北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (5): 870-874. doi: 10.19723/j.issn.1671-167X.2019.05.013
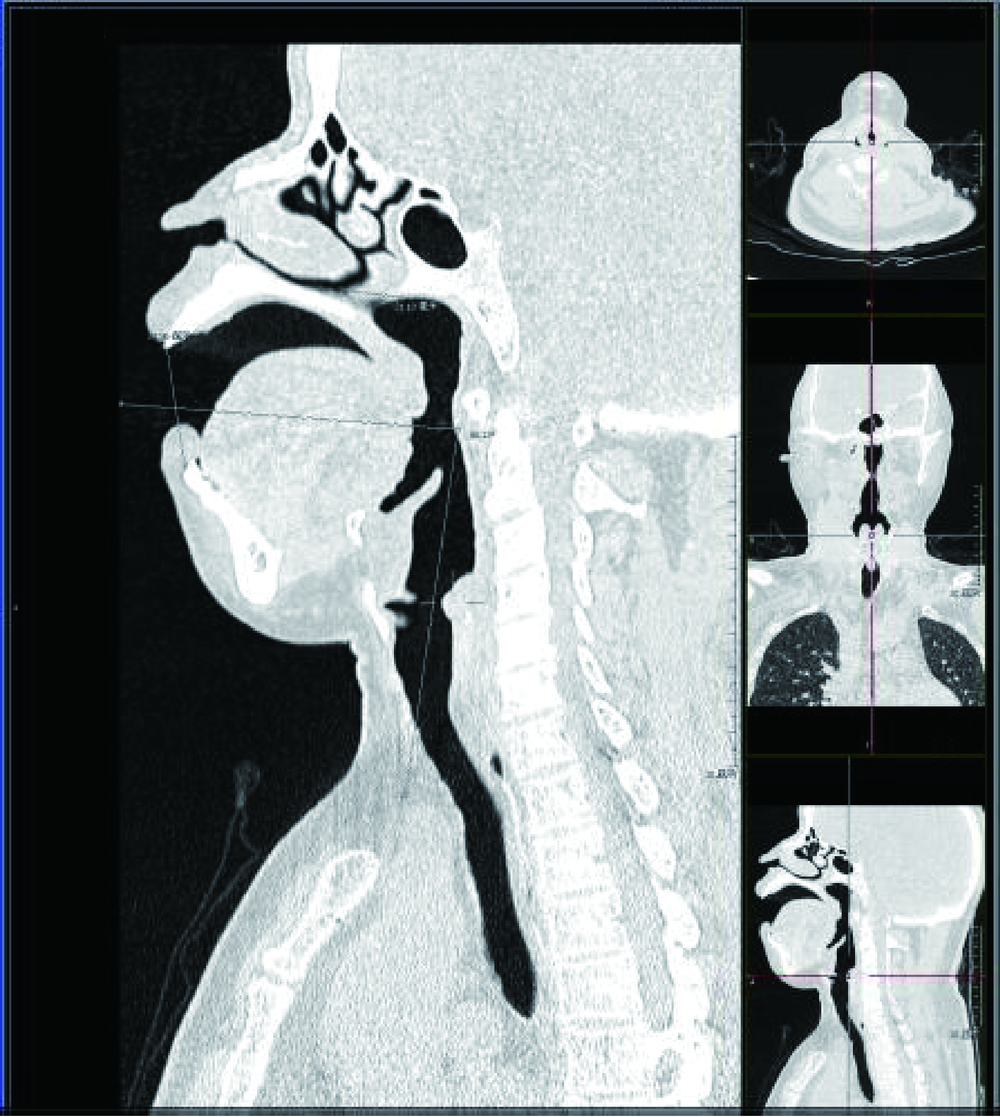
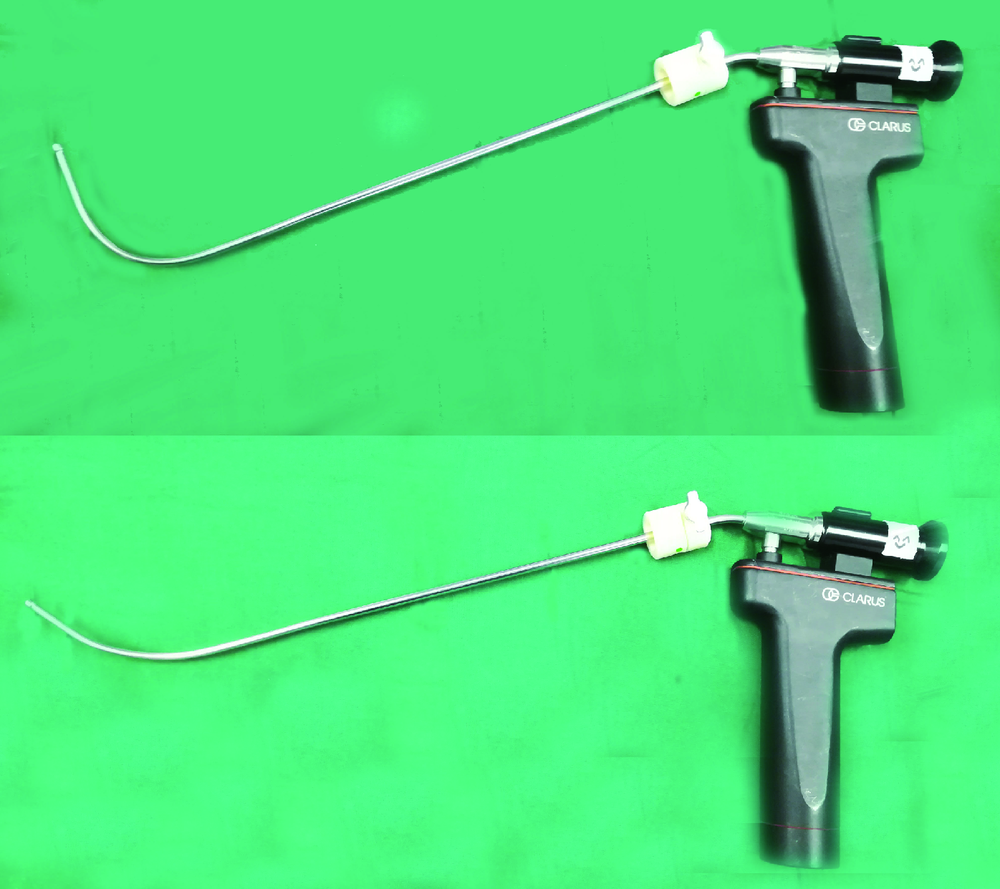
困难气道中运用CT 三维重建技术指导硬质纤维气管镜行气管插管
洪洪1,钱宇婷1,付磊2,王武2,李成辉1,尹毅青1,△( )
)
- 1. 中日友好医院 麻醉科, 北京 100029
2. 中日友好医院 影像科, 北京 100029
Study on the use of CT three-dimensional reconstruction technique for guiding tracheal intubation with rigid fiber bronchoscope in difficult airway
Hong HONG1,Yu-ting QIAN1,Lei FU2,Wu WANG2,Cheng-hui LI1,Yi-qing YIN1,△( )
)
- 1. Department of Anesthesiology,China-Japan Friendship Hopital,Beijing 100029, China
2. Department of Medical Image,China-Japan Friendship Hopital,Beijing 100029, China
摘要:
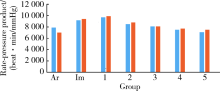
目的:研究困难气道中运用CT 三维重建技术指导硬质纤维气管镜行气管插管的效果。方法: 选择美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅰ~Ⅱ级、颈项强直、颈部外伤需制动或严重颈椎病颈椎固定的择期手术患者44例,随机分为两组,试验组(E组)24例和对照组(C组)20例。术前采集入组患者上气道CT 数据,依据患者的CT三维重建图像及由此获得的参数计算完成对Shikani硬质纤维气管镜(后简称硬质镜)管芯塑型,随机分组后,根据患者所在组别分别选用相应的硬质镜插管,E组采用根据患者CT三维重建图像计算的角度塑型后的硬质镜,C组采用原始角度硬质镜,并记录首次插管成功率及气管插管成功率,气管插管时间,入室(Tb)、插管后即刻(T0)、插管后5 min内(T1~T5)7个时间点血压、心率和脉搏氧饱和度,以及24 h内气管插管相关并发症。结果: 两组插管成功率均为100%,E组首次插管成功率为96%,C组首次插管成功率为70%,E组首次插管成功率高于C组。E组插管时间为(20.7±10.6) s,C组插管时间为(21.5±17.6) s,E组优于C组,但差异无统计学意义(P>0.05)。插管操作对血流动力学影响方面,E组心率血压乘积(rate-pressure product,RPP)在T0、T1、T2、T4、T5小于C组,但差异无统计学意义(P>0.05),两组气管插管相关并发症差异无统计学意义(P>0.05)。结论: 依据CT三维重建技术图像计算的角度对硬质镜管芯塑型,对提高颈椎固定困难气道患者的首次气管插管成功率具有一定指导意义。
中图分类号:
- R614
| [1] | Kheterpal S, Healy D, Aziz MF , et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group[J]. Anesthesiology, 2013,119(6):1360-1369. |
| [2] | Martini RP, Larson DM . Clinical evaluation and airway management for adults with cervical spine instability[J]. Anesthesiology Clin, 2015,33(2):315-327. |
| [3] | Yao YT, Jia NG, Li CH , et al. Comparison of endotracheal intubation with the Shikani Optical Stylet using the left molar approach and direct laryngoscopy[J]. Chin Med J (Engl), 2008,121(14):1324-1327. |
| [4] | Suppan L, Tramèr MR, Niquille M , et al. Alternative intubation techniques vs. Macintosh laryngoscopy in patients with cervical spine immobilization: Systematic review and meta-analysis of randomized controlled trials[J]. Br J Anaesth, 2016,116(1):27-36. |
| [5] | Turkstra TP, Pelz DM, Shaikh AA , et al. Cervical spine motion: a fluoroscopic comparison of Shikani Optical Stylet vs macintosh laryngoscope[J]. Can J Anaesth, 2007,54(6):441-447. |
| [6] | Rabab SS, Mahrous MD, Ahmed A , et al. The shikani optical stylet as an alternative to awake fiberoptic intubation in patients at risk of secondary cervical spine injury: a randomized controlled trial[J]. Neurosurg Anesthesiol, 2018,30(4):354-358. |
| [7] | 李月光, 张玉龙, 夏阂涛 . 光棒在困难气管插管中的应用[J]. 江苏医药, 2010,36(2):226-227. |
| [8] | 陈洁, 汪小海, 马正良 , 等. 非困难气道光棒气管插管折弯角度的研究[J]. 中华临床医师杂志, 2012,6(19):6110-6111. |
| [9] | 王冬青, 周永连, 张雷波 , 等. 光棒气管插管折弯方法的研究[J]. 临床麻醉学杂志, 2006,22(1):32-33. |
| [10] | Boedeker BH, Barak-Bernhagen MA, Miller DJ , et al. Improving rigid fiberoptic intubation: a comparison of the Bonfils Intubating Fiberscope? with a novel modification[J]. BMC Emerg Med, 2010,10:11. |
| [11] | Marson BA, Anderson E, Wilkes AR , et al. Bougie-related airway trauma: dangers of the hold-up sign[J]. Anaesthesia, 2014,69(3):219-223. |
| [12] | Nagamine Y, Kurahashi K . The use of three-dimensional computed tomography images for anticipated difficult intubation airway evaluation of a patient with treacher Collins syndrome[J]. Anesth Analg, 2007,105(3):626-628. |
| [13] | Lee HC, Kim MK, Kim YH , et al. Radiographic predictors of difficult laryngoscopy in acromegaly patients[J]. Neurosurg Anesthesiol, 2019,31(1):50-56. |
| [1] | 王军, 姚兰, 张宁, 索利斌, 李红培, 魏越, 查鹏, 梁正, 刘鲲鹏. 单侧胸椎旁阻滞对实施双腔气管插管患者血流动力学和意识水平的影响[J]. 北京大学学报(医学版), 2024, 56(5): 890-895. |
| [2] | 魏越,姚兰,陆希,王军,蔺莉,刘鲲鹏. 胃超声检查评估剖宫产产妇术前饮用碳水化合物后胃排空的效果[J]. 北京大学学报(医学版), 2023, 55(6): 1082-1087. |
| [3] | 魏越,陆希,张静,刘鲲鹏,王永军,姚兰. 术前2 h口服碳水化合物对妇科腹腔镜特殊体位手术患者胃容量及反流误吸风险的影响[J]. 北京大学学报(医学版), 2023, 55(5): 893-898. |
| [4] | 史成梅,周阳,杨宁,李正迁,陶一帆,邓莹,郭向阳. 丙泊酚用于无痛胃肠镜检查对患者术后精神活动的影响[J]. 北京大学学报(医学版), 2023, 55(2): 324-327. |
| [5] | 王洁初,姚优修,郭向阳. 严重低钾血症致麻醉后潜在致命性心律失常1例的术中管理[J]. 北京大学学报(医学版), 2023, 55(1): 186-189. |
| [6] | 康志宇,王磊磊,韩永正,郭向阳. 北京冬季奥林匹克运动会运动员手术的麻醉管理[J]. 北京大学学报(医学版), 2022, 54(4): 770-773. |
| [7] | 白鹏,怀伟,夏天,杨钟玮,郭向阳,周方. 气管插管和喉罩在手术室与滑雪场雪道建立人工气道时间的比较[J]. 北京大学学报(医学版), 2022, 54(1): 166-169. |
| [8] | 穆东亮,薛铖,安彬,王东信. 硬膜外阻滞与结直肠癌患者术后远期生存状态的关系:一项倾向性评分匹配的回顾性研究[J]. 北京大学学报(医学版), 2021, 53(6): 1152-1158. |
| [9] | 耿志宇,高为华,王东信. 全身麻醉气管插管患者术后声带运动不良的临床结局[J]. 北京大学学报(医学版), 2021, 53(2): 337-340. |
| [10] | 张庆芬,赵红,冯艺. 不同全身麻醉管理方式与早产儿眼底手术临床结局[J]. 北京大学学报(医学版), 2021, 53(1): 195-199. |
| [11] | 孟昭婷,穆东亮. 肺叶切除术中少尿与术后急性肾损伤的关系[J]. 北京大学学报(医学版), 2021, 53(1): 188-194. |
| [12] | 韩永正,井凤云,徐懋,郭向阳. 颈椎脊索瘤行肿瘤切除术的麻醉管理1例[J]. 北京大学学报(医学版), 2019, 51(5): 981-983. |
| [13] | 刘鲲鹏,王宝宁,申琰琰,李卫霞,李昭,姚兰. 胸部硬膜外给予利多卡因对双腔气管插管患者血流动力学和唤醒水平的影响[J]. 北京大学学报(医学版), 2019, 51(4): 742-747. |
| [14] | 邓莹,李岩,姚瑶,冯丹丹,徐懋. 颈5-6神经根阻滞技术用于肩关节镜术后镇痛的随机对照研究[J]. 北京大学学报(医学版), 2019, 51(1): 177-181. |
| [15] | 程小娥,彭慧浈,户雪雪,冯小金,马龙先,蒋昌宇,柳涛. 米诺环素抑制甲醛炎性痛及机制[J]. 北京大学学报(医学版), 2018, 50(5): 797-804. |
|
||