Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (3): 397-402. doi: 10.19723/j.issn.1671-167X.2024.03.004
Previous Articles Next Articles
Association between self-control and co-occurrence of depressive symptoms and overweight or obesity during adolescence and early adulthood: A ten-year prospective cohort study based on national surveys
Jing CHEN1,Rui SHAN1,Wucai XIAO1,Xiaorui ZHANG2,Zheng LIU1,*( )
)
- 1. Department of Maternal and Child Health, Peking University School of Public Health, Beijing 100191, China
2. Department of Pediatrics, Peking University People's Hospital, Beijing 100044, China
CLC Number:
- R479.4
| 1 |
Sawyer SM , Afifi RA , Bearinger LH , et al. Adolescence: A foundation for future health[J]. Lancet, 2012, 379 (9826): 1630- 1640.
doi: 10.1016/S0140-6736(12)60072-5 |
| 2 |
McGrath JJ , Al-Hamzawi A , Alonso J , et al. Age of onset and cumulative risk of mental disorders: A cross-national analysis of population surveys from 29 countries[J]. Lancet Psychiatry, 2023, 10 (9): 668- 681.
doi: 10.1016/S2215-0366(23)00193-1 |
| 3 |
Rao DP , Kropac E , Do MT , et al. Childhood overweight and obesity trends in Canada[J]. Health Promot Chronic Dis Prev Can, 2016, 36 (9): 194- 198.
doi: 10.24095/hpcdp.36.9.03 |
| 4 |
Shorey S , Ng ED , Wong CHJ . Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta-analysis[J]. Br J Clin Psychol, 2022, 61 (2): 287- 305.
doi: 10.1111/bjc.12333 |
| 5 |
NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults[J]. Lancet, 2017, 390 (10113): 2627- 2642.
doi: 10.1016/S0140-6736(17)32129-3 |
| 6 | World Health Organization. Depression and other common mental disorders: Global health estimates[R]. Geneva: World Health Organization, 2017. |
| 7 |
Chooi YC , Ding C , Magkos F . The epidemiology of obesity[J]. Metabolism, 2019, 92, 6- 10.
doi: 10.1016/j.metabol.2018.09.005 |
| 8 |
Smith JD , Fu E , Kobayashi MA . Prevention and management of childhood obesity and its psychological and health comorbidities[J]. Annu Rev Clin Psychol, 2020, 16, 351- 378.
doi: 10.1146/annurev-clinpsy-100219-060201 |
| 9 | Jelalian E , Jandasek B , Wolff JC , et al. Cognitive-behavioral therapy plus healthy lifestyle enhancement for depressed, overweight/obese adolescents: Results of a pilot trial[J]. J Clin Child Adolesc Psychol, 2019, 48 (Suppl 1): S24- S33. |
| 10 | Bräutigam-Ewe M , Lydell M , Månsson J , et al. Dietary advice on prescription: Experiences with a weight reduction programme[J]. J Clin Nurs, 2017, 26 (5/6): 795- 804. |
| 11 |
Couch D , Han GS , Robinson P , et al. Men' s weight loss stories: How personal confession, responsibility and transformation work as social control[J]. Health (London), 2019, 23 (1): 76- 96.
doi: 10.1177/1363459317724855 |
| 12 |
Zhu N , Lu HJ , Chang L . Peer popularity and self-discipline as protective factors against depressive symptoms in Chinese adolescents: Do boys and girls benefit equally[J]. Psych J, 2024, 13 (1): 66- 78.
doi: 10.1002/pchj.708 |
| 13 |
Tsur AM , Akavian I , Landau R , et al. Adolescent body mass index and early chronic kidney disease in young adulthood[J]. JAMA Pediatr, 2024, 178 (2): 142- 150.
doi: 10.1001/jamapediatrics.2023.5420 |
| 14 |
Twig G , Yaniv G , Levine H , et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood[J]. N Engl J Med, 2016, 374 (25): 2430- 2440.
doi: 10.1056/NEJMoa1503840 |
| 15 | Xie Y , Hu J . An introduction to the China family panel studies (CFPS)[J]. Chin Sociol Rev, 2014, 47 (1): 3- 29. |
| 16 | 中华人民共和国国家卫生和计划生育委员会. WS/T 456—2014学龄儿童青少年营养不良筛查[S]. 北京: 中国标准出版社, 2014. |
| 17 | 中华人民共和国国家卫生和计划生育委员会. WS/T 586—2018学龄儿童青少年超重与肥胖筛查[S]. 北京: 中国标准出版社, 2018. |
| 18 | 章婕, 吴振云, 方格, 等. 流调中心抑郁量表全国城市常模的建立[J]. 中国心理卫生杂志, 2010, 24 (2): 139- 143. |
| 19 |
Lennon H , Kelly S , Sperrin M , et al. Framework to construct and interpret latent class trajectory modelling[J]. BMJ Open, 2018, 8 (7): e020683.
doi: 10.1136/bmjopen-2017-020683 |
| 20 | World Health Organization. Growth reference data for 5-19 years[EB/OL]. [2024-01-15]. http://www.who.int/growthref/en/. |
| 21 | World Health Organization. BMI-for-age (5-19 years). Growth reference 5-19 years[EB/OL]. [2024-01-15]. http://www.who.int/growthref/who2007_bmi_for_age/en/. |
| 22 |
Kemps E , Goossens L , Petersen J , et al. Evidence for enhancing childhood obesity treatment from a dual-process perspective: A systematic literature review[J]. Clin Psychol Rev, 2020, 77, 101840.
doi: 10.1016/j.cpr.2020.101840 |
| 23 |
Pines AR , Sacchet MD , Kullar M , et al. Multi-unit relations among neural, self-report, and behavioral correlates of emotion regulation in comorbid depression and obesity[J]. Sci Rep, 2018, 8 (1): 14032.
doi: 10.1038/s41598-018-32394-2 |
| 24 |
Rios-Leyvraz M , Ortega N , Chiolero A . Reliability of self-reported height and weight in children: A school-based cross-sectional study and a review[J]. Nutrients, 2022, 15 (1): 75.
doi: 10.3390/nu15010075 |
| 25 |
Field AE , Aneja P , Rosner B . The validity of self-reported weight change among adolescents and young adults[J]. Obesity (Silver Spring), 2007, 15 (9): 2357- 2364.
doi: 10.1038/oby.2007.279 |
| [1] | Tianjiao HOU,Zhibo ZHOU,Zhuqing WANG,Mengying WANG,Siyue WANG,Hexiang PENG,Huangda GUO,Yixin LI,Hanyu ZHANG,Xueying QIN,Yiqun WU,Hongchen ZHENG,Jing LI,Tao WU,Hongping ZHU. Gene-gene/gene-environment interaction of transforming growth factor-β signaling pathway and the risk of non-syndromic oral clefts [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 384-389. |
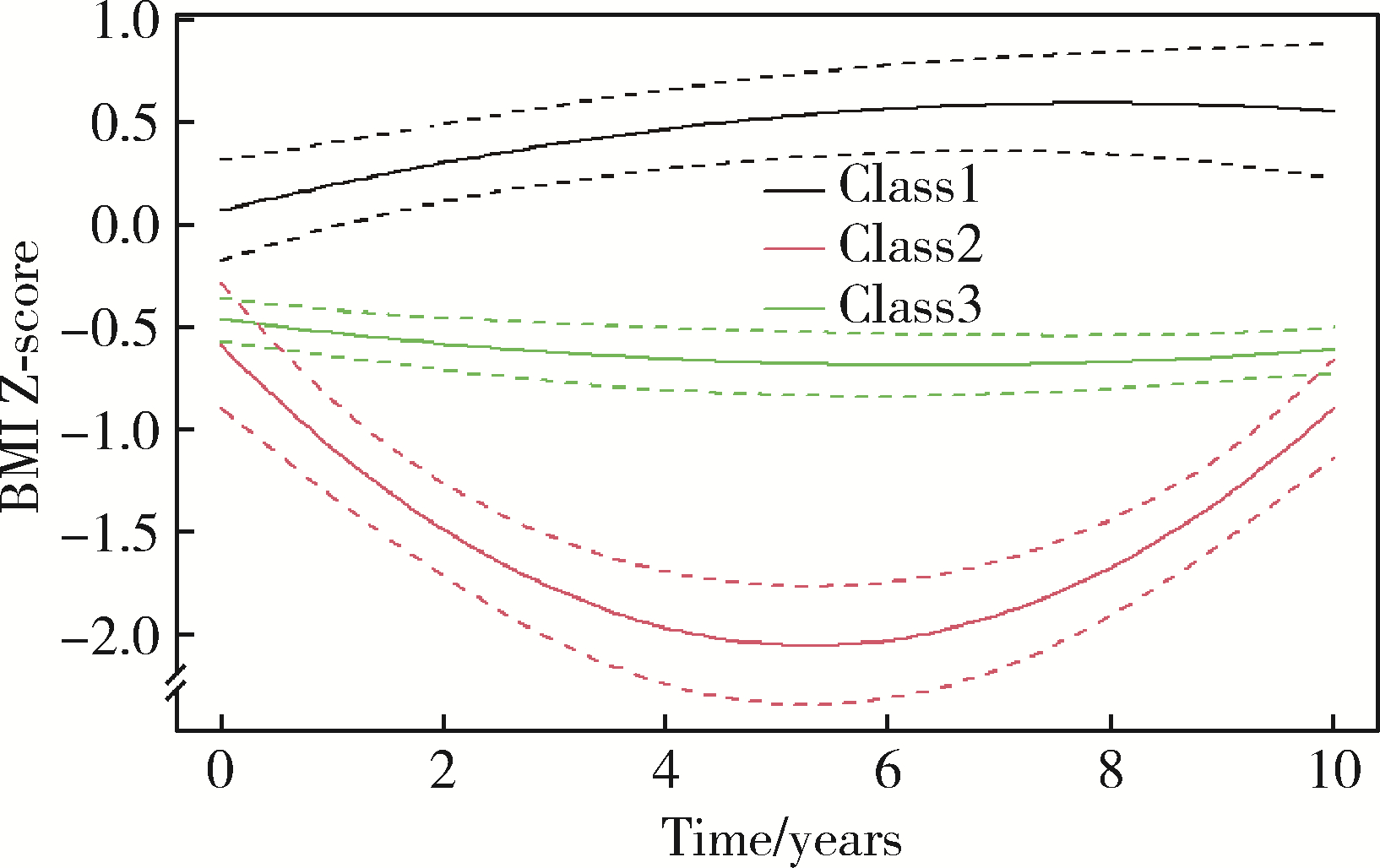
| [2] | Zhihan YUE,Na HAN,Zheng BAO,Jinlang LYU,Tianyi ZHOU,Yuelong JI,Hui WANG,Jue LIU,Haijun WANG. A prospective cohort study of association between early childhood body mass index trajectories and the risk of overweight [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 390-396. |
| [3] | Yifan WU,Yingxiang YU,Lan XIE,Zhida ZHANG,Cuiqing CHANG. Characteristics of resting energy expenditure and evaluation of prediction formulas in young men with different body mass indexes [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 247-252. |
| [4] | Chu-yun CHEN,Peng-fei SUN,Jing ZHAO,Jia JIA,Fang-fang FAN,Chun-yan WANG,Jian-ping LI,Yi-meng JIANG,Yong HUO,Yan ZHANG. Related factors of endogenous erythropoietin and its association with 10-year risks of cardiovascular disease in a community-based Chinese study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1068-1073. |
| [5] | Chun-su ZHU,Zhi-wei LIAN,Yi-min CUI. Association between depression and chronic diseases among middle-aged and older Chinese adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 606-611. |
| [6] | Ting WANG,Qiao-sheng LI,Hao-ran LIU,Wei-yan JIAN. Urban-rural differentials in the relationship between personality traits and changes in depressive symptoms [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 385-391. |
| [7] | Jia-jia DANG,Shan CAI,Pan-liang ZHONG,Ya-qi WANG,Yun-fei LIU,Di SHI,Zi-yue CHEN,Yi-hang ZHANG,Pei-jin HU,Jing LI,Jun MA,Yi SONG. Association of outdoor artificial light at night exposure with overweight and obesity among children and adolescents aged 9 to 18 years in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 421-428. |
| [8] | Jing CHEN,Wu-cai XIAO,Rui SHAN,Jie-yun SONG,Zheng LIU. Influence of rs2587552 polymorphism of DRD2 gene on the effect of a childhood obesity intervention: A prospective, parallel-group controlled trial [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 436-441. |
| [9] | Zi-wei ZHANG,Yu-meng HUA,Ai-ping LIU. Joint association of depression symptoms and 10-year risk of ischemic cardiovascular disease with the cardiovascular disease in middle-aged and elderly people in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 465-470. |
| [10] | Tao MA,Yan-hui LI,Man-man CHEN,Ying MA,Di GAO,Li CHEN,Qi MA,Yi ZHANG,Jie-yu LIU,Xin-xin WANG,Yan-hui DONG,Jun MA. Associations between early onset of puberty and obesity types in children: Based on both the cross-sectional study and cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 961-970. |
| [11] | GUO Zi-ning, LIANG Zhi-sheng, ZHOU Yi, ZHANG Na, HUANG Jie. Genetic study of cardiovascular disease subtypes defined by International Classification of Diseases [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 453-459. |
| [12] | Meng-ying WANG,Wen-yong LI,Ren ZHOU,Si-yue WANG,Dong-jing LIU,Hong-chen ZHENG,Jing LI,Nan LI,Zhi-bo ZHOU,Hong-ping ZHU,Tao WU,Yong-hua HU. Evaluating the effect of WNT pathway genes considering interactions on the risk of non-syndromic oral clefts among Chinese populations [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 815-820. |
| [13] | Xiao-na NA,Zhu ZHU,Yang-yang CHEN,Dong-ping WANG,Hao-jie WANG,Yang SONG,Xiao-chuan MA,Pei-yu WANG,Ai-ping LIU. Associations of distribution of time spent in physical activity and sedentary behavior with obesity [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 486-491. |
| [14] | Xiao-yuan ZHANG,Cheng-cheng GUO,Ying-xiang YU,Lan XIE,Cui-qing CHANG. Establishment of high-fat diet-induced obesity and insulin resistance model in rats [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 557-563. |
| [15] | Cheng-cheng GUO,Xiao-yuan ZHANG,Ying-xiang YU,Lan XIE,Cui-qing CHANG. Effects of chlorogenic acid on glucose tolerance and its curve characteristics in high-fat diet-induced obesity rats [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 269-274. |
|
||