北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (6): 1140-1145. doi: 10.19723/j.issn.1671-167X.2020.06.026
慢性多灶性骨髓炎1例及文献回顾
- 1. 新疆医科大学第一附属医院风湿免疫科,乌鲁木齐 8300542
2. 北京大学第三医院风湿免疫科,北京 100191
Chronic multifocal osteomyelitis: A case report and literature review
Yong-wei HU1,Rui LIU2,△( ),Li LUO1,△(
),Li LUO1,△( )
)
- 1. Department of Rheumatology, the First Affiliated Hospital of Xinjiang Medical University, Urumchi 8300542, China
2. Department of Rheumatology, Peking University Third Hospital, Beijing 100191, China
摘要:
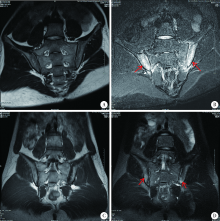
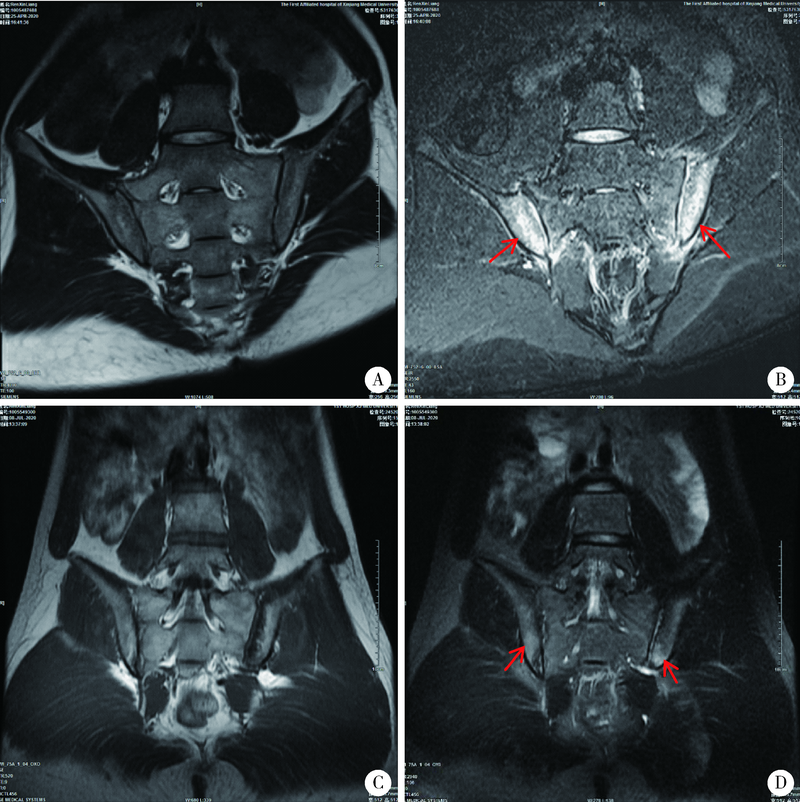
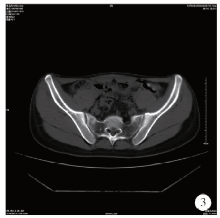
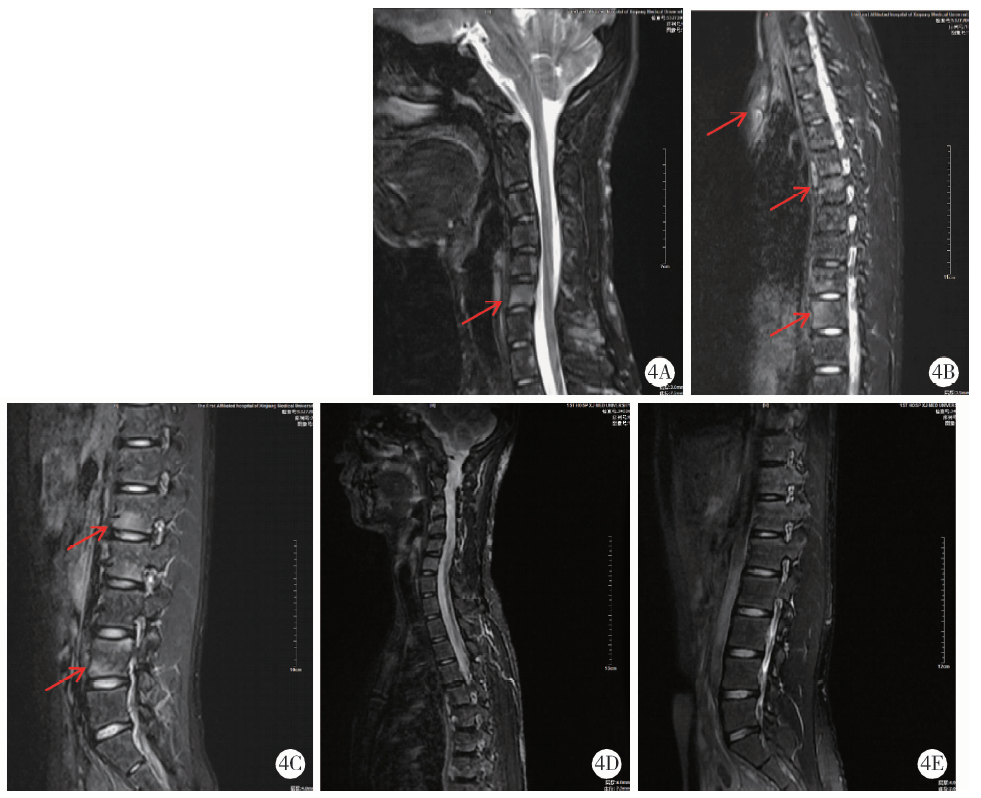
分析1例慢性多灶性骨髓炎病例的临床表现、血清学及影像学检查、诊断依据、治疗方案、出院后随访评估等,了解慢性复发性多灶性骨髓炎的发病机制、诊断、鉴别诊断、治疗,并进一步了解自身炎症性骨病的特点。本例患者青少年起病,伴有严重皮损,有进行性加重的脊柱关节疼痛,结合临床表现及辅助检查,符合慢性多灶性骨髓炎的诊断。经过抗炎、止痛效果不佳,后换用肿瘤坏死因子α(tumor necrosis factor α,TNF-α)抑制剂后疼痛缓解,炎症指标恢复正常,皮疹及影像学检查明显改善。慢性复发性多灶性骨髓炎属于自身炎症性骨病中多基因疾病的一种,又称慢性非细菌性骨髓炎,是一种罕见的非感染性炎性疾病,可引起多灶性溶骨性病变,以周期性加重和缓解为特征。该病发病率低,发病机制不清楚,可能与促炎及抗炎失衡有关,诊断无特异性指标及统一的诊断标准,常易与代谢性骨病、感染、肿瘤等疾病相混淆,临床表现为骨痛、发热、皮疹、骨折等,实验室检查可见炎症指标明显增高,影像学检查有溶骨性或硬化性改变,MRI在识别骨病变和组织水肿上更有效,而且比骨发射型计算机断层扫描(emission computed tomography,ECT)更准确。治疗用药方面,多数开始使用非甾体类抗炎药,但易复发并出现新发病灶,还可选择其他治疗方案,如糖皮质激素、TNF-α抑制剂及双磷酸盐、甲氨蝶呤等改善病情的抗风湿药物(disease-modifying anti-rheumatic drugs,DMARDs)。对慢性多灶性骨髓炎的早期诊断和治疗可以预防和减少疾病的并发症,改善患者预后。
中图分类号:
- R681.2
| [1] |
Master SL, Simon A, Aksentijevich I, et al. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease[J]. Annu Rev Immunol, 2009,27:621-668.
doi: 10.1146/annurev.immunol.25.022106.141627 pmid: 19302049 |
| [2] | 余可谊, 沈敏. 自身炎症性骨病[J]. 中华医学杂志, 2016,96(15):1230-1232. |
| [3] |
Jansson A, Renner ED, Ramer J, et al. Classification of nonbacterial osteitis: rttrospective study of clinical, immunological and genetic in 89 patients[J]. Rheumatology, 2007,46(1):154-160.
doi: 10.1093/rheumatology/kel190 pmid: 16782988 |
| [4] |
Sciannro R, Insalaco A, Bracci LL, et al. Deregulation of the IL-1β axis in chronic recurrent multifocal osteomyelitis[J]. Pediatr Rheumatol Online J, 2014,7(17):12-30.
doi: 10.1186/1546-0096-7-12 |
| [5] | 吴凤岐. 再认识全身型幼年特发性关节炎[J]. 中华实用儿科临床杂志, 2014,11(29):1607-1610. |
| [6] |
Greenwood S, Leone A, Cassar-Pullicino VN. SAPHO and recurrent multifocal osteomyelitis[J]. Radiol Clin North Am, 2017,55(5):1035-1053.
pmid: 28774447 |
| [7] |
Sato H, Wada Y, Hasegawa E, et al. Adult-onset chronic recurrent multifocal osteomyelitis with high intensity of muscles detected by magnetic resonance imaging, successfully controlled with tocilizumab[J]. Intern Med, 2017,56(17):2353-2360.
doi: 10.2169/internalmedicine.8473-16 pmid: 28794369 |
| [8] |
Earwaker JW, Cotten A. SAPHO: Syndrome or concept? Imaging findings[J]. Skeletal Radiol, 2003,32(6):311-327.
doi: 10.1007/s00256-003-0629-x pmid: 12719925 |
| [9] | Inoue K, Yamaguchi T, Ozawa H, et al. Diagnosing active inflammation in the SAPHO syndrome using 18FDG-PET/CT in suspected metastatic vertebral bone tumors[J]. Ann Nucl Med, 2007,2l(8):477-480. |
| [10] |
Takeuchi K, Matsusita M, Takagishi K. A case of SAPHO (synovitis-acne-pustulosis-hyperostosis-osteomyelitis) syndrome in which [18F]fluorodeoxyglucose positron emission tomography was useful for differentiating from multiple metastatic bone tumors[J]. Mod Rheumatol, 2007,17(1):67-7l.
doi: 10.1007/s10165-006-0536-9 |
| [11] |
Morbach H, Hedrich CM, Beer M, et al. Autoinflammatory bone disorders[J]. Clin Immunol, 2013,147(3):185-196.
doi: 10.1016/j.clim.2012.12.012 |
| [12] |
Sharma M, ferguson PJ. Autoinflammatory bone disorders: update on immunologic abnormalities and clues about possible triggers[J]. Curr Opin Rheumatol, 2013,25(5):658-664.
doi: 10.1097/BOR.0b013e328363eb08 |
| [13] |
Maria FG, Mario D, Carmela G, et al. Chronic recurrent multifocal osteomyelitis: a case report[J]. Ital J Pediatr, 2018,44(1):26.
pmid: 29454377 |
| [14] |
Wipff J, Adamsbaum C, Kahan A, et al. Chronic recurrent multifocal osteomyelitis. Joint Bone Spine[J]. Joint Bone Spine Revue Du Rhumatisme, 2011,78(6):555-560.
doi: 10.1016/j.jbspin.2011.02.010 |
| [15] | Petty RE. Textbook of pediatric rheumatology[M]. 7th ed. Philadelphia: Elsevier, 2016: 406-417. |
| [16] |
von Kalle T, Heim N, Hospach T, et al. Typical pattern of bone involvement in whole-body MRI of patients with chronic recurrent multifocal osteomyelitis (CRMO)[J]. Rofo, 2013,185(7):655-661.
doi: 10.1055/s-0033-1335283 pmid: 23696017 |
| [17] | Ramraj R, Chun C, Marcovici P. Chronic Recurrent Multifocal Osteomyelitis in Crohn Disease: Complete Resolution With Anti-TNFα Therapy[J]. J Pediatr Gastrointestinal Nutr, 2018,67(3):e57. |
| [18] |
Roderick MR, Shah R, Rogers V, et al. Chronic recurrent multifocal osteomyelitis (CRMO): advancing the diagnosis[J]. Pediatr Rheumatol Online J, 2016,14(1):47.
doi: 10.1186/s12969-016-0109-1 pmid: 27576444 |
| [19] |
Jansson AF, Müller TH, Gliera L, et al. Clinical score for nonbacterial osteitis in children and adults[J]. Arthritis Rheum, 2009,60(4):1152-1159.
doi: 10.1002/art.24402 pmid: 19333943 |
| [20] |
Bousvaros A, Marcon M, Treem W, et al. Chronic recurrent multifocal osteomyelitis associated with chronic inflammatory bowel disease in children[J]. Dig Dis Sci, 1999,44(12):2500-2507.
pmid: 10630504 |
| [21] |
Wipff J, Costantino F, Lemelle I, et al. A large national cohort of French patients with chronic recurrent multifocal osteitis[J]. Arthritis Rheumatol, 2015,67(4):1128-1137.
doi: 10.1002/art.39013 pmid: 25545761 |
| [22] | 赵梦珠, 余可宜, 沈敏, 等. 慢性无菌性骨髓炎8例及文献复习[J]. 中华临床免疫和变态反应杂志, 2019,4(13):118-124. |
| [23] |
Zhao Y, Wu EY, Oliver MS, et al. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions[J]. Arthritis Care Res (Hoboken), 2018,70(8):1228-1237.
doi: 10.1002/acr.2018.70.issue-8 |
| No related articles found! |
|
||