Journal of Peking University (Health Sciences) ›› 2024, Vol. 56 ›› Issue (4): 575-581. doi: 10.19723/j.issn.1671-167X.2024.04.005
Previous Articles Next Articles
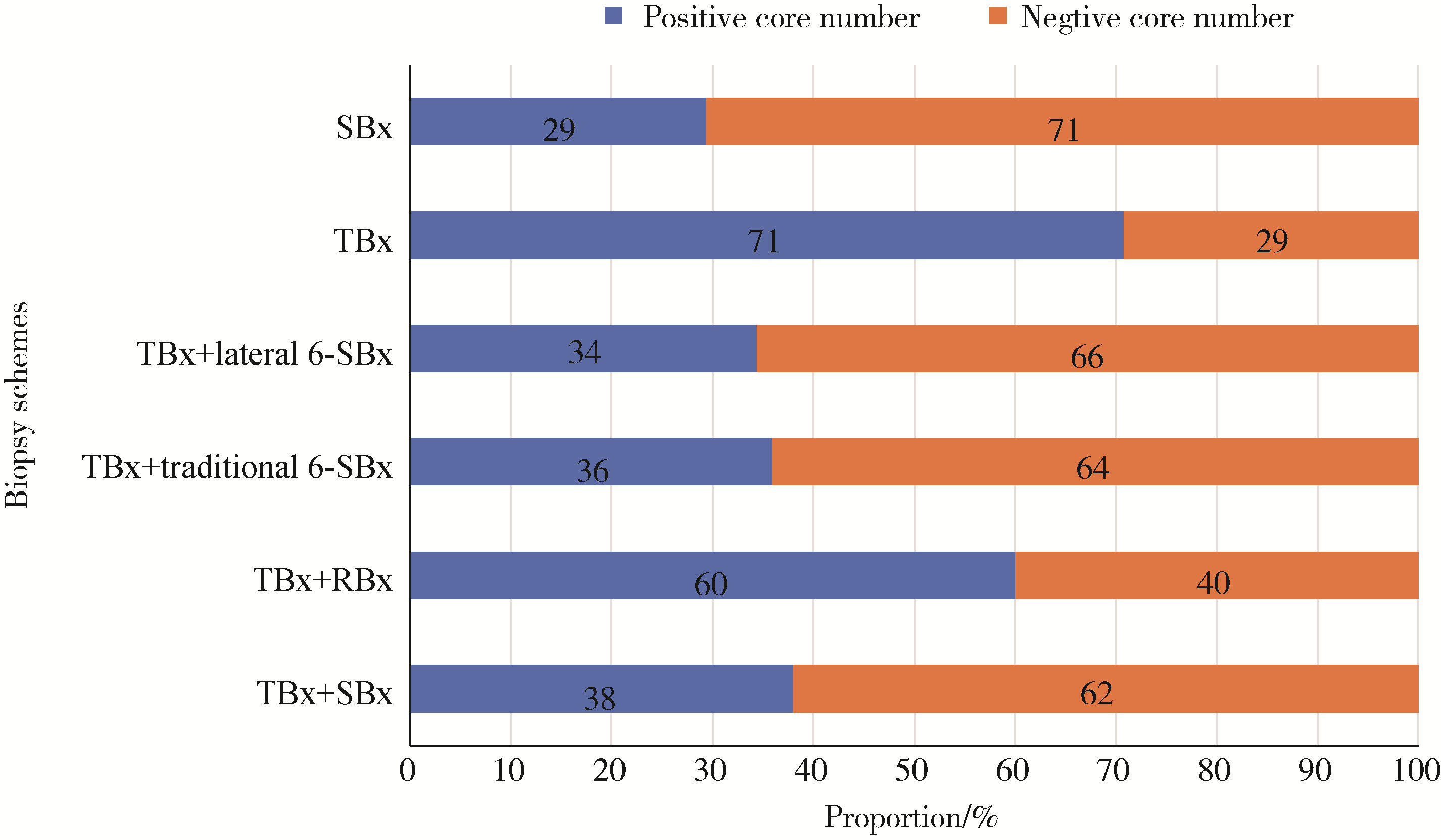
Diagnostic efficacy of targeted biopsy combined with regional systematic biopsy in prostate cancer in patients with PI-RADS 4-5
Kaifeng YAO,Mingjian RUAN,Derun LI,Yuxuan TIAN,Yuke CHEN,Yu FAN,Yi LIU*( )
)
- Department of Urology, Peking University First Hospital; Institution of Urology, Peking University; Beijing Key Laboratory of Urogenital Diseases (Male) Molecular Diagnosis and Treatment Center; National Urological Cancer Center, Beijing 100034, China
CLC Number:
- R737.25
| 1 | 黄健, 王建业, 孔垂泽. 中国泌尿外科和男科疾病诊断治疗指南(2019版)[M]. 北京: 科学出版社, 2020: 115- 131. |
| 2 |
Turkbey B , Rosenkrantz AB , Haider MA , et al. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2[J]. Eur Urol, 2019, 76 (3): 340- 351.
doi: 10.1016/j.eururo.2019.02.033 |
| 3 |
Mottet N , van den Bergh RCN , Briers E , et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer: 2020 update. Part 1: Screening, diagnosis, and local treatment with curative intent[J]. Eur Urol, 2021, 79 (2): 243- 262.
doi: 10.1016/j.eururo.2020.09.042 |
| 4 |
Hagens MJ , Noordzij MA , Mazel JW , et al. An magnetic resonance imaging-directed targeted-plus-perilesional biopsy approach for prostate cancer diagnosis: "Less is more"[J]. Eur Urol Open Sci, 2022, 43, 68- 73.
doi: 10.1016/j.euros.2022.07.006 |
| 5 | Freifeld Y , Xi Y , Passoni N , et al. Optimal sampling scheme in men with abnormal multiparametric MRI undergoing MRI-TRUS fusion prostate biopsy[J]. Urol Oncol, 2018, 37 (1): 57- 62. |
| 6 |
Raman AG , Sarma KV , Raman SS , et al. Optimizing spatial biopsy sampling for the detection of prostate cancer[J]. J Urol, 2021, 206 (3): 595- 603.
doi: 10.1097/JU.0000000000001832 |
| 7 |
Hagens MJ , Salamanca MF , Padhani AR , et al. Diagnostic performance of a magnetic resonance imaging-directed targeted plus regional biopsy approach in prostate cancer diagnosis: A systematic review and meta-analysis[J]. Euro Urol Open Sci, 2022, 40, 95- 103.
doi: 10.1016/j.euros.2022.04.001 |
| 8 |
Caverly TJ , Hayward RA , Reamer E , et al. Presentation of benefits and harms in US cancer screening and prevention guidelines: Systematic review[J]. J Natl Cancer Inst, 2016, 108 (6): djv436.
doi: 10.1093/jnci/djv436 |
| 9 |
何为, 全晶, 张琦, 等. 影像融合靶向穿刺、系统穿刺以及联合穿刺诊断前列腺癌的差异[J]. 中华泌尿外科杂志, 2021, 42 (8): 581- 585.
doi: 10.3760/cma.j.cn112330-20210628-00346 |
| 10 |
刘禹, 高杰, 汪维, 等. 靶向穿刺与靶向联合系统穿刺对前列腺PI-RADS评分4~5分患者的诊断效能比较[J]. 中华泌尿外科杂志, 2021, 42 (3): 192- 196.
doi: 10.3760/cma.j.cn112330-20200722-00553 |
| 11 |
Kasivisvanathan V , Rannikko AS , Borghi M , et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis[J]. N Engl J Med, 2018, 378 (19): 1767- 1777.
doi: 10.1056/NEJMoa1801993 |
| 12 |
Rouvière O , Puech P , Renard-Penna R , et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): A prospective, multicentre, paired diagnostic study[J]. Lancet Oncol, 2019, 20 (1): 100- 109.
doi: 10.1016/S1470-2045(18)30569-2 |
| 13 |
Schoots IG , Roobol MJ , Nieboer D , et al. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard trans-rectal ultrasound-guided biopsy: A systematic review and meta-analysis[J]. Eur Urol, 2015, 68 (3): 438- 450.
doi: 10.1016/j.eururo.2014.11.037 |
| 14 |
梁玲辉, 承逸飞, 夏炜, 等. MRI-TRUS融合靶向前列腺活检中的靶区针数最优化研究[J]. 中华泌尿外科杂志, 2022, 43 (11): 850- 854.
doi: 10.3760/cma.j.cn112330-20210108-00012 |
| 15 |
涂祥, 熊性宇, 张驰宸, 等. 6针系统穿刺联合3针磁共振引导靶向穿刺对前列腺癌的检出效果[J]. 中华泌尿外科杂志, 2022, 43 (12): 914- 919.
doi: 10.3760/cma.j.cn112330-20211005-00526 |
| 16 |
Bryk DJ , Llukani E , Taneja S , et al. The role of ipsilateral and contralateral transrectal ultrasound-guided systematic prostate biopsy in men with unilateral magnetic resonance imaging lesion undergoing magnetic resonance imaging-ultrasound fusion-targeted prostate biopsy[J]. Urology, 2017, 102, 178- 182.
doi: 10.1016/j.urology.2016.11.017 |
| 17 | 刘毅, 袁昌巍, 吴静云, 等. 靶向穿刺+6针系统穿刺对PI-RADS 5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2023, 55 (5): 812- 817. |
| 18 | Cornford P, Tilki D, van den Bergh RCN, et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on prostate cancer: Diagnostic evaluation [R/OL]. (2024-04) [2024-05-06]. https://uroweb.org/guidelines/prostate-cancer/chapter/diagnostic-evaluation. |
| 19 |
Klingebiel M , Arsov C , Ullrich T , et al. Reasons for missing cli-nically significant prostate cancer by targeted magnetic resonance imaging/ultrasound fusion-guided biopsy[J]. Eur J Radiol, 2021, 137, 109587.
doi: 10.1016/j.ejrad.2021.109587 |
| 20 |
Feuer Z , Meng X , Rosenkrantz AB , et al. Application of the PRECISION trial biopsy strategy to a contemporary magnetic resonance imaging-targeted biopsy cohort: How many clinically significant prostate cancers are missed?[J]. J Urol, 2021, 205 (3): 740- 747.
doi: 10.1097/JU.0000000000001406 |
| 21 | Le Nobin J , Orczyk C , Deng FM , et al. Prostate tumour volumes: Evaluation of the agreement between magnetic resonance imaging and histology using novel co-registration software[J]. BJU Int, 2014, 114 (6b): E105- E112. |
| 22 | Franklin A , Gianduzzo T , Yaxley J , et al. Use of a trizonal schema to assess targeting accuracy in prostatic fusion biopsy[J]. BJU Int, 2020, 126 (Suppl 1): 6- 11. |
| 23 |
Aslim EJ , Law YXT , Fook-Chong SMC , et al. Defining prostate cancer size and treatment margin for focal therapy: Does intra-lesional heterogeneity impact the performance of multiparametric MRI?[J]. BJU Int, 2021, 128 (2): 178- 186.
doi: 10.1111/bju.15355 |
| 24 |
Priester A , Natarajan S , Khoshnoodi P , et al. Magnetic resonance imaging underestimation of prostate cancer geometry: Use of patient specific molds to correlate images with whole mount pathology[J]. J Urol, 2017, 197 (2): 320- 326.
doi: 10.1016/j.juro.2016.07.084 |
| 25 |
Brisbane WG , Priester AM , Ballon J , et al. Targeted prostate biopsy: Umbra, penumbra, and value of perilesional sampling[J]. Eur Urol, 2022, 82 (3): 303- 310.
doi: 10.1016/j.eururo.2022.01.008 |
| 26 |
Novara G , Zattoni F , Zecchini G , et al. Role of targeted biopsy, perilesional biopsy, and random biopsy in prostate cancer diagnosis by mpMRI/transrectal ultrasonography fusion biopsy[J]. World J Urol, 2023, 41 (11): 3239- 3247.
doi: 10.1007/s00345-023-04382-3 |
| 27 | Jiang X, Chen M, Tian J, et al. Comparison of regional saturation biopsy, targeted biopsy, and systematic biopsy in patients with prostate-specific antigen levels of 4-20 ng/mL: A prospective, single-center, randomized controlled trial [J/OL]. Eur Urol Oncol, (2023-12-28) [2024-01-19]. doi: 10.1016/j.euo.2023.12.002. |
| [1] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [2] | Yuxuan TIAN,Mingjian RUAN,Yi LIU,Derun LI,Jingyun WU,Qi SHEN,Yu FAN,Jie JIN. Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 567-574. |
| [3] | Junyong OU,Kunming NI,Lulin MA,Guoliang WANG,Ye YAN,Bin YANG,Gengwu LI,Haodong SONG,Min LU,Jianfei YE,Shudong ZHANG. Prognostic factors of patients with muscle invasive bladder cancer with intermediate-to-high risk prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 582-588. |
| [4] | Yi LIU,Chang-wei YUAN,Jing-yun WU,Qi SHEN,Jiang-xi XIAO,Zheng ZHAO,Xiao-ying WANG,Xue-song LI,Zhi-song HE,Li-qun ZHOU. Diagnostic efficacy of prostate cancer using targeted biopsy with 6-core systematic biopsy for patients with PI-RADS 5 [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 812-817. |
| [5] | Chang-wei YUAN,De-run LI,Zhi-hua LI,Yi LIU,Gang-zhi SHAN,Xue-song LI,Li-qun ZHOU. Application of dynamic contrast enhanced status in multiparametric magnetic resonance imaging for prostatic cancer with PI-RADS 4 lesion [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 838-842. |
| [6] | Yan XIONG,Xin LI,Li LIANG,Dong LI,Li-min YAN,Xue-ying LI,Ji-ting DI,Ting LI. Evaluation of accuracy of pathological diagnosis based on thyroid core needle biopsy [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 234-242. |
| [7] | Dan-feng ZHENG,Jun-yu LI,Jia-xi LI,Ying-shuang ZHANG,Yan-feng ZHONG,Miao YU. Pathologic features of paraspinal muscle biopsies in patients with adolescent idiopathic scoliosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 283-291. |
| [8] | ZHOU Guang-ping,ZHOU Qian-yun,ZHU Ji-hong. A case report of TAFRO syndrome [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 814-817. |
| [9] | ZHANG Lei,LI Guo-liang,DANG Zong-hui, ,A yong,WU Ling-jie,LIU Li-jun. Analysis of bleeding risk in percutaneous renal biopsy in Tibet [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 298-301. |
| [10] | WANG Ying-chun,HUANG Yong-hui,CHANG Hong,YAO Wei,YAN Xiu-e,LI Ke,ZHANG Yao-peng,ZHENG Wei. Characteristics of benign and malignant lesions of ampullary polyps and the accuracy of forceps biopsy [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 204-209. |
| [11] | Yi LIU,Zhi-jian LIU,Qi SHEN,Jing-yun WU,Yu FAN,De-run LI,Wei YU,Zhi-song HE. A clinical analysis of 14 cases of prostatic stromal tumor of uncertain malignant potential [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 621-624. |
| [12] | Yi-chang HAO,Ye YAN,Fan ZHANG,Min QIU,Lang ZHOU,Ke LIU,Jian LU,Chun-lei XIAO,Yi HUANG,Cheng LIU,Lu-lin MA. Surgical strategy selection and experience summary of prostate cancer with positive single needle biopsy [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 625-631. |
| [13] | Ye YAN,Hai-zhui XIA,Xu-sheng LI,Wei HE,Xue-hua ZHU,Zhi-ying ZHANG,Chun-lei XIAO,Yu-qing LIU,Hua HUANG,Liang-hua HE,Jian LU. Application of U-shaped convolutional neural network in auto segmentation and reconstruction of 3D prostate model in laparoscopic prostatectomy navigation [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 596-601. |
| [14] | MAO Jia-ming, LIU De-feng,ZHAO Lian-ming,HONG Kai, ZHANG Li, MA Lu-lin, JIANG Hui, QIAO Jie. Effect of testicular puncture biopsy on the success rate of microdissection testicular sperm extraction for idiopathic non-obstructive azoospermia [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 613-616. |
| [15] | ZHANG Fan, XIAO Chun-lei, ZHANG Shu-dong, HUANG Yi, MA Lu-lin. Relationship between recovery of urinary continence after laparoscopic radical prostatectomy and prostatic volume and intravesical prostatic protursion length [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 621-625. |
|
||