[J]. Foot Ankle Clin, 2022, 27 (2): 343- 353.
doi: 10.1016/j.fcl.2021.11.020 |
| 2 |
Stołtny T , Dugiełło B , Pasek J , et al. Tibiotalocalcaneal arthrodesis in osteoarthritis deformation of ankle and subtalar joint: Evaluation of treatment results[J]. J Foot Ankle Surg, 2022, 61 (1): 205- 211.
doi: 10.1053/j.jfas.2021.09.005 |
| 3 |
Yao Y , Mo Z , Wu G , et al. A personalized 3D-printed plate for tibiotalocalcaneal arthrodesis: Design, fabrication, biomechanical evaluation and postoperative assessment[J]. Comput Biol Med, 2021, 133, 104368.
doi: 10.1016/j.compbiomed.2021.104368 |
| 4 |
Perez-Aznar A , Gonzalez-Navarro B , Bello-Tejeda LL , et al. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: A prospective cohort study at a minimum five year follow-up[J]. Int Orthop, 2021, 45 (9): 2299- 2305.
doi: 10.1007/s00264-020-04904-3 |
| 5 |
Pitts C , Alexander B , Washington J , et al. Factors affecting the outcomes of tibiotalocalcaneal fusion[J]. Bone Joint J, 2020, 102-B (3): 345- 351.
doi: 10.1302/0301-620X.102B3.BJJ-2019-1325.R1 |
| 6 |
Kitaoka HB , Alexander IJ , Adelaar RS , et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes[J]. Foot Ankle Int, 1994, 15 (7): 349- 353.
doi: 10.1177/107110079401500701 |
| 7 |
Reed MD , van Nostran W . Assessing pain intensity with the visual analog scale: A plea for uniformity[J]. J Clin Pharmacol, 2014, 54 (3): 241- 244.
doi: 10.1002/jcph.250 |
| 8 |
Martínez-de-Albornoz P , Monteagudo M . Tibiotalocalcaneal arthrodesis in severe hindfoot deformities[J]. Foot Ankle Clin, 2022, 27 (4): 847- 866.
doi: 10.1016/j.fcl.2022.08.008 |
| 9 |
Burns PR , Dunse A . Tibiotalocalcaneal arthrodesis for foot and ankle deformities[J]. Clin Podiatr Med Surg, 2017, 34 (3): 357- 380.
doi: 10.1016/j.cpm.2017.02.007 |
| 10 |
Monteagudo M , Martínez-de-Albornoz P . Deciding between ankle and tibiotalocalcaneal arthrodesis for isolated ankle arthritis[J]. Foot Ankle Clin, 2022, 27 (1): 217- 231.
doi: 10.1016/j.fcl.2021.11.012 |
| 11 |
Rana B , Patel S . Results of ankle and hind foot arthrodesis in diabetic Charcot neuroarthropathy: A retrospective analysis of 44 patients[J]. J Clin Orthop Trauma, 2021, 23, 101637.
doi: 10.1016/j.jcot.2021.101637 |
| 12 |
Chraim M , Krenn S , Alrabai HM , et al. Mid-term follow-up of patients with hindfoot arthrodesis with retrograde compression intramedullary nail in Charcot neuroarthropathy of the hindfoot[J]. Bone Joint J, 2018, 100-B (2): 190- 196.
doi: 10.1302/0301-620X.100B2.BJJ-2017-0374.R2 |
| 13 |
Kollig E , Esenwein SA , Muhr G , et al. Fusion of the septic ankle: Experience with 15 cases using hybrid external fixation[J]. J Trauma, 2003, 55 (4): 685- 691.
doi: 10.1097/01.TA.0000051933.83342.E4 |
| 14 |
Hartmann R , Grubhofer F , Waibel FWA , et al. Treatment of hindfoot and ankle infections with Ilizarov external fixator or spacer, followed by secondary arthrodesis[J]. J Orthop Res, 2021, 39 (10): 2151- 2158.
doi: 10.1002/jor.24938 |
| 15 |
Baumbach SF , Massen FK , Hörterer S , et al. Comparison of arthroscopic to open tibiotalocalcaneal arthrodesis in high-risk patients[J]. Foot Ankle Surg, 2019, 25 (6): 804- 811.
doi: 10.1016/j.fas.2018.10.006 |
| 16 |
Rausch S , Loracher C , Fröber R , et al. Anatomical evaluation of different approaches for tibiotalocalcaneal arthrodesis[J]. Foot Ankle Int, 2014, 35 (2): 163- 167.
doi: 10.1177/1071100713517095 |
| 17 |
Wu M , Scott D , Abar B , et al. Does a fibula-sparing approach improve outcomes in tibiotalocalcaneal arthrodesis?[J]. Foot Ankle Surg, 2023, 29 (1): 90- 96.
doi: 10.1016/j.fas.2022.11.001 |
| 18 |
Carranza-Bencano A , Tejero S , Del CG , et al. Minimal incision surgery for tibiotalocalcaneal arthrodesis[J]. Foot Ankle Int, 2014, 35 (3): 272- 284.
doi: 10.1177/1071100713515447 |
| 19 |
Pellegrini MJ , Schiff AP , Adams SJ , et al. Outcomes of tibiotalocalcaneal arthrodesis through a posterior Achilles tendon-splitting approach[J]. Foot Ankle Int, 2016, 37 (3): 312- 319.
doi: 10.1177/1071100715615398 |
| 20 |
Eckholt S , Garcia-Elvira R , Fontecilla N , et al. Role of extra-articular tibiotalocalcaneal arthrodesis and posterior approach in highly complex cases[J]. Foot Ankle Int, 2018, 39 (2): 219- 225.
doi: 10.1177/1071100717737973 |
| 21 |
Gong J , Zhou B , Tao X , et al. Tibiotalocalcaneal arthrodesis with headless compression screws[J]. J Orthop Surg Res, 2016, 11 (1): 91.
doi: 10.1186/s13018-016-0425-7 |
| 22 |
Gutteck N , Schilde S , Reichel M , et al. Posterolateral plate fixation with Pantalarlock® is more stable than nail fixation in tibiotalocalcaneal arthrodesis in a biomechanical cadaver study[J]. Foot Ankle Surg, 2020, 26 (3): 328- 333.
doi: 10.1016/j.fas.2019.04.006 |
| 23 |
Richman J , Cota A , Weinfeld S . Intramedullary nailing and external ring fixation for tibiotalocalcaneal arthrodesis in Charcot arthropathy[J]. Foot Ankle Int, 2017, 38 (2): 149- 152.
doi: 10.1177/1071100716671884 |
| [1] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [2] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [3] | Lei WANG,Tian-dong HAN,Wei-xing JIANG,Jun LI,Dao-xin ZHANG,Ye TIAN. Comparison of safety and effectiveness of active migration technique and in situ lithotripsy technique in the treatment of 1-2 cm upper ureteral calculi by flexible ure-teroscopy [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 553-557. |
| [4] | Shi-kai XIONG,Wei-li SHI,An-hong WANG,Xing XIE,Qin-wei GUO. Radiographic diagnosis of distal fibula avulsion fractures: Comparison of ankle X-ray and three-dimensional reconstruction of CT [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 156-159. |
| [5] | LI Wei-hao,LI Wei,ZHANG Xue-min,LI Qing-le,JIAO Yang,ZHANG Tao,JIANG Jing-jun,ZHANG Xiao-ming. Comparison of the outcomes between open and hybrid approaches in the treatment of thoracoabdominal aortic aneurysms repair [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 177-181. |
| [6] | Yan-fang JIANG,Jian WANG,Yong-jian WANG,Jia LIU,Yin PEI,Xiao-peng LIU,Ying-fang AO,Yong MA. Mid-to-long term clinical outcomes and predictors after anterior cruciate ligament revision [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 857-863. |
| [7] | Zheng-da ZHU,Yan GAO,Wen-xiu HE,Xin FANG,Yang LIU,Pan WEI,Zhi-min YAN,Hong HUA. Efficacy and safety of Nocardia rubra cell wall skeleton for the treatment of erosive oral lichen planus [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 964-969. |
| [8] | LIU Li-li,LIU Zhi-ke,ZHANG Liang,LI Ning,FANG Ting,Dong-ZHANG Liang,XU Guo-zhang,ZHAN Si-yan. Epidemiological and etiological characteristics of hand, foot and mouth disease among children aged 5 years and younger in Ningbo (2016 to 2019) [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 491-497. |
| [9] | WU Jing-heng, TIAN Guang-lei, TIAN Meng-meng, CHEN Shan-lin. Clinical characteristics of 170 cases of macrodactyly [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 590-593. |
| [10] | HOU Zong-chen,AO Ying-fang,HU Yue-lin,JIAO Chen,GUO Qin-wei,HUANG Hong-shi,REN Shuang,ZHANG Si,XIE Xing,CHEN Lin-xin,ZHAO Feng,PI Yan-bin,LI Nan,JIANG Dong. Characteristics and related factors of plantar pressure in the chronic ankle instability individuals [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 279-285. |
| [11] | Xiao LI,Jia-zeng SU,Yan-yan ZHANG,Li-qi ZHANG,Ya-qiong ZHANG,Deng-gao LIU,Guang-yan YU. Inflammation grading and sialoendoscopic treatment of131I radioiodine-induced sialadenitis [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 586-590. |
| [12] | Ying ZHAN,Yi-tian DU,Zhen-zhen YANG,Chun-li ZHANG,Xian-rong QI. Preparation and characterization of paclitaxel microspheres in situ gel and its antitumor efficacy by local injection [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 477-486. |
| [13] | Dong JIANG,Yue-lin HU,Chen JIAO,Qin-wei GUO,Xing XIE,Lin-xin CHEN,Feng ZHAO,Yan-bin PI. Mid-to-long term outcomes and influence factors of postoperative concurrent chronic ankle instability and posterior ankle impingement [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 505-509. |
| [14] | Ze-chuan YANG,Chao-xu LIU,Yang LIN,Wei-hua HU,Wen-jian CHEN,Feng LI,Heng ZENG. All levels miniplate fixation and a modified hybrid fixation method in expansive open-door cervical laminoplasty: a retrospective comparative study [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 187-193. |
| [15] | Wen-zhe YOU,Gui-li DOU,Bin XIA. Two-year outcomes and the influence factors of indirect pulp treatment in primary teeth: a retrospective study [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 65-69. |
|
||