北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 698-705. doi: 10.19723/j.issn.1671-167X.2019.04.018
女性膀胱癌患者腹腔镜膀胱全切术与开放膀胱全切术的倾向性评分匹配比较
黄海文1,闫兵2,尚美霞3,刘漓波1,郝瀚1,席志军1,△( )
)
- 1. 北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿、男性生殖系肿瘤研究中心,北京 100034
2. 邢台市人民医院泌尿外科,河北邢台 054001
3. 北京大学第一医院医学统计室,北京 100034
Propensity-matched comparison of laparoscopic and open radical cystectomy for female patients with bladder cancer
Hai-wen HUANG1,Bing YAN2,Mei-xia SHANG3,Li-bo LIU1,Han HAO1,Zhi-jun XI1,△( )
)
- 1.Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center, Beijing 100034, China
2. Department of Urology, Xingtai People’s Hospital, Xingtai 054001, Hebei, China
3. Department of Medical Statistics, Peking University First Hospital, Beijing 100034, China
摘要:
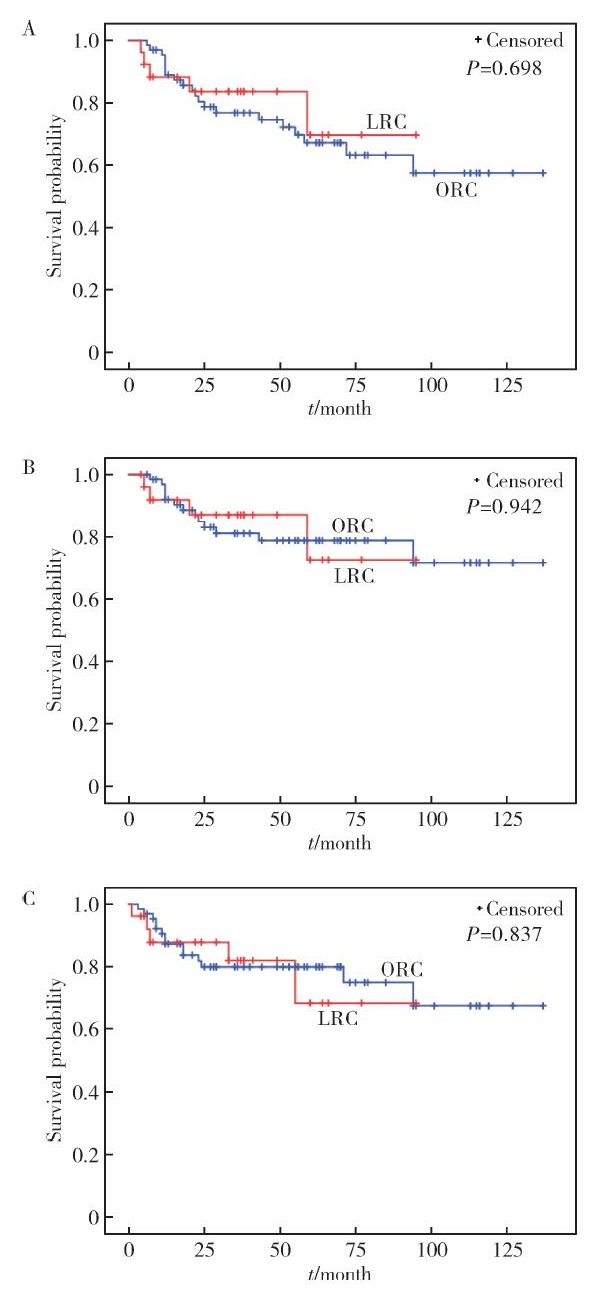
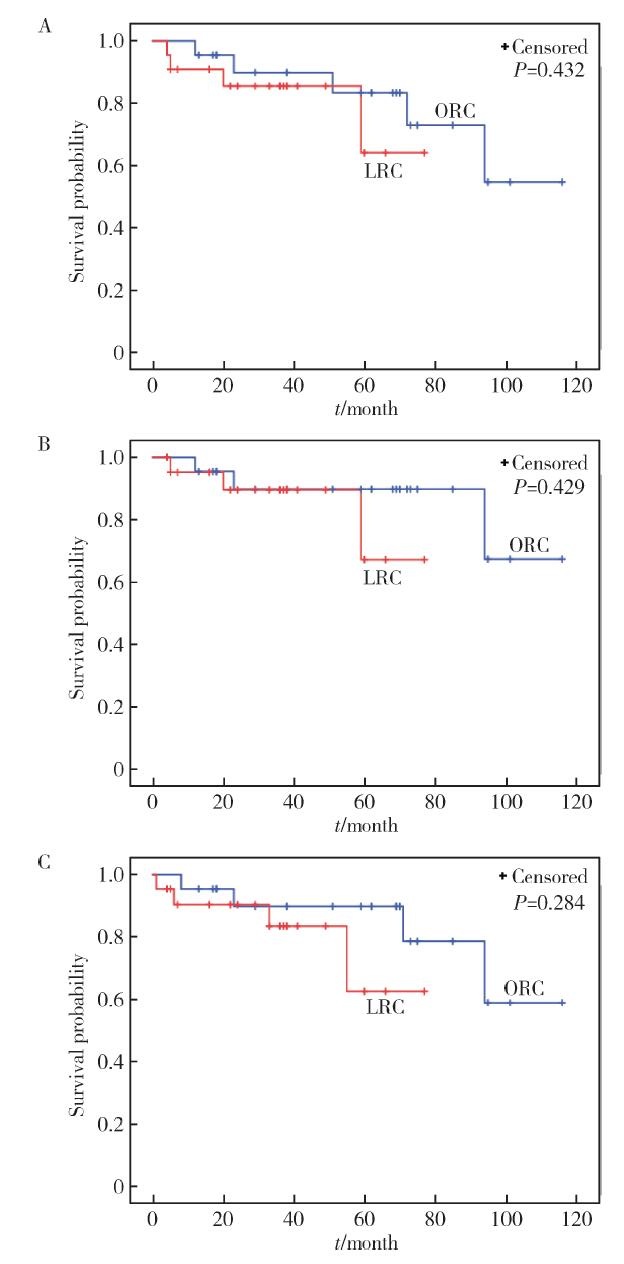
目的:比较女性膀胱癌患者腹腔镜膀胱全切术和开放膀胱全切术两种术式的围手术及肿瘤学预后差异。方法:回顾性分析2006—2017年于北京大学第一医院泌尿外科行根治性膀胱全切术的女性膀胱癌患者91例,将腹腔镜膀胱全切患者以1 :1的比例运用倾向性评分匹配(propensity score matching,PSM)方法与开放膀胱全切患者进行匹配,匹配因素包括年龄、体重指数(body mass index,BMI)、美国麻醉医师协会(American Society of Anesthesio-logists,ASA)评分、T分期及N分期,比较匹配前后两组患者的围手术及肿瘤学特征,应用Kaplan-Meier法比较匹配前后两组间总生存时间(overall survival,OS)、肿瘤特异生存时间(cancer specific survival,CSS)、无进展生存时间(progression free survival,PFS)。采用COX多因素回归分析校正匹配因素,进行敏感性分析。结果:共纳入行开放膀胱全切术患者65例,腹腔镜膀胱全切患者26例,中位随访时间为38个月(四分位距1869个月)。与开放膀胱全切组相比,腹腔镜膀胱全切组患者年龄更小(P<0.001),术前ASA评分更低(P=0.018),匹配后,22例开放膀胱全切患者与腹腔镜膀胱全切患者匹配成功。匹配前,腹腔镜膀胱全切组术中失血量更少(P=0.005),术中输血率更低(P<0.001),清扫淋巴结数目更多(P=0.035),围手术期并发症发生率较低(P=0.015),两组间OS(P=0.698)、CSS(P=0.942)、PFS(P=0.837)差异无统计学意义;匹配后,腹腔镜膀胱全切组术中失血量仍较开放膀胱全切组更少(P=0.009),术中输血率更低(P=0.001),围手术期并发症发生率较低(P=0.040),但清扫淋巴结数目两组间差异无统计学意义,两组间OS(P=0.432)、CSS(P=0.429)、PFS(P=0.284)差异亦无统计学意义。COX多因素回归分析显示,手术方式并不是女性膀胱癌患者OS(HR 1.134, 95%CI 0.335~3.835,P=0.839)、CSS(HR 1.051,95%CI 0.234~4.719,P=0.949)、PFS(HR 0.538,95%CI 0.138~2.095,P=0.371)的独立预测因子。结论:腹腔镜膀胱全切术术中出血量少、术中输血率低、围术期并发症少,但本研究并无证据表明女性膀胱癌患者接受腹腔镜膀胱全切术的预后优于开放膀胱全切术。
中图分类号:
- R737.14
| [1] | Antoni S, Ferlay J, Soerjomataram I , et al. Bladder cancer incidence and mortality: A global overview and recent trends[J]. Eur Urol, 2017,71(1):96-108. |
| [2] | Pang C, Guan Y, Li H , et al. Urologic cancer in China[J]. Jpn J Clin Oncol, 2016,46(6):497-501. |
| [3] | Tang K, Li H, Xia D , et al. Laparoscopic versus open radical cystectomy in bladder cancer: A systematic review and meta-analysis of comparative studies[J]. PLoS One, 2014,9(5):e95667. |
| [4] | Esquinas C, Alonso JM, Mateo E , et al. Prospective study comparing laparoscopic and open radical cystectomy: Surgical and oncological results[J]. Actas Urol Esp, 2018,42(2):94-102. |
| [5] | Guillotreau J, Game X, Mouzin M , et al. Radical cystectomy for bladder cancer: morbidity of laparoscopic versus open surgery[J]. J Urol, 2009,181(2):554-559. |
| [6] | Ha US, Kim SI, Kim SJ , et al. Laparoscopic versus open radical cystectomy for the management of bladder cancer: Mid-term oncological outcome[J]. Int J Urol, 2010,17(1):55-61. |
| [7] | Haber GP, Crouzet S, Gill IS . Laparoscopic and robotic assisted radical cystectomy for bladder cancer: A critical analysis[J]. Eur Urol, 2008,54(1):54-62. |
| [8] | Hemal AK, Kolla SB . Comparison of laparoscopic and open radical cystoprostatectomy for localized bladder cancer with 3-year oncological followup: a single surgeon experience[J]. J Urol, 2007,178(6):2340-2343. |
| [9] | Porpiglia F, Renard J, Billia M , et al. Open versus laparoscopy-assisted radical cystectomy: Results of a prospective study[J]. J Endourol, 2007,21(3):325-329. |
| [10] | Wang SZ, Chen LW, Zhang YH , et al. Comparison of hand-assisted laparoscopic and open radical cystectomy for bladder can-cer[J]. Urol Int, 2010,84(1):28-33. |
| [11] | Lin T, Fan X, Zhang C , et al. A prospective randomised controlled trial of laparoscopic vs. open radical cystectomy for bladder cancer: perioperative and oncologic outcomes with 5-year follow-up T Lin et al[J]. Br J Cancer, 2014,110(4):842-849. |
| [12] | Dobruch J, Daneshmand S, Fisch M , et al. Gender and bladder cancer: a collaborative review of etiology, biology, and outcomes[J]. Eur Urol, 2016,69(2):300-310. |
| [13] | Stenzl A . Cystectomy: technical considerations in male and female patients[J]. EAU Update Series, 2005,3(3):138-146. |
| [14] |
孟一森, 王宇, 范宇 , 等. 根治性膀胱全切手术及尿流改道方式对高龄患者围手术期并发症的影响[J]. 北京大学学报(医学版), 2016,48(4):632-637.
doi: 10.3969/j.issn.1671-167X.2016.04.013 |
| [15] | Shabsigh A, Korets R, Vora KC , et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology[J]. Eur Urol, 2009,55(1):164-174. |
| [16] | Stein JP, Lieskovsky G, Cote R , et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1 054 patients[J]. J Clin Oncol, 2001,19(3):666-675. |
| [17] | Studer UE, Burkhard FC, Schumacher M , et al. Twenty years experience with an ileal orthotopic low pressure bladder substitute: lessons to be learned[J]. J Urol, 2006,176(1):161-166. |
| [18] | Parra RO, Andrus CH, Jones JP , et al. Laparoscopic cystectomy: initial report on a new treatment for the retained bladder[J]. J Urol, 1992,148(4):1140-1144. |
| [19] | Aboumarzouk OM, Hughes O, Narahari K , et al. Safety and feasibility of laparoscopic radical cystectomy for the treatment of bladder cancer[J]. J Endourol, 2013,27(9):1083-1095. |
| [20] | Biondi-Zoccai G, Romagnoli E, Agostoni P , et al. Are propensity scores really superior to standard multivariable analysis?[J]. Contemp Clin Trials, 2011,32(5):731-740. |
| [21] | 焦明旭, 张晓, 刘迪 , 等. 倾向性评分匹配在非随机对照研究中的应用[J]. 中国卫生统计, 2016,33(2):350-352. |
| [22] | 王永吉, 蔡宏伟, 夏结来 , 等. 倾向指数匹配法与Logistic回归分析方法对比研究[J]. 现代预防医学, 2011,38(12):2217-2219. |
| [23] | Challacombe BJ, Bochner BH, Dasgupta P , et al. The role of laparoscopic and robotic cystectomy in the management of muscle-invasive bladder cancer with special emphasis on cancer control and complications[J]. Eur Urol, 2011,60(4):767-775. |
| [24] | Rios GE, Lopez-Tello GJ, Martinez-Pineiro LL . Laparoscopic radical cystectomy[J]. Clin Transl Oncol, 2009,11(12):799-804. |
| [25] | Chade DC, Laudone VP, Bochner BH , et al. Oncological outcomes after radical cystectomy for bladder cancer: open versus minimally invasive approaches[J]. J Urol, 2010,183(3):862-869. |
| [26] | Liedberg F, Mansson W . Lymph node metastasis in bladder cancer[J]. Eur Urol, 2006,49(1):13-21. |
| [27] | Dotan ZA, Kavanagh K, Yossepowitch O , et al. Positive surgical margins in soft tissue following radical cystectomy for bladder cancer and cancer specific survival[J]. J Urol, 2007,178(6):2308-2312. |
| [28] | Hadjizacharia P, Stein JP, Cai J , et al. The impact of positive soft tissue surgical margins following radical cystectomy for high-grade, invasive bladder cancer[J]. World J Urol, 2009,27(1):33-38. |
| [1] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [2] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [3] | 刘慧丽,吕彦函,王晓晓,李民. 老年患者腹腔镜泌尿系肿瘤根治术后慢性疼痛的影响因素[J]. 北京大学学报(医学版), 2023, 55(5): 851-856. |
| [4] | 王晓伟,穆英超,郭振宇,周玉博,张勇,李宏田,刘建蒙. 中国山东某县1951年以来出生女性初潮年龄与绝经年龄长期趋势[J]. 北京大学学报(医学版), 2023, 55(3): 502-510. |
| [5] | 张铃福,侯纯升,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 腹腔镜下经胆囊管胆管引流联合胆总管探查取石术治疗复杂胆管结石的临床效果[J]. 北京大学学报(医学版), 2022, 54(6): 1185-1189. |
| [6] | 王飞,秦彩朋,杜依青,刘士军,李清,徐涛. 中危非肌层浸润性膀胱癌的最佳膀胱镜监测强度[J]. 北京大学学报(医学版), 2022, 54(4): 669-673. |
| [7] | 安立哲,熊六林,陈亮,王焕瑞,陈伟男,黄晓波. 腹腔镜肾盂成形术联合肾盂镜超声碎石取石术治疗肾盂输尿管连接部梗阻合并肾结石[J]. 北京大学学报(医学版), 2022, 54(4): 746-750. |
| [8] | 邢云飞,刘春毅,孟文颖,张杰,焦明远,金蕾,靳蕾. 围受孕期服用微量营养增补剂与孕早期血清维生素E浓度的关系[J]. 北京大学学报(医学版), 2022, 54(3): 434-442. |
| [9] | 张帆,陈曲,郝一昌,颜野,刘承,黄毅,马潞林. 术前及术后膜性尿道长度与腹腔镜根治性前列腺切除术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2022, 54(2): 299-303. |
| [10] | 张帆,黄晓娟,杨斌,颜野,刘承,张树栋,黄毅,马潞林. 前列腺尖部深度与腹腔镜前列腺癌根治术后早期控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2021, 53(4): 692-696. |
| [11] | 董文敏,王明瑞,胡浩,王起,许克新,徐涛. Allium覆膜金属输尿管支架长期留置治疗输尿管-回肠吻合口狭窄的初期临床经验及随访结果[J]. 北京大学学报(医学版), 2020, 52(4): 637-641. |
| [12] | 朱洁,李建红,袁婷婷,和璐,梁宇红. 绝经期妇女牙周状况与骨质密度的相关性分析[J]. 北京大学学报(医学版), 2019, 51(6): 1115-1118. |
| [13] | 杨飞龙,洪锴,赵国江,刘承,宋一萌,马潞林. 基于长链非编码RNA的生物信息学分析构建膀胱癌预后模型并确定预后生物标志物[J]. 北京大学学报(医学版), 2019, 51(4): 615-622. |
| [14] | 赵海岳,叶雄俊,陈伟男,安立哲,刘军,熊六林,黄晓波. 腹腔镜肾盂成型术中异位血管的处理方法[J]. 北京大学学报(医学版), 2019, 51(4): 660-664. |
| [15] | 张铃福,侯纯升,黄永辉,徐智,王立新,凌晓锋,王港,崔龙,修典荣. 胃空肠吻合术后胆总管结石腹腔镜手术取石和内镜取石的比较[J]. 北京大学学报(医学版), 2019, 51(2): 345-348. |
|
||