1 资料与方法
1.1 研究对象
1.2 研究方法
1.3 统计学分析
2 结果
2.1 一般情况
表1 COPD患者的基线特征分布Table 1 Baseline characteristics of COPD participants by level of total physical activity |
| Characteristic | Quintiles of total physical activity | F/χ2 | P | ||||
| Q1 (n=6 774) | Q2 (n=6 668) | Q3 (n=6 731) | Q4 (n=6 698) | Q5 (n=6 717) | |||
| Age/years,${\bar x}$±s | 64.4±8.8 | 61.6±9.7 | 58.1±10.5 | 55.0±10.3 | 52.0±9.5 | 1 746.7 | < 0.001 |
| Gender, n (%) | 1 155.9 | < 0.001 | |||||
| Female | 2 405 (35.5) | 4 174 (62.6) | 3 655 (54.3) | 3 697 (55.2) | 3 009 (44.8) | ||
| Male | 4 369 (64.5) | 2 494 (37.4) | 3 076 (45.7) | 3 001 (44.8) | 3 708 (55.2) | ||
| Area, n (%) | 538.2 | < 0.001 | |||||
| Urban | 3 069 (45.3) | 2 714 (40.7) | 2 275 (33.8) | 1 842 (27.5) | 2 317 (34.5) | ||
| Rural | 3 705 (54.7) | 3 954 (59.3) | 4 456 (66.2) | 4 856 (72.5) | 4 400 (65.5) | ||
| Married, n (%) | 19.44 | 0.001 | |||||
| Married | 5 731 (84.6) | 5 661 (84.9) | 5 829 (86.6) | 5 800 (86.6) | 5 803 (86.4) | ||
| Other | 1 043 (15.4) | 1 007 (15.1) | 902 (13.4) | 898 (13.4) | 914 (13.6) | ||
| Education, n (%) | 86.72 | < 0.001 | |||||
| Middle school and higher | 2 249 (33.2) | 2 174 (32.6) | 2 214 (32.9) | 2 043 (30.5) | 1 840 (27.4) | ||
| Primary school and lower | 4 525 (66.8) | 4 494 (67.4) | 4 517 (67.1) | 4 655 (69.5) | 4 877 (72.6) | ||
| Household income, n (%) | 55.75 | < 0.001 | |||||
| ≥20 000 yuan/year | 2 113 (31.2) | 2 274 (34.1) | 2 430 (36.1) | 2 197 (32.8) | 2 230 (33.2) | ||
| < 20 000 yuan/year | 4 661 (68.8) | 4 394 (65.9) | 4 301 (63.9) | 4 501 (67.2) | 4 487 (66.8) | ||
| Occupation, n (%) | 3 949.37 | < 0.001 | |||||
| Agriculture and industrial | 2 174 (32.1) | 2 634 (39.5) | 4 146 (61.6) | 4 930 (73.6) | 5 145 (76.6) | ||
| Other occupation | 4 600 (67.9) | 4 034 (60.5) | 2 585 (38.4) | 1 768 (26.4) | 1 572 (23.4) | ||
| Regular consumption of meat, n (%) | 31.86 | < 0.001 | |||||
| ≥4 d/week | 2 757 (40.7) | 2 674 (40.1) | 2 612 (38.8) | 2 451 (36.6) | 2 646 (39.4) | ||
| < 4 d/week | 4 017 (59.3) | 3 994 (59.9) | 4 119 (61.2) | 4 247 (63.4) | 4 071 (60.6) | ||
| Regular consumption of fresh vegetables, n (%) | 12.81 | 0.012 | |||||
| ≥4 d/week | 6 672 (98.5) | 6 588 (98.8) | 6 643 (98.7) | 6 571 (98.1) | 6 616 (98.5) | ||
| < 4 d/week | 102 (1.5) | 80 (1.2) | 88 (1.3) | 127 (1.9) | 101 (1.5) | ||
| Regular consumption of fresh fruit, n (%) | 104.56 | < 0.001 | |||||
| ≥4 d/week | 1 531 (22.6) | 1 607 (24.1) | 1 602 (23.8) | 1 326 (19.8) | 1 209 (18.0) | ||
| < 4 d/week | 5 243 (77.4) | 5 061 (75.9) | 5 129 (76.2) | 5 372 (80.2) | 5 508 (82.0) | ||
| Drinking status, n (%) | 52.19 | < 0.001 | |||||
| Current weekly drinker | 2 683 (39.6) | 2 627 (39.4) | 2 706 (40.2) | 2 693 (40.2) | 2 821 (42.0) | ||
| Non-current weekly drinker | 4 091 (60.4) | 4 041 (60.6) | 4 025 (59.8) | 4 005 (59.8) | 3 896 (58.0) | ||
| Smoking status, n (%) | 18.58 | 0.001 | |||||
| Current daily smoker | 1 009 (14.9) | 1 014 (15.2) | 1 198 (17.8) | 1 192 (17.8) | 1 243 (18.5) | ||
| Non-current smoker | 5 765 (85.1) | 5 654 (84.8) | 5 533 (82.2) | 5 506 (82.2) | 5 474 (81.5) | ||
| BMI/(kg/m2),${\bar x}$±s | 22.8±3.8 | 22.8±3.7 | 22.8±3.5 | 22.5±3.4 | 22.5±3.2 | 10.65 | < 0.001 |
| Sedentary/ (h/d),${\bar x}$±s | 3.5±2.0 | 3.5±1.8 | 3.1±1.6 | 2.7±1.5 | 2.5±1.4 | 390.75 | < 0.001 |
| GOLD, n (%) | 456.27 | < 0.001 | |||||
| 1 | 1 687 (24.9) | 1 840 (27.6) | 2 006 (29.8) | 1 942 (29.0) | 2 042 (30.4) | ||
| 2 | 3 184 (47.0) | 3 194 (47.9) | 3 150 (46.8) | 3 275 (48.9) | 3 379 (50.3) | ||
| 3 | 1 429 (21.1) | 1 300 (19.5) | 1 292 (19.2) | 1 233 (18.4) | 1 101 (16.4) | ||
| 4 | 474 (7.0) | 334 (5.0) | 283 (4.2) | 248 (3.7) | 195 (2.9) | ||
| Self-assessed health status, n (%) | 362.41 | < 0.001 | |||||
| Excellent | 644 (9.5) | 785 (11.8) | 828 (12.3) | 824 (12.3) | 804 (11.9) | ||
| Good | 1 361 (20.1) | 1 426 (21.4) | 1 615 (24.0) | 1 567 (23.4) | 1 798 (26.8) | ||
| Average | 2 994 (44.2) | 3 065 (45.9) | 3 110 (46.2) | 3 182 (47.5) | 3 054 (45.5) | ||
| Poor | 1 775 (26.2) | 1 392 (20.9) | 1 178 (17.5) | 1 125 (16.8) | 1 061 (15.8) | ||
| Coronary heart disease, n (%) | 46.98 | < 0.001 | |||||
| Yes | 318 (4.7) | 280 (4.2) | 269 (4.0) | 174 (2.6) | 154 (2.3) | ||
| No | 6 456 (95.3) | 6 388 (95.8) | 6 462 (96.0) | 6 524 (97.4) | 6 563 (97.7) | ||
| Diabetes, n (%) | 62.14 | < 0.001 | |||||
| Yes | 271 (4.0) | 240 (3.6) | 168 (2.5) | 147 (2.2) | 114 (1.7) | ||
| No | 6 503 (96.0) | 6 428 (96.4) | 6 563 (97.5) | 6 551 (97.8) | 6 603 (98.3) | ||
| Kidney disease, n (%) | 14.35 | 0.006 | |||||
| Yes | 163 (2.4) | 120 (1.8) | 108 (1.6) | 127 (1.9) | 101 (1.5) | ||
| No | 6 611 (97.6) | 6 548 (98.2) | 6 623 (98.4) | 6 571 (98.1) | 6 616 (98.5) | ||
| Stroke, n (%) | 101.74 | < 0.001 | |||||
| Yes | 217 (3.2) | 133 (2.0) | 94 (1.4) | 60 (0.9) | 60 (0.9) | ||
| No | 6 557 (96.8) | 6 535 (98.0) | 6 637 (98.6) | 6 638 (99.1) | 6 657 (99.1) | ||
Total physical activity was divided into 5 parts according to quintiles, and the boundaries are 0.2-, 8.0-, 12.2-, 19.1-, 30.3-108.2 MET-hours/day; Results were standardized by age, sex, and region (where appropriate). COPD, chronic obstructive pulmonary disease; BMI, body mass index; GOLD, Global Initiative for Chronic Obstructive Lung Disease; MET, metabolic equivalent of the task. |
2.2 总体力活动与死亡风险的关联
表2 COPD患者中总体力活动与死亡风险的关联Table 2 Associations of total physical activity with mortality risk in COPD patients |
| Quintiles of total physical activity | P | |||||
| Q1 | Q2 | Q3 | Q4 | Q5 | ||
| All-cause mortality | ||||||
| Number of deaths, n | 2 764 | 1 955 | 1 558 | 1 195 | 842 | |
| Mortality rate/% | 40.4 | 26.8 | 20.5 | 15.5 | 10.6 | |
| Model 1, HR(95%CI) | 1.00 | 0.83 (0.78, 0.88) | 0.76 (0.70, 0.81) | 0.69 (0.63, 0.74) | 0.63 (0.58, 0.69) | < 0.001 |
| Model 2, HR(95%CI) | 1.00 | 0.90 (0.84, 0.95) | 0.85 (0.79, 0.91) | 0.78 (0.72, 0.85) | 0.77 (0.70, 0.85) | < 0.001 |
| Vascular disease mortality | ||||||
| Number of deaths, n | 1 069 | 749 | 506 | 372 | 244 | |
| Mortality rate/% | 15.6 | 10.3 | 6.7 | 4.8 | 3.1 | |
| Model 1, HR(95%CI) | 1.00 | 0.81 (0.74, 0.89) | 0.75 (0.66, 0.84) | 0.73 (0.63, 0.84) | 0.66 (0.56, 0.77) | < 0.001 |
| Model 2, HR(95%CI) | 1.00 | 0.88 (0.80, 0.97) | 0.83 (0.73, 0.93) | 0.82 (0.71, 0.94) | 0.77 (0.65, 0.91) | 0.002 |
| Malignant tumor mortality | ||||||
| Number of deaths, n | 619 | 470 | 383 | 327 | 287 | |
| Mortality rate/% | 9.1 | 6.4 | 5.1 | 4.2 | 3.6 | |
| Model 1, HR(95%CI) | 1.00 | 1.01 (0.90, 1.15) | 0.91 (0.79, 1.05) | 0.88 (0.75, 1.03) | 0.88 (0.74, 1.04) | 0.105 |
| Model 2, HR(95%CI) | 1.00 | 1.03 (0.91, 1.16) | 0.94 (0.82, 1.09) | 0.91 (0.77, 1.08) | 0.92 (0.78, 1.10) | 0.293 |
| Respiratory disease mortality | ||||||
| Number of deaths, n | 702 | 493 | 427 | 288 | 165 | |
| Mortality rate/% | 10.3 | 6.8 | 5.6 | 3.7 | 2.1 | |
| Model 1, HR(95%CI) | 1.00 | 0.74 (0.66, 0.83) | 0.61 (0.53, 0.70) | 0.45 (0.38, 0.53) | 0.37 (0.31, 0.46) | < 0.001 |
| Model 2, HR(95%CI) | 1.00 | 0.86 (0.76, 0.97) | 0.76 (0.66, 0.87) | 0.58 (0.49, 0.69) | 0.58 (0.48, 0.71) | < 0.001 |
Total physical activity was divided into 5 parts according to quintiles, and the boundaries are 0.2-, 8.0-, 12.2-, 19.1-, 30.3-108.2 MET-hours/day; Model 1 was adjusted for education levels, income levels, occupation categories and marriage status; Model 2 was additionally adjusted for smoking, alcohol intake, dietary habits (frequency of meat, fresh vegetable, and fruit consumption), sedentary time(hours/day), BMI, self-assessed health status, GOLD levels, coronary heart disease, diabetes, kidney disease, stroke; The denominator of the mortality rate was 1 000 person-years. COPD, chronic obstructive pulmonary disease; MET, metabolic equivalent of the task; BMI, body mass index; GOLD, Global Initiative for Chronic Obstructive Lung Disease. |
表3 COPD患者中总体力活动与全因死亡风险的亚组分析Table 3 Subgroup analysis for the associations of total physical activity with all-cause mortality risk in COPD patients |
| Quintiles of total physical activity | P(LR χ2) | |||||
| Q1 | Q2 | Q3 | Q4 | Q5 | ||
| Age group/years | 0.028 (7.12) | |||||
| 30- | 1.00 | 1.19 (0.76, 1.86) | 1.06 (0.68, 1.65) | 1.02 (0.66, 1.59) | 1.15 (0.75, 1.77) | |
| 50- | 1.00 | 0.88 (0.73, 1.06) | 0.86 (0.71, 1.04) | 0.81 (0.67, 0.99) | 0.81 (0.66, 0.99) | |
| 60- | 1.00 | 0.90 (0.84, 0.96) | 0.85 (0.79, 0.92) | 0.79 (0.72, 0.87) | 0.77 (0.68, 0.86) | |
| Area | 0.125 (2.35) | |||||
| Rural | 1.00 | 0.89 (0.83, 0.96) | 0.85 (0.78, 0.92) | 0.79 (0.72, 0.86) | 0.75 (0.68, 0.83) | |
| Urban | 1.00 | 0.93 (0.84, 1.04) | 0.88 (0.77, 1.01) | 0.80 (0.65, 0.97) | 0.86 (0.70, 1.06) | |
| Gender | 0.012 (6.24) | |||||
| Male | 1.00 | 0.90 (0.83, 0.97) | 0.90 (0.82, 0.98) | 0.83 (0.75, 0.92) | 0.81 (0.73, 0.91) | |
| Female | 1.00 | 0.86 (0.78, 0.95) | 0.77 (0.68, 0.87) | 0.67 (0.58, 0.77) | 0.64 (0.53, 0.76) | |
| Smoking status | 0.109 (2.57) | |||||
| Non-current smoker | 1.00 | 0.91 (0.83, 0.99) | 0.82 (0.74, 0.92) | 0.76 (0.67, 0.86) | 0.71 (0.61, 0.82) | |
| Current daily smoker | 1.00 | 0.88 (0.81, 0.96) | 0.86 (0.78, 0.95) | 0.79 (0.71, 0.88) | 0.79 (0.70, 0.89) | |
| Drinking status | 0.004 (8.12) | |||||
| Non-current weekly drinker | 1.00 | 0.92 (0.86, 0.98) | 0.86 (0.80, 0.93) | 0.78 (0.71, 0.85) | 0.77 (0.69, 0.86) | |
| Current weekly drinker | 1.00 | 0.74 (0.62, 0.87) | 0.75 (0.63, 0.89) | 0.74 (0.61, 0.89) | 0.71 (0.58, 0.87) | |
| Sedentary/(h/d) | 0.158 (1.99) | |||||
| < 3 | 1.00 | 0.91 (0.82, 1.00) | 0.83 (0.75, 0.93) | 0.78 (0.68, 0.88) | 0.75 (0.66, 0.86) | |
| ≥3 | 1.00 | 0.88 (0.81, 0.95) | 0.85 (0.77, 0.93) | 0.78 (0.70, 0.87) | 0.78 (0.68, 0.89) | |
| GOLD | 0.016 (8.32) | |||||
| 1 | 1.00 | 0.92 (0.78, 1.09) | 0.84 (0.69, 1.03) | 0.76 (0.60, 0.95) | 0.76 (0.60, 0.97) | |
| 2 | 1.00 | 0.95 (0.87, 1.04) | 0.95 (0.85, 1.06) | 0.91 (0.81, 1.04) | 0.87 (0.76, 1.00) | |
| 3-4 | 1.00 | 0.82 (0.75, 0.90) | 0.74 (0.66, 0.82) | 0.66 (0.58, 0.74) | 0.64 (0.55, 0.75) | |
| BMI/(kg/m2) | 0.003 (14.30) | |||||
| Underweight | 1.00 | 0.86 (0.75, 0.99) | 0.78 (0.66, 0.92) | 0.64 (0.53, 0.78) | 0.57 (0.45, 0.71) | |
| Normal weight | 1.00 | 0.88 (0.81, 0.95) | 0.80 (0.73, 0.89) | 0.73 (0.65, 0.81) | 0.71 (0.63, 0.80) | |
| Overweight | 1.00 | 0.86 (0.75, 0.98) | 0.81 (0.69, 0.96) | 0.91 (0.75, 1.11) | 0.77 (0.61, 0.96) | |
| Obese | 1.00 | 1.02 (0.78, 1.33) | 1.08 (0.81, 1.44) | 0.60 (0.39, 0.91) | 0.80 (0.49, 1.32) | |
| Self-assessed health status | 0.010 (11.34) | |||||
| Excellent | 1.00 | 0.99 (0.78, 1.24) | 0.91 (0.69, 1.20) | 0.90 (0.65, 1.23) | 0.95 (0.68, 1.33) | |
| Good | 1.00 | 0.87 (0.75, 1.02) | 0.82 (0.69, 0.98) | 0.78 (0.64, 0.95) | 0.70 (0.57, 0.86) | |
| Average | 1.00 | 0.87 (0.80, 0.95) | 0.87 (0.78, 0.96) | 0.78 (0.69, 0.88) | 0.73 (0.63, 0.84) | |
| Poor | 1.00 | 0.85 (0.76, 0.95) | 0.71 (0.62, 0.81) | 0.61 (0.53, 0.71) | 0.58 (0.48, 0.71) | |
Total physical activity was divided into 5 parts according to quintiles, and the boundaries are 0.2-, 8.0-, 12.2-, 19.1-, 30.3-108.2 MET-hours/day; Results are presented as HR (95%CI) and based on model 2; P values for interaction were calculated by likelihood ratio test, comparing models with and without cross-product terms between the stratification variables and total physical activity;Given the small number of participants with GOLD level 4, the GOLD 3 and GOLD 4 were combined into one group for the subgroup analysis. COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; BMI, body mass index; MET, metabolic equivalent of the task. |
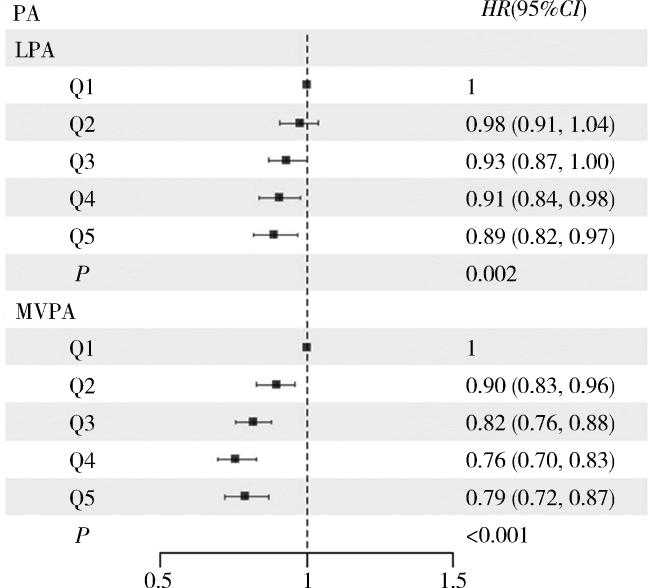
2.3 不同强度体力活动与死亡风险的关联
图1 COPD患者不同强度体力活动与全因死亡风险的关联Figure 1 Associations between different intensities of physical activity and all-cause mortality risk in COPD patients LPA was divided into 5 parts according to quintiles, and the boundaries are 0-, 2.8-, 6.0-, 8.6-, 12.9-42.67 MET-hours/day; MVPA was divided into 5 parts according to quintiles, and the boundaries are 0-, 0.1-, 2.9-, 6.6-, 21.1-101.9 MET-hours/day; results are presented as HR (95%CI) and based on model 2. PA, physical activity; LPA low-level physical activity; MVPA moderate-to-vigorous-level physical activity; MET, metabolic equivalent of the task; COPD, chronic obstructive pulmonary disease. |
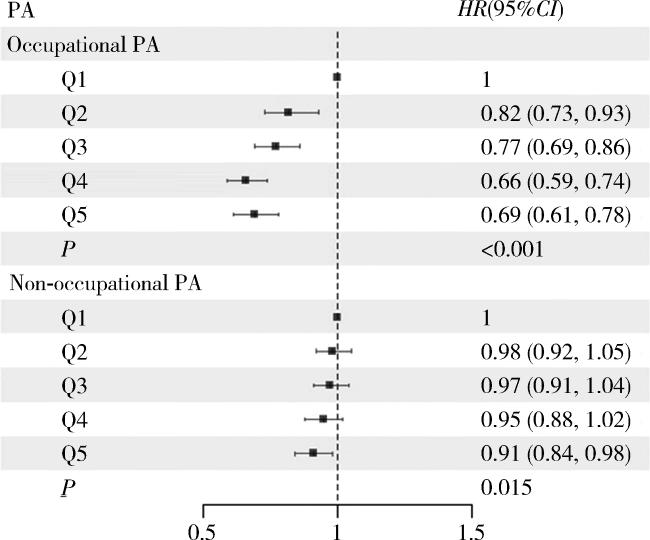
2.4 不同类型体力活动与死亡风险的关联
图2 COPD患者不同类型体力活动与全因死亡风险的关联Figure 2 Associations between different types of physical activity and all-cause mortality risk in COPD patients Occupational PA was divided into 5 parts according to quintiles, and the boundaries are 0-, 0.3-, 2.3-, 10.7-, 21.7-100 MET-hours/day; Non-occupational PA was divided into 5 parts according to quintiles, and the boundaries are 0-, 3.7-, 6.2-, 8.4-, 11.2-58.97 MET-hours/day; results are presented as HR (95%CI) and based on model 2. PA physical activity; MET, metabolic equivalent of the task; COPD, chronic obstructive pulmonary disease. |