Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 557-563. doi: 10.19723/j.issn.1671-167X.2020.03.024
Previous Articles Next Articles
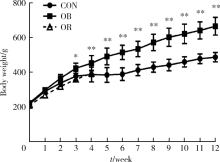
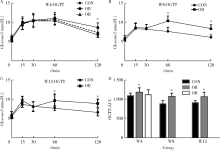
Establishment of high-fat diet-induced obesity and insulin resistance model in rats
Xiao-yuan ZHANG,Cheng-cheng GUO,Ying-xiang YU,Lan XIE,Cui-qing CHANG( )
)
- Institute of Sports Medicine, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R-332
| [1] | Rees DA, Alcolado JC. Animal models of diabetes mellitus[J]. Diabet Med, 2005,22(4):359-370. |
| [2] | Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications[J]. Nat Rev Endocrinol, 2013,9(1):13-27. |
| [3] | Chen D, Wang MW. Development and application of rodent models for type 2 diabetes[J]. Diabetes Obes Metab, 2005,7(4):307-317. |
| [4] | Panchal SK, Brown L. Rodent models for metabolic syndrome research[J]. J Biomed Biotechnol, 2011,2011:351982. doi: 10.1155/2011/351982. |
| [5] | 张小华, 张汝学, 贾正平, 等. 高脂饮食和地塞米松联合诱导胰岛素抵抗大鼠模型[J]. 中国实验动物学报, 2008,16(5):325-329. |
| [6] | Chen SH, Zhuang XH, Liu YT, et al. Expression and significance of lipin1 and AMPKalpha in hepatic insulin resistance in diet-induced insulin resistance rats[J]. Exp Clin Endocrinol Diabetes, 2012,120(2):84-88. |
| [7] |
Marques C, Meireles M, Norberto S, et al. High-fat diet-induced obesity rat model: a comparison between Wistar and Sprague-Dawley rat[J]. Adipocyte, 2016,5(1):11-21.
doi: 10.1080/21623945.2015.1061723 pmid: 27144092 |
| [8] |
Davidson EP, Coppey LJ, Dake B, et al. Effect of treatment of Sprague-Dawley rats with AVE7688, enalapril, or candoxatril on diet-induced obesity [J]. J Obes, 2011, 2011: pii: 686952. doi: 10.1155/2011/686952.
pmid: 20847891 |
| [9] |
Reed MJ, Meszaros K, Entes LJ, et al. A new rat model of type 2 diabetes: the fat-fed, streptozotocin-treated rat[J]. Metabolism, 2000,49(11):1390-1394.
doi: 10.1053/meta.2000.17721 pmid: 11092499 |
| [10] | 王智华, 宋光耀, 刘晶, 等. 高脂饮食诱发胰岛素抵抗大鼠模型的建立与评价[J]. 现代中西医结合杂志, 2012,21(3):244-245. |
| [11] | Svegliati-Baroni G, Candelaresi C, Saccomanno S, et al. A model of insulin resistance and nonalcoholic steatohepatitis in rats: role of peroxisome proliferator-activated receptor-alpha and n-3 polyunsa-turated fatty acid treatment on liver injury[J]. Am J Pathol, 2006,169(3):846-860. |
| [12] | Hariri N, Thibault L. High-fat diet-induced obesity in animal models[J]. Nutr Res Rev, 2010,23(2):270-299. |
| [13] | 那立欣, 赵丹, 宁华, 等. 减肥功能实验动物模型的改良[J]. 卫生研究, 2010,39(2):162-164. |
| [14] |
Kleiner DE Brunt EM van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease[J]. Hepatology, 2005,41(6):1313-1321.
pmid: 15915461 |
| [15] |
Levin BE, Dunn-Meynell AA, Balkan B, et al. Selective breeding for diet-induced obesity and resistance in Sprague-Dawley rats[J]. Am J Physiol, 1997,273(2 Pt 2):R725-R730.
doi: 10.1152/ajpregu.1997.273.2.R725 pmid: 9277561 |
| [16] |
Cheng HS, Ton SH, Phang S, et al. Increased susceptibility of post-weaning rats on high-fat diet to metabolic syndrome[J]. J Adv Res, 2017,8(6):743-752.
pmid: 29062573 |
| [17] | Giles ED, Jackman MR, Maclean PS. Modeling diet-induced obesity with obesity-prone rats: Implications for studies in females[J]. Front Nutr, 2016,3(3):50. |
| [18] | Ghibaudi L, Cook J, Farley C, et al. Fat intake affects adiposity, comorbidity factors, and energy metabolism of sprague-dawley rats[J]. Obes Res, 2002,10(9):956-963. |
| [19] |
Chalkley SM, Hettiarachchi M, Chisholm DJ, et al. Long-term high-fat feeding leads to severe insulin resistance but not diabetes in Wistar rats[J]. Am J Physiol Endocrinol Metab, 2002,282(6):E1231-E1238.
pmid: 12006352 |
| [20] | Malvi P, Piprode V, Chaube B, et al. High fat diet promotes achievement of peak bone mass in young rats[J]. Biochem Biophys Res Commun, 2014,455(1-2):133-138. |
| [21] | Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease[J]. J Clin Invest, 2011,121(6):2111-2117. |
| [22] |
Karalis KP, Giannogonas P, Kodela E, et al. Mechanisms of obesity and related pathology: Linking immune responses to metabolic stress[J]. FEBS J, 2009,276(20):5747-5754.
pmid: 19754872 |
| [23] | Hotamisligil GS. Inflammatory pathways and insulin action[J]. Int J Obes Relat Metab Disord, 2003,27(Suppl 3):S53-55. |
| [24] | Shapiro H, Lutaty A, Ariel A. Macrophages, meta-inflammation, and immuno-metabolism[J]. Scientific World J, 2011,11(6):2509-2529. |
| [1] | Jiang JIN, Xue CHEN, Yan ZHAO, Jun JIA, Jianzhong ZHANG. The role and its regulatory significance of interleukin-25 in ovalbumin induced atopic dermatitis of mice [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 756-762. |
| [2] | Hanwei KE, Qi WANG, Kexin XU. Optimization study of an animal model for interstitial cystitis/bladder pain syndrome based on the dose effect of cyclophosphamide [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 908-912. |
| [3] | Shengqi ZHENG,Tianchi HUA,Guicao YIN,Wei ZHANG,Ye YAO,Yifan LI. Association between the triglyceride-glucose index and the incidence of nephrolithiasis in male individuals [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 610-616. |
| [4] | Jing CHEN,Rui SHAN,Wucai XIAO,Xiaorui ZHANG,Zheng LIU. Association between self-control and co-occurrence of depressive symptoms and overweight or obesity during adolescence and early adulthood: A ten-year prospective cohort study based on national surveys [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 397-402. |
| [5] | Chu-yun CHEN,Peng-fei SUN,Jing ZHAO,Jia JIA,Fang-fang FAN,Chun-yan WANG,Jian-ping LI,Yi-meng JIANG,Yong HUO,Yan ZHANG. Related factors of endogenous erythropoietin and its association with 10-year risks of cardiovascular disease in a community-based Chinese study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1068-1073. |
| [6] | Jia-jia DANG,Shan CAI,Pan-liang ZHONG,Ya-qi WANG,Yun-fei LIU,Di SHI,Zi-yue CHEN,Yi-hang ZHANG,Pei-jin HU,Jing LI,Jun MA,Yi SONG. Association of outdoor artificial light at night exposure with overweight and obesity among children and adolescents aged 9 to 18 years in China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 421-428. |
| [7] | Jing CHEN,Wu-cai XIAO,Rui SHAN,Jie-yun SONG,Zheng LIU. Influence of rs2587552 polymorphism of DRD2 gene on the effect of a childhood obesity intervention: A prospective, parallel-group controlled trial [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 436-441. |
| [8] | Ting-ting YUAN,Shen LI,Yan WU,Hai-tao WU. Establishment and behavioral evaluation of a mouse model of long-term free-choice alcohol drinking [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 315-323. |
| [9] | Zi-xiang GAO,Yong WANG,Ao-nan WEN,Yu-jia ZHU,Qing-zhao QIN,Yun ZHANG,Jing WANG,Yi-jiao ZHAO. Automatic determination of mandibular landmarks based on three-dimensional mandibular average model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 174-180. |
| [10] | Ling-wei MENG,Xue LI,Sheng-han GAO,Yue LI,Rui-tao CAO,Yi ZHANG,Shao-xia PAN. Comparison of three methods for establishing rat peri-implantitis model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 22-29. |
| [11] | Tao MA,Yan-hui LI,Man-man CHEN,Ying MA,Di GAO,Li CHEN,Qi MA,Yi ZHANG,Jie-yu LIU,Xin-xin WANG,Yan-hui DONG,Jun MA. Associations between early onset of puberty and obesity types in children: Based on both the cross-sectional study and cohort study [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 961-970. |
| [12] | Lin ZHU,Wei-yu ZHANG,Ke-xin XU. Urodynamic and histological evaluation of cyclophosphamide-induced bladder pain syndrome in SD rats [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 735-740. |
| [13] | Yu-han DENG,Yong JIANG,Zi-yao WANG,Shuang LIU,Yu-xin WANG,Bao-hua LIU. Long short-term memory and Logistic regression for mortality risk prediction of intensive care unit patients with stroke [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 458-467. |
| [14] | Jia-he ZHANG,Jia-qi SHI,Zhang-jian CHEN,Guang JIA. Effects of nano titanium dioxide on gut microbiota based on human digestive tract microecology simulation system in vitro [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 468-476. |
| [15] | LIU Si-min,ZHAO Yi-jiao,WANG Xiao-yan,WANG Zu-hua. In vitro evaluation of positioning accuracy of trephine bur at different depths by dynamic navigation [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 146-152. |
|
||